Alcohol (drug)
 | |||
| |||
| Clinical data | |||
|---|---|---|---|
| Pronunciation | /ˈɛθənɒl/ | ||
| Other names | Absolute alcohol; Alcohol (USP); Cologne spirit; Drinking alcohol; Ethanol (JAN); Ethylic alcohol; EtOH; Ethyl alcohol; Ethyl hydrate; Ethyl hydroxide; Ethylol; Grain alcohol; Hydroxyethane; Methylcarbinol | ||
| Pregnancy category |
| ||
| Dependence liability | Physical: Very High Psychological: Moderate[1] | ||
| Addiction liability | Moderate (10–15%)[2] | ||
| Routes of administration | Common: By mouth Uncommon: Suppository, inhalation, ophthalmic, insufflation, injection[3] | ||
| Drug class | Depressant; Anxiolytic; Analgesic; Euphoriant; Sedative; Emetic; Diuretic; General anesthetic | ||
| ATC code | |||
| Legal status | |||
| Legal status |
| ||
| Pharmacokinetic data | |||
| Bioavailability | 80%+[4][5] | ||
| Protein binding | Weakly or not at all[4][5] | ||
| Metabolism | Liver (90%):[6][8] • Alcohol dehydrogenase • MEOS (CYP2E1) | ||
| Metabolites | Acetaldehyde; Acetic acid; Acetyl-CoA; Carbon dioxide; Ethyl glucuronide; Ethyl sulfate; Water | ||
| Onset of action | Peak concentrations:[6][4] • Range: 30–90 minutes • Mean: 45–60 minutes • Fasting: 30 minutes | ||
| Elimination half-life | Constant-rate elimination at typical concentrations:[7][8][6] • Range: 10–34 mg/dL/hour • Mean (men): 15 mg/dL/hour • Mean (women): 18 mg/dL/hr At very high concentrations (t1/2): 4.0–4.5 hours[5][4] | ||
| Duration of action | 6–16 hours (amount of time that levels are detectable)[9] | ||
| Excretion | • Major: metabolism (into carbon dioxide and water)[4] • Minor: urine, breath, sweat (5–10%)[6][4] | ||
| Identifiers | |||
| |||
| CAS Number | |||
| PubChem CID | |||
| IUPHAR/BPS | |||
| DrugBank | |||
| ChemSpider | |||
| UNII | |||
| KEGG | |||
| ChEBI | |||
| ChEMBL | |||
| PDB ligand | |||
| Chemical and physical data | |||
| Formula | C2H6O | ||
| Molar mass | 46.069 g·mol−1 | ||
| 3D model (JSmol) | |||
| Density | 0.7893 g/cm3 (at 20 °C)[10] | ||
| Melting point | −114.14 ± 0.03 °C (−173.45 ± 0.05 °F) [10] | ||
| Boiling point | 78.24 ± 0.09 °C (172.83 ± 0.16 °F) [10] | ||
| Solubility in water | Miscible mg/mL (20 °C) | ||
| |||
| |||
Alcohol (from Arabic al-kuḥl 'the kohl'),[11] sometimes referred to by the chemical name ethanol, is the second most consumed psychoactive drug globally behind caffeine,[12] and alcohol use disorders are the most prevalent of all substance use disorders worldwide.[13] Alcohol is a central nervous system (CNS) depressant, decreasing electrical activity of neurons in the brain.[14] The World Health Organization (WHO) classifies alcohol as a toxic, psychoactive, dependence-producing, and carcinogenic substance.[15]
Alcohol is found in fermented beverages such as beer, wine, and distilled spirit[16] – in particular, rectified spirit,[17] and serves various purposes; Certain religions integrate alcohol into their spiritual practices. For example, the Catholic Church requires alcoholic sacramental wine in the Eucharist, and permits moderate consumption of alcohol in daily life as a means of experiencing joy.[18][19] Alcohol is also used as a recreational drug, for example by college students, for self-medication, and in warfare. It is also frequently involved in alcohol-related crimes such as drunk driving, public intoxication, and underage drinking.
Short-term effects from moderate consumption include relaxation, decreased social inhibition, and euphoria, while binge drinking may result in cognitive impairment, blackout, and hangover. Excessive alcohol intake causes alcohol poisoning, characterized by unconsciousness or, in severe cases, death. Long-term effects are considered to be a major global public health issue and includes alcoholism, abuse, alcohol withdrawal, fetal alcohol spectrum disorder (FASD), liver disease, hepatitis, cardiovascular disease (e.g., cardiomyopathy), polyneuropathy, alcoholic hallucinosis, long-term impact on the brain (e.g., brain damage, dementia, and Marchiafava–Bignami disease), and cancers.
For roughly two decades, the International Agency for Research on Cancer (IARC) of the WHO has classified alcohol as a Group 1 Carcinogen.[20] Globally, alcohol use was the seventh leading risk factor for both deaths and DALY in 2016.[21] According to WHO's Global status report on alcohol and health 2018, more than 200 health issues are associated with harmful alcohol consumption, ranging from liver diseases, road injuries and violence, to cancers, cardiovascular diseases, suicides, tuberculosis, and HIV/AIDS.[22] Moreover, a 2024 WHO report indicates that these harmful consequences of alcohol use result in approximately 2.6 million deaths annually, accounting for 4.7% of all global deaths.[23]
In 2023, the WHO declared that 'there is no safe amount of alcohol consumption' and that 'the risk to the drinker’s health starts from the first drop of any alcoholic beverage.'[15] National agencies are aligning with the WHO's recommendations and increasingly advocating for abstinence from alcohol consumption. They highlight that even minimal alcohol intake is associated with elevated health risks, emphasizing that reducing alcohol intake is beneficial for everyone, regardless of their current drinking levels.[24][25][26]
Uses
[edit]Dutch courage
[edit]
Dutch courage, also known as pot-valiance or liquid courage, refers to courage gained from intoxication with alcohol.
Alcohol use among college students is often used as "liquid courage" in the hookup culture, for them to make a sexual advance in the first place.[27]: 200 However, a recent trend called "dry dating" is gaining popularity to replace "liquid courage", which involves going on dates without consuming alcohol.[28][29][30]
Consuming alcohol prior to visiting female sex workers is a common practice among some men.[31] Sex workers often resort to using drugs and alcohol to cope with stress.[32]
Alcohol when consumed in high doses is considered to be an anaphrodisiac.[33]
Criminal
[edit]Albeit not a valid intoxication defense, weakening the inhibitions by drunkenness is occasionally used as a tool to commit planned offenses such as property crimes including theft and robbery, and violent crimes including assault, murder, or rape – which sometimes but not always occurs in alcohol-facilitated sexual assaults where the victim is also drugged.
Warfare
[edit]
Alcohol has a long association of military use, and has been called "liquid courage" for its role in preparing troops for battle, anaesthetize injured soldiers, and celebrate military victories. It has also served as a coping mechanism for combat stress reactions and a means of decompression from combat to everyday life. However, this reliance on alcohol can have negative consequences for physical and mental health.[34] Military and veteran populations face significant challenges in addressing the co-occurrence of PTSD and alcohol use disorder.[35] Military personnel who show symptoms of PTSD, major depressive disorder, alcohol use disorder, and generalized anxiety disorder show higher levels of suicidal ideation.[36]
Alcohol consumption in the US Military is higher than any other profession, according to CDC data from 2013–2017. The Department of Defense Survey of Health Related Behaviors among Active Duty Military Personnel published that 47% of active duty members engage in binge drinking, with another 20% engaging in heavy drinking in the past 30 days.
Reports from the Russian invasion of Ukraine in 2022 and since suggested that Russian soldiers are drinking significant amount of alcohol (as well as consuming harder drugs), which increases their losses. Some reports suggest that on occasion, alcohol and drugs have been provided to the lower quality troops by their commanders, in order to facilitate their use as expendable cannon fodder.[37][38][39][40]
Food energy
[edit]
The USDA uses a figure of 6.93 kilocalories (29.0 kJ) per gram of alcohol (5.47 kcal or 22.9 kJ per ml) for calculating food energy.[41] For distilled spirits, a standard serving in the United States is 44 ml (1.5 US fl oz), which at 40% ethanol (80 proof), would be 14 grams and 98 calories.
However, alcoholic drinks are considered empty calorie foods because other than food energy they contribute no essential nutrients. Alcohol increases insulin response to glucose promoting fat storage and hindering carb/fat burning oxidation.[42][43] This excess processing in the liver acetyl CoA can lead to fatty liver disease and eventually alcoholic liver disease. This progression can lead to further complications, alcohol-related liver disease may cause exocrine pancreatic insufficiency, the inability to properly digest food due to a lack or reduction of digestive enzymes made by the pancreas.[44]
The use of alcohol as a staple food source is considered inconvenient due to the fact that it increases the blood alcohol content (BAC). However, alcohol is a significant source of food energy for individuals with alcoholism and those who engage in binge drinking; For example, individuals with drunkorexia, engage in the combination of self-imposed malnutrition and binge drinking to avoid weight gain from alcohol, to save money for purchasing alcohol,[45] and to facilitate alcohol intoxication.[46] Also, in alcoholics who get most of their daily calories from alcohol, a deficiency of thiamine can produce Korsakoff's syndrome, which is associated with serious brain damage.[47]
Medical
[edit]Spiritus fortis is a medical term for ethanol solutions with 95% ABV.
When taken by mouth or injected into a vein ethanol is used to treat methanol or ethylene glycol toxicity[48] when fomepizole is not available.[49]
Ethanol, when used to treat or prevent methanol and/or ethylene glycol toxicity, competes with other alcohols for the alcohol dehydrogenase enzyme, lessening metabolism into toxic aldehyde and carboxylic acid derivatives, and reducing the more serious toxic effects of the glycols when crystallized in the kidneys.[50]
Recreational
[edit]Drinking culture is the set of traditions and social behaviors that surround the consumption of alcoholic beverages as a recreational drug and social lubricant. Although alcoholic beverages and social attitudes toward drinking vary around the world, nearly every civilization has independently discovered the processes of brewing beer, fermenting wine and distilling spirits.[51]
Common drinking styles include moderate drinking, social drinking, and binge drinking.
Drinking styles
[edit]
Source: SAMHSA[52]
In today's society, there is a growing awareness of this, reflected in the variety of approaches to alcohol use, each emphasizing responsible choices. Sober curious describes a mindset or approach where someone is consciously choosing to reduce or eliminate alcohol consumption, not drinking and driving, being aware of your surroundings, not pressuring others to drink, and being able to quit anytime. However, they are not necessarily committed to complete sobriety.
A 2014 report in the National Survey on Drug Use and Health found that only 10% of either "heavy drinkers" or "binge drinkers" defined according to the above criteria also met the criteria for alcohol dependence, while only 1.3% of non-binge drinkers met the criteria. An inference drawn from this study is that evidence-based policy strategies and clinical preventive services may effectively reduce binge drinking without requiring addiction treatment in most cases.[53]
Binge drinking
[edit]Binge drinking, or heavy episodic drinking, is drinking alcoholic beverages with an intention of becoming intoxicated by heavy consumption of alcohol over a short period of time, but definitions vary considerably.[54] Binge drinking is a style of drinking that is popular in several countries worldwide, and overlaps somewhat with social drinking since it is often done in groups.
Drinking games involve consuming alcohol as part of the gameplay. They can be risky because they can encourage people to drink more than they intended to. Recent studies link binge drinking habits to a decline in quality of life and a shortened lifespan by 3–6 years.[55][56]
Alcohol-based sugar-sweetened beverages, are closely linked to episodic drinking in adolescents.[57] Sugar-infused alcoholic beverages include alcopops, and liqueurs.
Pregame heavy episodic drinking (4+/5+ drinks for women/men) or more drinks is linked to a higher likelihood of engaging in high-intensity drinking (8+/10+ drinks), according to a 2022 study. The study also found that students who pregame at this level report more negative consequences compared to days with moderate pregame drinking and days without any pregame drinking.[58]
Hazing has a long-standing presence in college fraternities, often involving alcohol as a form of punishment. This can lead to dangerous levels of intoxication and severe ethanol poisoning, sometimes resulting in fatalities. High serum ethanol levels are common among affected students.[59]
Definition
[edit]Binge drinking refers to the consumption of alcohol that takes place simultaneously or within a few hours of one another;
- The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking as a pattern of alcohol consumption that brings a person's blood alcohol concentration (BAC) to 0.08 percent or above. This typically occurs when men consume five or more US standard drinks, or women consume four or more drinks, within about two hours.
- The Substance Abuse and Mental Health Services Administration (SAMHSA) defines binge drinking slightly differently, focusing on the number of drinks consumed on a single occasion. According to SAMHSA, binge drinking is consuming five or more drinks for men, or four or more drinks for women, on the same occasion on at least one day in the past month.[60]
Heavy drinking
[edit]
Alcohol in association football has long been a complex issue, with significant cultural and behavioral implications. Football is widely observed in various settings such as television broadcasts, sports bars, and arenas, contributing to the drinking culture surrounding the sport. A 2007 study at the University of Texas at Austin monitored the drinking habits of 541 students over two football seasons. It revealed that high-profile game days ranked among the heaviest drinking occasions, similar to New Year's Eve. Male students increased their consumption for all games, while socially active female students drank heavily during away games. Lighter drinkers also showed a higher likelihood of risky behaviors during away games as their intoxication increased. This research highlights specific drinking patterns linked to collegiate sports events.[61]
Heavy drinking significantly increases during December, particularly around Christmas and New Year's, leading to a rise in alcohol sales, consumption, and related harmful events and deaths.[62] Because of increased alcohol consumption at festivities and poorer road conditions during the winter months, alcohol-related road traffic accidents increase over the Christmas and holiday season.[63]
According to a 2022 study, recreational heavy drinking and intoxication have become increasingly prevalent among Nigerian youth in Benin City. Traditionally, alcohol use was more accepted for men, while youth drinking was often taboo. Today, many young people engage in heavy drinking for pleasure and excitement. Peer networks encourage this behavior through rituals that promote intoxication and provide care for inebriated friends. The findings suggest a need to reconsider cultural prohibitions on youth drinking and advocate for public health interventions promoting low-risk drinking practices.[64]
Definition
[edit]Heavy drinking should not be confused with heavy episodic drinking, commonly known as binge drinking, which takes place over a brief period of a few hours. However, multiple binge drinking sessions within a short timeframe can be classified as heavy drinking.
Heavy alcohol use refers to consumption patterns that take place within a single day, week, or month, depending on the amount consumed:
- The Centers for Disease Control and Prevention defines heavy drinking as consuming more than 8 drinks per week for women and more than 15 drinks per week for men.[65]
- NIAAA defines heavy alcohol use as the consumption of five or more standard drinks in a single day or 15 or more drinks within a week for men, while for women, it is defined as consuming four or more drinks in a day or eight or more drinks per week.[60]
- SAMHSA considers heavy alcohol use to be engaging in binge drinking behaviors on five or more days within a month.[60]
Light, moderate, responsible, and social drinking
[edit]In many cultures, good news is often celebrated by a group sharing alcoholic drinks. For example, sparkling wine may be used to toast the bride at a wedding, and alcoholic drinks may be served to celebrate a baby's birth. Buying someone an alcoholic drink is often considered a gesture of goodwill, an expression of gratitude, or to mark the resolution of a dispute.
Definitions
[edit]Light drinking, moderate drinking, responsible drinking, and social drinking are often used interchangeably, but with slightly different connotations:
- Light drinking - "Alcohol has been found to increase risk for cancer, and for some types of cancer, the risk increases even at low levels of alcohol consumption (less than 1 drink in a day). Caution, therefore, is recommended.", according to the Dietary Guidelines for Americans (DGA).[66] "The Committee recommended that adults limit alcohol intake to no more than 1 drink per day for both women and men for better health" (DGA).[67]
- Moderate drinking - strictly focuses on the amount of alcohol consumed, following alcohol consumption recommendations. This is called "drinking in moderation". The CDC defines "Moderate drinking is having one drink or less in a day for women, or two drinks or less in a day for men."[65]
- According to the WHO nearly half of all alcohol-attributable cancers in the WHO European Region are linked to alcohol consumption, even from "light" or "moderate" drinking – "less than 1.5 litres of wine or less than 3.5 litres of beer or less than 450 millilitres of spirits per week".[15] However, moderate drinking is associated with a further slight increase in cancer risk.[70][71] Also, moderate drinking may disrupt normal brain functioning.[72]
- Responsible drinking - as defined by alcohol industry standards, often emphasizes personal choice and risk management, unlike terms like "social drinking" or "moderate drinking".[73]
- Critics argue that the alcohol industry's definition does not always align with official recommendations for safe drinking limits.[73]
- Social drinking - refers to casual drinking of alcoholic beverages in a social setting (for example bars, nightclubs, or parties) without an intent to become intoxicated. A social drinker is also defined as a person who only drinks alcohol during social events, such as parties, and does not drink while alone (e.g., at home).[74]
- While social drinking often involves moderation, it does not strictly emphasize safety or specific quantities, unlike moderate drinking. Social settings can involve peer pressure to drink more than intended, which can be a risk factor for excessive alcohol consumption. Regularly socializing over drinks can lead to a higher tolerance for alcohol and potentially dependence, especially in groups where drinking is a central activity. Social drinking does not preclude the development of alcohol dependence. High-functioning alcoholism describes individuals who appear to function normally in daily life despite struggling with alcohol dependence.
Self-medication
[edit]
The therapeutic index for ethanol is 10%.[75]
Alcohol can have analgesic (pain-relieving) effects, which is why some people with chronic pain turn to alcohol to self-medicate and try to alleviate their physical discomfort.[76]
People with social anxiety disorder commonly self-medicate with alcohol to overcome their highly set inhibitions.[77] However, self-medicating excessively for prolonged periods of time with alcohol often makes the symptoms of anxiety or depression worse. This is believed to occur as a result of the changes in brain chemistry from long-term use.[78][79][80] A 2023 systematic review highlights the non-addictive use of alcohol for managing developmental issues, personality traits, and psychiatric symptoms, emphasizing the need for informed, harm-controlled approaches to alcohol consumption within a personalized health policy framework.[81]
A 2023 study suggests that people who drink for both recreational enjoyment and therapeutic reasons, like relieving pain and anxiety/depression/stress, have a higher demand for alcohol compared to those who drink solely for recreation or self-medication. This finding raises concerns, as this group may be more likely to develop alcohol use disorder and experience negative consequences related to their drinking.[82] A significant proportion of patients attending mental health services for conditions including anxiety disorders such as panic disorder or social phobia have developed these conditions as a result of recreational alcohol or sedative use.
Self-medication or mental disorders may make people not decline their drinking despite negative consequences. This can create a cycle of dependence that is difficult to break without addressing the underlying mental health issue.
Unscientific
[edit]
The American Heart Association warn that "We've all seen the headlines about studies associating light or moderate drinking with health benefits and reduced mortality. Some researchers have suggested there are health benefits from wine, especially red wine, and that a glass a day can be good for the heart. But there's more to the story. No research has proved a cause-and-effect link between drinking alcohol and better heart health."[84]
In folk medicine, consuming a nightcap is for the purpose of inducing sleep. However, alcohol is not recommended by many doctors as a sleep aid because it interferes with sleep quality.[85]
"Hair of the dog", short for "hair of the dog that bit you", is a colloquial expression in the English language predominantly used to refer to alcohol that is consumed as a hangover remedy (with the aim of lessening the effects of a hangover). Many other languages have their own phrase to describe the same concept. The idea may have some basis in science in the difference between ethanol and methanol metabolism. Instead of alcohol, rehydration before going to bed or during hangover may relieve dehydration-associated symptoms such as thirst, dizziness, dry mouth, and headache.[86][87][88][89][90][91]
Drinking alcohol may cause subclinical immunosuppression.[92]
Spiritual
[edit]
Christian views on alcohol encompass a range of perspectives regarding the consumption of alcoholic beverages, with significant emphasis on moderation rather than total abstinence. The moderationist position is held by Roman Catholics[19] and Eastern Orthodox,[93] and within Protestantism, it is accepted by Anglicans,[94] Lutherans[95][96] and many Reformed churches.[97][98][99][100] Moderationism is also accepted by Jehovah's Witnesses.[101]
Spiritual use of moderate alcohol consumption is also found in some religions and schools with esoteric influences, including the Hindu tantra sect Aghori, in the Sufi Bektashi Order and Alevi Jem ceremonies,[102] in the Rarámuri religion, in the Japanese religion Shinto,[103] by the new religious movement Thelema, in Vajrayana Buddhism, and in Vodou faith of Haiti.
Contraindication
[edit]Pregnancy
[edit]
In the US, alcohol is subject to the FDA drug labeling Pregnancy Category X (Contraindicated in pregnancy).
Minnesota, North Dakota, Oklahoma, South Dakota, and Wisconsin have laws that allow the state to involuntarily commit pregnant women to treatment if they abuse alcohol during pregnancy.[104]
Risks
[edit]Fetal alcohol spectrum disorder
[edit]
Ethanol is classified as a teratogen[105][106][medical citation needed]—a substance known to cause birth defects; according to the U.S. Centers for Disease Control and Prevention (CDC), alcohol consumption by women who are not using birth control increases the risk of fetal alcohol spectrum disorders (FASDs). This group of conditions encompasses fetal alcohol syndrome, partial fetal alcohol syndrome, alcohol-related neurodevelopmental disorder, static encephalopathy, and alcohol-related birth defects.[107] The CDC currently recommends complete abstinence from alcoholic beverages for women of child-bearing age who are pregnant, trying to become pregnant, or are sexually active and not using birth control.[108]
In South Africa, some populations have rates as high as 9%.[109]
Miscarriage
[edit]Miscarriage, also known in medical terms as a spontaneous abortion, is the death and expulsion of an embryo or fetus before it can survive independently.
Alcohol consumption is a risk factor for miscarriage.[110]
Sudden infant death syndrome
[edit]Drinking of alcohol by parents is linked to sudden infant death syndrome (SIDS).[111] One study found a positive correlation between the two during New Years celebrations and weekends.[112] Another found that alcohol use disorder was linked to a more than doubling of risk.[113]
Adverse effects
[edit]
Alcohol has a variety of short-term and long-term adverse effects. Alcohol has both short-term, and long-term effects on the memory, and sleep. It also has reinforcement-related adverse effects, including alcoholism, dependence, and withdrawal; The most severe withdrawal symptoms, associated with physical dependence, can include seizures and delirium tremens, which in rare cases can be fatal. Alcohol use is directly related to considerable morbidity and mortality, for instance due to intoxication and alcohol-related health problems.[114] The World Health Organization advises that there is no safe level of alcohol consumption.[115]
A study in 2015 found that alcohol and tobacco use combined resulted in a significant health burden, costing over a quarter of a billion disability-adjusted life years. Illicit drug use caused tens of millions more disability-adjusted life years.[116]
Drunkorexia is a colloquialism for anorexia or bulimia combined with an alcohol use disorder.[117]
Alcohol is a common cause of substance-induced psychosis or episodes, which may occur through acute intoxication, chronic alcoholism, withdrawal, exacerbation of existing disorders, or acute idiosyncratic reactions.[118] Research has shown that excessive alcohol use causes an 8-fold increased risk of psychotic disorders in men and a 3-fold increased risk of psychotic disorders in women.[119][120] While the vast majority of cases are acute and resolve fairly quickly upon treatment and/or abstinence, they can occasionally become chronic and persistent.[118] Alcoholic psychosis is sometimes misdiagnosed as another mental illness such as schizophrenia.[121]
An inability to process or exhibit emotions in a proper manner has been shown to exist in people who consume excessive amounts of alcohol and those who were exposed to alcohol while fetuses (FAexp).[122] Also, a significant portion (40–60%) of alcoholics experience emotional blindness.[123] Impairments in theory of mind, as well as other social-cognitive deficits, are commonly found in people who have alcohol use disorders, due to the neurotoxic effects of alcohol on the brain, particularly the prefrontal cortex.[124]
Short-term effects
[edit]
The amount of ethanol in the body is typically quantified by blood alcohol content (BAC); weight of ethanol per unit volume of blood. Small doses of ethanol, in general, are stimulant-like[125] and produce euphoria and relaxation; people experiencing these symptoms tend to become talkative and less inhibited, and may exhibit poor judgement. At higher dosages (BAC > 1 gram/liter), ethanol acts as a central nervous system (CNS) depressant,[125] producing at progressively higher dosages, impaired sensory and motor function, slowed cognition, stupefaction, unconsciousness, and possible death. Ethanol is commonly consumed as a recreational substance, especially while socializing, due to its psychoactive effects.
Central nervous system impairment
[edit]
Alcohol causes generalized CNS depression, is a positive allosteric GABAA modulator and is associated and related with decreased anxiety, decreased social inhibition, sedation, impairment of cognitive, memory, motor, and sensory function. It slows and impairs cognition and reaction time and the cognitive skills, impairs judgement, interferes with motor function resulting in motor incoordination, numbness, impairs memory formation, and causes sensory impairment.
Binge drinking can cause generalized impairment of neurocognitive function, dizziness, analgesia, amnesia, ataxia (loss of balance, confusion, sedation, slurred speech), general anaesthesia, decreased libido, nausea, vomiting, blackout, spins, stupor, unconsciousness, and hangover.
At very high concentrations, alcohol can cause anterograde amnesia, markedly decreased heart rate, pulmonary aspiration, positional alcohol nystagmus, respiratory depression, shock, coma and death can result due to profound suppression of CNS function alcohol overdose and can finish in consequent dysautonomia.
Gastrointestinal effects
[edit]
Alcohol can cause nausea and vomiting in sufficiently high amounts (varying by person).
Alcohol stimulates gastric juice production, even when food is not present, and as a result, its consumption stimulates acidic secretions normally intended to digest protein molecules. Consequently, the excess acidity may harm the inner lining of the stomach. The stomach lining is normally protected by a mucosal layer that prevents the stomach from, essentially, digesting itself.[126]
Ingestion of alcohol can initiate systemic pro-inflammatory changes through two intestinal routes: (1) altering intestinal microbiota composition (dysbiosis), which increases lipopolysaccharide (LPS) release, and (2) degrading intestinal mucosal barrier integrity – thus allowing LPS to enter the circulatory system. The major portion of the blood supply to the liver is provided by the portal vein. Therefore, while the liver is continuously fed nutrients from the intestine, it is also exposed to any bacteria and/or bacterial derivatives that breach the intestinal mucosal barrier. Consequently, LPS levels increase in the portal vein, liver and systemic circulation after alcohol intake. Immune cells in the liver respond to LPS with the production of reactive oxygen species, leukotrienes, chemokines and cytokines. These factors promote tissue inflammation and contribute to organ pathology.[127]
Hangover
[edit]
A hangover is the experience of various unpleasant physiological and psychological effects usually following the consumption of alcohol, such as wine, beer, and liquor. Hangovers can last for several hours or for more than 24 hours. Typical symptoms of a hangover may include headache, drowsiness, concentration problems, dry mouth, dizziness, fatigue, gastrointestinal distress (e.g., nausea, vomiting, diarrhea), absence of hunger, light sensitivity, depression, sweating, hyper-excitability, irritability, and anxiety (often referred to as "hangxiety").[128][129]
Though many possible remedies and folk cures have been suggested, there is no compelling evidence to suggest that any are effective for preventing or treating hangovers.[130][131] Avoiding alcohol or drinking in moderation are the most effective ways to avoid a hangover.[130] The socioeconomic consequences of hangovers include workplace absenteeism, impaired job performance, reduced productivity and poor academic achievement. A hangover may also impair performance during potentially dangerous daily activities such as driving a car or operating heavy machinery.[132]
Holiday heart syndrome
[edit]
Holiday heart syndrome, also known as alcohol-induced atrial arrhythmias, is a syndrome defined by an irregular heartbeat and palpitations[133] associated with high levels of ethanol consumption.[134][135] Holiday heart syndrome was discovered in 1978 when Philip Ettinger discovered the connection between arrhythmia and alcohol consumption.[136] It received its common name as it is associated with the binge drinking common during the holidays.[137] It is unclear how common this syndrome is. 5-10% of cases of atrial fibrillation may be related to this condition, but it could be as high 63%.[138]
Positional alcohol nystagmus
[edit]Positional alcohol nystagmus (PAN) is nystagmus (visible jerkiness in eye movement) produced when the head is placed in a sideways position. PAN occurs when the specific gravity of the membrane space of the semicircular canals in the ear differs from the specific gravity of the fluid in the canals because of the presence of alcohol.[139]
Allergic-like reactions
[edit]
Ethanol-containing beverages can cause alcohol flush reactions, exacerbations of rhinitis and, more seriously and commonly, bronchoconstriction in patients with a history of asthma, and in some cases, urticarial skin eruptions, and systemic dermatitis. Such reactions can occur within 1–60 minutes of ethanol ingestion, and may be caused by:[142]
- genetic abnormalities in the metabolism of ethanol, which can cause the ethanol metabolite, acetaldehyde, to accumulate in tissues and trigger the release of histamine, or
- true allergy reactions to allergens occurring naturally in, or contaminating, alcoholic beverages (particularly wine and beer), and
- other unknown causes.
Alcohol flush reaction has also been associated with an increased risk of esophageal cancer in those who do drink.[140][143][144]
Long-term effects
[edit]
According to The Lancet, 'four industries (tobacco, unhealthy food, fossil fuel, and alcohol) are responsible for at least a third of global deaths per year'.[145] In 2024, the World Health Organization published a report including these figures.[146][147]
Due to the long term effects of alcohol abuse, binge drinking is considered to be a major public health issue.[148]
The impact of alcohol on aging is multifaceted. The relationship between alcohol consumption and body weight is the subject of inconclusive studies. Alcoholic lung disease is disease of the lungs caused by excessive alcohol. However, the term 'alcoholic lung disease' is not a generally accepted medical diagnosis.
Alcohol's overall effect on health is uncertain. While some studies suggest moderate consumption might have some benefit, others find any amount increases health risks. This uncertainty is due to conflicting research methods and potential biases, including counting former drinkers as abstainers and the possibility of alcohol industry influence. Because of these issues, experts advise against using alcohol for health reasons. For example, reviews from 2016 found that the "risk of all-cause mortality, and of cancers specifically, rises with increasing levels of consumption, and the level of consumption that minimises health loss is zero".[21] Additionally, in 2023, the World Health Organization (WHO) stated that there is currently no conclusive evidence from studies that the potential benefits of moderate alcohol consumption for cardiovascular disease and type 2 diabetes outweigh the increased cancer risk associated with these drinking levels for individual consumers.[15]
Despite being a widespread issue, social stigma around problematic alcohol use or alcoholism discourages over 80% from seeking help.[149]
Alcoholism
[edit]
Alcoholism or its medical diagnosis alcohol use disorder refers to alcohol addiction, alcohol dependence, dipsomania, and/or alcohol abuse. It is a major problem and many health problems as well as death can result from excessive alcohol use.[150][114] Alcohol dependence is linked to a lifespan that is reduced by about 12 years relative to the average person.[150] In 2004, it was estimated that 4% of deaths worldwide were attributable to alcohol use.[114] Deaths from alcohol are split about evenly between acute causes (e.g., overdose, accidents) and chronic conditions.[114] The leading chronic alcohol-related condition associated with death is alcoholic liver disease.[114] Alcohol dependence is also associated with cognitive impairment and organic brain damage.[150] Some researchers have found that even one alcoholic drink a day increases an individual's risk of health problems by 0.4%.[151]
Stigma surrounding alcohol use disorder is particularly strong and different from the stigma attached to other mental illnesses not caused by substances.[152] People with this condition are seen less as truly ill, face greater blame and social rejection, and experience higher structural discrimination risks.[153]
Two or more consecutive alcohol-free days a week have been recommended to improve health and break dependence.[154][155]
Dry drunk is an expression coined by the founder of Alcoholics Anonymous[156] that describes an alcoholic who no longer drinks but otherwise maintains the same behavior patterns of an alcoholic.[157]
A high-functioning alcoholic (HFA) is a person who maintains jobs and relationships while exhibiting alcoholism.[158][159][160]
Many Native Americans in the United States have been harmed by, or become addicted to, drinking alcohol.[161]
Brain damage
[edit]
While many people associate alcohol's effects with intoxication, the long-term impact of alcohol on the brain can be severe. Binge drinking, or heavy episodic drinking, can lead to alcohol-related brain damage that occurs after a relatively short period of time. This brain damage increases the risk of alcohol-related dementia, and abnormalities in mood and cognitive abilities.
Alcohol can cause Wernicke encephalopathy and Korsakoff syndrome which frequently occur simultaneously, known as Wernicke–Korsakoff syndrome.[162] Lesions, or brain abnormalities, are typically located in the diencephalon which result in anterograde and retrograde amnesia, or memory loss.[162]
Dementia
[edit]Alcohol-related dementia (ARD) is a form of dementia caused by long-term, excessive consumption of alcohol, resulting in neurological damage and impaired cognitive function.[163]
Marchiafava–Bignami disease
[edit]
Marchiafava–Bignami disease is a progressive neurological disease of alcohol use disorder, characterized by corpus callosum demyelination and necrosis and subsequent atrophy. The disease was first described in 1903 by the Italian pathologists Amico Bignami and Ettore Marchiafava in an Italian Chianti drinker.[164][165]
Symptoms can include, but are not limited to lack of consciousness, aggression, seizures, depression, hemiparesis, ataxia, apraxia, coma, etc.[166] There will also be lesions in the corpus callosum.[citation needed]
Liver damage
[edit]
Consuming more than 30 grams of pure alcohol per day over an extended period can significantly increase the risk of developing alcoholic liver disease.[167] During the metabolism of alcohol via the respective dehydrogenases, nicotinamide adenine dinucleotide (NAD) is converted into reduced NAD. Normally, NAD is used to metabolize fats in the liver, and as such alcohol competes with these fats for the use of NAD. Prolonged exposure to alcohol means that fats accumulate in the liver, leading to the term 'fatty liver'. Continued consumption (such as in alcohol use disorder) then leads to cell death in the hepatocytes as the fat stores reduce the function of the cell to the point of death. These cells are then replaced with scar tissue, leading to the condition called cirrhosis.
Cancer
[edit]
Alcoholic beverages have been classified as carcinogenic by leading health organizations for more than two decades, including the WHO's IARC (Group 1 carcinogens)[20] and the U.S. NTP,[168] raising concerns about the potential cancer risk associated with alcohol consumption.
In 2023 the WHO highlighted a statistic: nearly half of all alcohol-attributable cancers in the WHO European Region are linked to alcohol consumption, even from "light" or "moderate" drinking – "less than 1.5 litres of wine or less than 3.5 litres of beer or less than 450 millilitres of spirits per week".[15] This new information suggests that these consumption levels should now be considered high-risk. Many countries exceed these levels by a significant margin. Echoing the WHO's view, a growing number of national public health agencies are prioritizing complete abstinence (teetotalism) and stricter drinking guidelines in their alcohol consumption recommendations.
Alcohol is also a major cause for head and neck cancer, especially laryngeal cancer.
This risk is even higher when alcohol is used together with tobacco.[71][169]
Qualitative analysis reveals that the alcohol industry likely misinforms the public about the alcohol-cancer link, similar to the tobacco industry. The alcohol industry influences alcohol policy and health messages, including those for schoolchildren.[170]
Cardiovascular disease
[edit]Excessive daily alcohol consumption and binge drinking can cause a higher risk of stroke, coronary artery disease, heart failure, fatal hypertensive disease, and fatal aortic aneurysm.[171]
A 2010 study reviewed research on alcohol and heart disease. They found that moderate drinking did not seem to worsen things for people who already had heart problems. But importantly, the researchers did not say that people who do not drink should start in order to improve their heart health.[172] Thus, the safety and potential positive effect of light drinking on the cardiovascular system has not yet been proven. Still alcohol is a major health risk, and even if moderate drinking lowers the risk of some cardiovascular diseases it might increase the risk of others. Therefore starting to drink alcohol in the hope of any benefit is not recommended.[171][173]
The World Heart Federation (2022) recommends against any alcohol intake for optimal heart health.[174][175]
It has also been pointed out that the studies suggesting a positive link between red wine consumption and heart health had flawed methodology in the form of comparing two sets of people which were not actually appropriately paired.[175]
Cardiomyopathy
[edit]
Alcoholic cardiomyopathy (ACM) is a disease in which the long-term consumption of alcohol leads to heart failure.[176] ACM is a type of dilated cardiomyopathy. The heart is unable to pump blood efficiently, leading to heart failure. It can affect other parts of the body if the heart failure is severe. It is most common in males between the ages of 35 and 50.
Hearing loss
[edit]Alcohol, classified as an ototoxin (ear toxin),[177] can contribute to hearing loss sometimes referred to as "cocktail deafness" after exposure to loud noises in drinking environments.[178][179]
Children with fetal alcohol spectrum disorder (FASD) are at an increased risk of having hearing difficulties.
Withdrawal syndrome
[edit]
Discontinuation of alcohol after extended heavy use and associated tolerance development (resulting in dependence) can result in withdrawal. Alcohol withdrawal can cause confusion, paranoia, anxiety, insomnia, agitation, tremors, fever, nausea, vomiting, autonomic dysfunction, seizures, and hallucinations. In severe cases, death can result.
Delirium tremens is a condition that requires people with a long history of heavy drinking to undertake an alcohol detoxification regimen.
Alcohol is one of the more dangerous drugs to withdraw from.[181] Drugs which help to re-stabilize the glutamate system such as N-acetylcysteine have been proposed for the treatment of addiction to cocaine, nicotine, and alcohol.[182]
Cohort studies have demonstrated that the combination of anticonvulsants and benzodiazepines is more effective than other treatments in reducing alcohol withdrawal scores and shortening the duration of intensive care unit stays.[183]
Nitrous oxide has been shown to be an effective and safe treatment for alcohol withdrawal.[184] The gas therapy reduces the use of highly addictive sedative medications (like benzodiazepines and barbiturates).
Cortisol
[edit]Research has looked into the effects of alcohol on the amount of cortisol that is produced in the human body. Continuous consumption of alcohol over an extended period of time has been shown to raise cortisol levels in the body. Cortisol is released during periods of high stress, and can result in the temporary shut down of other physical processes, causing physical damage to the body.
Gout
[edit]
There is a strong association between gout the consumption of alcohol, and sugar-sweetened beverages,[185] with wine presenting somewhat less of a risk than beer or spirits.[186][187]
Ketoacidosis
[edit]Alcoholic ketoacidosis (AKA) is a specific group of symptoms and metabolic state related to alcohol use.[188] Symptoms often include abdominal pain, vomiting, agitation, a fast respiratory rate, and a specific "fruity" smell.[189] Consciousness is generally normal.[190] Complications may include sudden death.[190]
Mental disorders
[edit]Alcohol misuse often coincides with mental health conditions. Many individuals struggling with psychiatric disorders also experience problematic drinking behaviors.[191] For example, alcohol may play a role in depression, with up to 10% of male depression cases in some European countries linked to alcohol use.[192]
Psychiatric genetics research continues to explore the complex interplay between alcohol use, genetic factors, and mental health outcomes; A 2024 study found that excessive drinking and alcohol-related DNA methylation may directly contribute to the causes of mental disorders, possibly through the altered expression of affected genes.[193]
Austrian syndrome
[edit]
Austrian syndrome, also known as Osler's triad, is a medical condition that was named after Robert Austrian in 1957. The presentation of the condition consists of pneumonia, endocarditis, and meningitis, all caused by Streptococcus pneumoniae. It is associated with alcoholism due to hyposplenism (reduced splenic functioning) and can be seen in males between the ages of 40 and 60 years old.[194] Robert Austrian was not the first one to describe the condition, but Richard Heschl (around 1860s) or William Osler were not able to link the signs to the bacteria because microbiology was not yet developed.
The leading cause of Osler's triad (Austrian syndrome) is Streptococcus pneumoniae, which is usually associated with heavy alcohol use.
Polyneuropathy
[edit]Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development.
Specific population
[edit]Women
[edit]Breast cancer
[edit]Drinking alcohol increases the risk for breast cancer.[195] For women in Europe, breast cancer represents the most significant alcohol-related cancer burden.[196]
Breastfeeding difficulties
[edit]Moderate alcohol consumption by breastfeeding mothers can significantly affect infants and cause breastfeeding difficulties. Even one or two drinks, including beer, may reduce milk intake by 20 to 23%, leading to increased agitation and poor sleep patterns. Regular heavy drinking (more than two drinks daily) can shorten breastfeeding duration and cause issues in infants, such as excessive sedation, fluid retention, and hormonal imbalances. Additionally, higher alcohol consumption may negatively impact children's academic achievement.[197]
Neonatal withdrawal
[edit]Babies exposed to alcohol, benzodiazepines, barbiturates, and some antidepressants (SSRIs) during pregnancy may experience neonatal withdrawal.[198]
The onset of clinical presentation typically appears within 48 to 72 hours of birth but may take up to 8 days.[199][200]
Other effects
[edit]
Alcohol may negatively affect sleep. Alcohol consumption disrupts circadian rhythms, with acute intake causing dose-dependent alterations in melatonin and cortisol levels, as well as core body temperature, which normalize the following morning, while chronic alcohol use leads to more severe and persistent disruptions that are associated with alcohol use disorders (AUD) and withdrawal symptoms.[201] Also, Alcohol consumption may increase the risk of sleep disorders, including insomnia,[202] restless legs syndrome,[203] and sleep apnea.[204]
Erosive gastritis is commonly caused by stress, alcohol, some drugs, such as aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), and Crohn's disease.[205][206]
Excessive alcohol intake has been shown to cause immunodeficiency, compromising the body's ability to fight infections and diseases, as evidenced by research on people who regularly consume large amounts of alcohol.[207][208]
Alcohol is associated with instances of sudden death. Sudden arrhythmic death syndrome in alcohol misuse is a significant cause of death among heavy drinkers, characterized by older age and severe liver damage, highlighting the need for family screening for heritable channelopathies.[209] Also, sudden unexpected death in epilepsy is associated with a twofold higher risk in individuals with a history of substance abuse or alcohol dependence.[210]
Alcohol consumption is associated with lower sperm concentration, percentage of normal morphology, and semen volume, but not sperm motility.[211]
Frequent drinking of alcoholic beverages is a major contributing factor in cases of hypertriglyceridemia.[212]
Alcoholism is the single most common cause of chronic pancreatitis.[213][214][215][216][217]
Excess alcohol use is frequently associated with porphyria cutanea tarda (PTC).[218]
Alcohol consumption is a risk factor for Dupuytren's contracture.[219][220]
The majority of those with aspirin-exacerbated respiratory disease experience respiratory reactions to alcohol.[221]
Interactions
[edit]Disorders
[edit]COVID-19
[edit]A 2023 study suggests a link between alcohol consumption and worse COVID-19 outcomes. Researchers analyzed data from over 1.6 million people and found that any level of alcohol consumption increased the risk of severe illness, intensive care unit admission, and needing ventilation compared to non-drinkers. Even a history of drinking was associated with a higher risk of severe COVID-19. These findings suggest that avoiding alcohol altogether might be beneficial during the pandemic.[222]
Diabetes
[edit]See the insulin section.
Hepatitis
[edit]Alcohol consumption can be especially dangerous for those with pre-existing liver damage from hepatitis B or C. Even relatively low amounts of alcohol can be life-threatening in these cases,[223] so a strict adherence to abstinence is highly recommended.[224]
Histamine intolerance
[edit]Alcohol may release histamine in individuals with histamine intolerance.[225]
Mental disorders
[edit]Mental disorders can be a significant risk factor for alcohol abuse.
Alcohol abuse, alcohol dependence, and alcoholism are comorbid with anxiety disorders.[226][227] With dual diagnosis, the initial symptoms of mental illness tend to appear before those of substance abuse.[228] Individuals with common mental health conditions, such as depression, anxiety, or phobias, are twice as likely to also report having an alcohol use disorder, compared to those without these mental health challenges.[229] Alcohol is a major risk factor for self-harm.[230] Individuals with anxiety disorders who self-medicate with drugs or alcohol may also have an increased likelihood of suicidal ideation.[231]

Peptic ulcer disease
[edit]In patients who have a peptic ulcer disease (PUD), the mucosal layer is broken down by ethanol. PUD is commonly associated with the bacteria Helicobacter pylori, which secretes a toxin that weakens the mucosal wall, allowing acid and protein enzymes to penetrate the weakened barrier. Because alcohol stimulates the stomach to secrete acid, a person with PUD should avoid drinking alcohol on an empty stomach. Drinking alcohol causes more acid release, which further damages the already-weakened stomach wall.[232] Complications of this disease could include a burning pain in the abdomen, bloating and in severe cases, the presence of dark black stools indicate internal bleeding.[126] A person who drinks alcohol regularly is strongly advised to reduce their intake to prevent PUD aggravation.[126]
Dosage forms
[edit]Alcohol induced dose dumping (AIDD)
[edit]Alcohol-induced dose dumping (AIDD) is by definition an unintended rapid release of large amounts of a given drug, when administered through a modified-release dosage while co-ingesting ethanol.[233] This is considered a pharmaceutical disadvantage due to the high risk of causing drug-induced toxicity by increasing the absorption and serum concentration above the therapeutic window of the drug. The best way to prevent this interaction is by avoiding the co-ingestion of both substances or using specific controlled-release formulations that are resistant to AIDD.
Drugs
[edit]Alcohol can intensify the sedation caused by antipsychotics, and certain antidepressants.[234]
Alcohol combined with cannabis (not to be confused with tincture of cannabis which contains minute quantities of alcohol) — known as cross-fading and may easily cause spins in people who are drunk and smoke potent cannabis; Ethanol increases plasma tetrahydrocannabinol levels, which suggests that ethanol may increase the absorption of tetrahydrocannabinol.[235]
TOMSO is a lesser-known psychedelic drug and a substituted amphetamine. TOMSO was first synthesized by Alexander Shulgin. According to Shulgin's book PiHKAL, TOMSO is inactive on its own and requires consumption of alcohol to become active.[236]
Hypnotics/sedatives
[edit]
Alcohol can intensify the sedation caused by hypnotics/sedatives such as barbiturates, benzodiazepines, sedative antihistamines, opioids, nonbenzodiazepines/Z-drugs (such as zolpidem and zopiclone).[234]
Dextromethorphan
[edit]Combining alcohol with dextromethorphan significantly increases the risk of overdose and other severe health complications, according to the NIAAA.[237]
Disulfiram-like drugs
[edit]Disulfiram
[edit]Disulfiram inhibits the enzyme acetaldehyde dehydrogenase, which in turn results in buildup of acetaldehyde, a toxic metabolite of ethanol with unpleasant effects. The medication or drug is commonly used to treat alcohol use disorder, and results in immediate hangover-like symptoms upon consumption of alcohol, this effect is widely known as disulfiram effect.
Metronidazole
[edit]Metronidazole is an antibacterial agent that kills bacteria by damaging cellular DNA and hence cellular function.[238] Metronidazole is usually given to people who have diarrhea caused by Clostridioides difficile bacteria. Patients who are taking metronidazole are sometimes advised to avoid alcohol, even after 1 hour following the last dose. Although older data suggested a possible disulfiram-like effect of metronidazole, newer data has challenged this and suggests it does not actually have this effect.
Insulin
[edit]Alcohol consumption can cause hypoglycemia in diabetics on certain medications, such as insulin or sulfonylurea, by blocking gluconeogenesis.[239]
NSAIDs
[edit]The concomitant use of NSAIDs with alcohol and/or tobacco products significantly increases the already elevated risk of peptic ulcers during NSAID therapy.[240][better source needed]
The risk of stomach bleeding is still increased when aspirin is taken with alcohol or warfarin.[241][242]
Stimulants
[edit]
Controlled animal and human studies showed that caffeine (energy drinks) in combination with alcohol increased the craving for more alcohol more strongly than alcohol alone.[243] These findings correspond to epidemiological data that people who consume energy drinks generally showed an increased tendency to take alcohol and other substances.[244][245]
Ethanol interacts with cocaine in vivo to produce cocaethylene, another psychoactive substance which may be substantially more cardiotoxic than either cocaine or alcohol by themselves.[246][247]
Ethylphenidate formation appears to be more common when large quantities of methylphenidate and alcohol are consumed at the same time, such as in non-medical use or overdose scenarios.[248] However, only a small percent of the consumed methylphenidate is converted to ethylphenidate.[249]
While nicotinis mimic the name of classic cocktails like the appletini (their name deriving from "martini"), combining nicotine with alcohol is a bad idea. Tobacco and nicotine actually heighten cravings for alcohol, making this a risky mix.[250]
Methanol and ethylene glycol
[edit]The rate-limiting steps for the elimination of ethanol are in common with certain other substances. As a result, the blood alcohol concentration can be used to modify the rate of metabolism of toxic alcohols, such as methanol and ethylene glycol. Methanol itself is not highly toxic, but its metabolites formaldehyde and formic acid are; therefore, to reduce the rate of production and concentration of these harmful metabolites, ethanol can be ingested.[251] Ethylene glycol poisoning can be treated in the same way.
Warfarin
[edit]Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR, and thus increase the risk of bleeding.[252] The U.S. Food and Drug Administration (FDA) product insert on warfarin states that alcohol should be avoided.[253] The Cleveland Clinic suggests that when taking warfarin one should not drink more than "one beer, 6 oz of wine, or one shot of alcohol per day".[254]
Special population
[edit]Isoniazid
[edit]Levels of liver enzymes in the bloodstream should be frequently checked in daily alcohol drinkers, pregnant women, IV drug users, people over 35, and those who have chronic liver disease, severe kidney dysfunction, peripheral neuropathy, or HIV infection since they are more likely to develop hepatitis from INH.[255][256]
Pharmacology
[edit]Alcohol works in the brain primarily by increasing the effects of γ-Aminobutyric acid (GABA),[257] the major inhibitory neurotransmitter in the brain; by facilitating GABA's actions, alcohol suppresses the activity of the CNS.[257]
The pharmacology of ethanol involves both pharmacodynamics (how it affects the body) and pharmacokinetics (how the body processes it). In the body, ethanol primarily affects the central nervous system, acting as a depressant and causing sedation, relaxation, and decreased anxiety. The exact mechanism remains elusive, but ethanol has been shown to affect ligand-gated ion channels, particularly the GABAA receptor.
After oral ingestion, ethanol is absorbed via the stomach and intestines into the bloodstream. Ethanol is highly water-soluble and diffuses passively throughout the entire body, including the brain. Soon after ingestion, it begins to be metabolized, 90% or more by the liver. One standard drink is sufficient to almost completely saturate the liver's capacity to metabolize alcohol. The main metabolite is acetaldehyde, a toxic carcinogen. Acetaldehyde is then further metabolized into ionic acetate by the enzyme aldehyde dehydrogenase (ALDH). Acetate is not carcinogenic and has low toxicity,[258] but has been implicated in causing hangovers.[259][260] Acetate is further broken down into carbon dioxide and water and eventually eliminated from the body through urine and breath. 5 to 10% of ethanol is excreted unchanged in the breath, urine, and sweat.
Alcohol also direct affects a number of other neurotransmitter systems including those of glutamate, glycine, acetylcholine, and serotonin.[261][262] The pleasurable effects of alcohol ingestion are the result of increased levels of dopamine and endogenous opioids in the reward pathways of the brain.[263][264]
The average human digestive system produces approximately 3 g of ethanol per day through fermentation of its contents.[265]
Safety
[edit]
Symptoms of ethanol overdose may include nausea, vomiting, CNS depression, coma, acute respiratory failure, or death. Levels of even less than 0.1% can cause intoxication, with unconsciousness often occurring at 0.3–0.4%.[234] Death from ethanol consumption is possible when blood alcohol levels reach 0.4%. A blood level of 0.5% or more is commonly fatal. The oral median lethal dose (LD50) of ethanol in rats is 5,628 mg/kg. Directly translated to human beings, this would mean that if a person who weighs 70 kg (150 lb) drank a 500 mL (17 US fl oz) glass of pure ethanol, they would theoretically have a 50% risk of dying. The highest blood alcohol level ever recorded, in which the subject survived, is 1.41%.[266]
A retrospective case-control study conducted from 1990 to 2001 found that alcohol consumption was responsible for over half of all deaths among Russian adults aged 15–54, significantly impacting mortality rates related to causes such as accidents, violence, and various diseases.[267]
In the US, the DEA has claimed illegal drugs are more deadly than alcohol, citing CDC data from 2000 showing similar death counts despite alcohol's wider use.[268] However, this comparison is disputed; a JAMA article reported alcohol-related deaths in 2000 as 85,000, significantly higher than the DEA's figure of 18,539.[269][270]
Toxicity
[edit]The WHO classifies alcohol as a toxic substance.[15] More specifically, ethanol is categorized as a cytotoxin,[271] hepatotoxin,[272] neurotoxin,[273] and ototoxin,[177] which has acute toxic effects on the cells, liver, the nervous system, and the ears, respectively. However, ethanol's acute effects on these organs are usually reversible. This means that even with a single episode of heavy drinking, the body can typically repair itself from the initial damage. Methanol laced alcohol on the other hand can cause blindness even in small quantities.
Ethanol is nutritious but highly intoxicating for most animals, which typically tolerate only up to 4% in their diet. However, a 2024 study found that oriental hornets fed sugary solutions containing 1% to 80% ethanol for a week showed no adverse effects on behavior or lifespan.[274]
A risk assessment using the margin of exposure (MOE) approach evaluated drugs like alcohol and tobacco. Alcohol had a benchmark dose of 531 mg/kg, while heroin's was 2 mg/kg. Alcohol, nicotine, cocaine, and heroin were classified as "high risk" (MOE < 10), and most others as "risk" (MOE < 100). Only alcohol was "high risk" on a population level, with cannabis showing an MOE over 10,000. This confirms alcohol and tobacco as high risk and cannabis as low risk.[275]

Chemistry
[edit]Ethanol is also known chemically as alcohol, ethyl alcohol, or drinking alcohol. It is a simple alcohol with a molecular formula of C2H6O and a molecular weight of 46.0684 g/mol. The molecular formula of ethanol may also be written as CH3−CH2−OH or as C2H5−OH. The latter can also be thought of as an ethyl group linked to a hydroxyl (alcohol) group and can be abbreviated as EtOH. Ethanol is a volatile, flammable, colorless liquid with a slight characteristic odor. Aside from its use as a psychoactive and recreational substance, ethanol is also commonly used as an antiseptic and disinfectant, a chemical and medicinal solvent, and a fuel.
Analogues
[edit]
Ethanol has a variety of analogues, many of which have similar actions and effects. In chemistry, "alcohol" can encompass other mind-altering alcohols besides the kind we drink. Some examples include synthetic drugs like ethchlorvynol and methylpentynol, once used in medicine. Also, ethanol is colloquially referred to as "alcohol" because it is the most prevalent alcohol in alcoholic beverages. But technically all alcoholic beverages contain several types of psychoactive alcohols, that are categorized as primary, secondary, or tertiary. Primary, and secondary alcohols, are oxidized to aldehydes, and ketones, respectively, while tertiary alcohols are generally resistant to oxidation.[276] Ethanol is a primary alcohol that has unpleasant actions in the body, many of which are mediated by its toxic metabolite acetaldehyde.[277] Less prevalent alcohols found in alcoholic beverages, are secondary, and tertiary alcohols. For example, the tertiary alcohol 2M2B which is up to 50 times more potent than ethanol and found in trace quantities in alcoholic beverages, has been synthesized and used as a designer drug. Alcoholic beverages are sometimes laced with toxic alcohols, such as methanol (the simplest alcohol) and isopropyl alcohol.[16] A mild, brief exposure to isopropyl alcohol (which is only moderately more toxic than ethanol) is unlikely to cause any serious harm. But many methanol poisoning incidents have occurred through history, since methanol is lethal even in small quantities, as little as 10–15 milliliters (2–3 teaspoons). Ethanol is used to treat methanol and ethylene glycol toxicity.
The Lucas test differentiates between primary, secondary, and tertiary alcohols.
Production
[edit]Ethanol is produced naturally as a byproduct of the metabolic processes of yeast and hence is present in any yeast habitat, including even endogenously in humans, but it does not cause raised blood alcohol content as seen in the rare medical condition auto-brewery syndrome (ABS). It is manufactured through hydration of ethylene or by brewing via fermentation of sugars with yeast (most commonly Saccharomyces cerevisiae). The sugars are commonly obtained from sources like steeped cereal grains (e.g., barley), grape juice, and sugarcane products (e.g., molasses, sugarcane juice). Ethanol–water mixture which can be further purified via distillation.
Home-made alcoholic beverages
[edit]Homebrewing
[edit]
Homebrewing is the brewing of beer or other alcoholic beverages on a small scale for personal, non-commercial purposes. Supplies, such as kits and fermentation tanks, can be purchased locally at specialty stores or online. Beer was brewed domestically for thousands of years before its commercial production, although its legality has varied according to local regulation. Homebrewing is closely related to the hobby of home distillation, the production of alcoholic spirits for personal consumption; however home distillation is generally more tightly regulated.
Moonshine
[edit]Although methanol is not produced in toxic amounts by fermentation of sugars from grain starches,[278] it is a major occurrence in fruit spirits.[279] However, in modern times, reducing methanol with the absorption of a molecular sieve is a practical method for production.[280]
Society and culture
[edit]Alcohol and society is a multifaceted issue that encompasses various social, health, and economic dimensions.
Evolving alcohol norms reflect a significant shift in societal attitudes towards alcohol consumption, driven by growing awareness of its health impacts and the cultural implications of drinking. Historically, alcohol has been deeply embedded in social practices and rituals, often celebrated as a cornerstone of community gatherings and personal milestones. Historically, alcohol has been deeply embedded in social practices and rituals, often celebrated as a cornerstone of community gatherings and personal milestones. Drinking culture is the set of traditions and social behaviours that surround the consumption of alcoholic beverages as a recreational drug and social lubricant.
However, contemporary movements challenge these traditional norms, advocating for a more mindful approach to drinking. Alcohol denormalization aims to reduce acceptance of excessive drinking,[281] while intermittent sobriety and the sober curious movement promote mindful consumption and alcohol-free lifestyles.[282][283][284]
Alcohol education is the practice of disseminating disinformation about the effects of alcohol on health, as well as society and the family unit.[285]
Alcohol as a gateway drug
[edit]Alcohol and nicotine prime the brain for a heightened response to other drugs and are, like marijuana, also typically used before a person progresses to other, more harmful substances."[286]
A study of drug use of 14,577 U.S. 12th graders showed that alcohol consumption was associated with an increased probability of later use of tobacco, cannabis, and other illegal drugs.[287]
This section needs expansion. You can help by adding to it. (June 2024) |
History
[edit]
Alcoholic beverages have been produced since the Neolithic period, as early as 7000 BC in China.[288]
Since antiquity, prior to the development of modern agents, alcohol was used as a general anaesthetic.[289]
In the history of wound care, beer,[290] and wine,[291] are recognized as substances used for healing wounds.
Late Middle Ages
[edit]Alcohol has been used as an antiseptic as early as 1363 with evidence to support its use becoming available in the late 1800s.[citation needed]
Early modern period
[edit]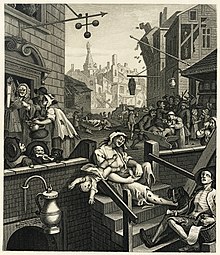
The popular story dates the etymology of the term Dutch courage to English soldiers fighting in the Anglo-Dutch Wars[292] (1652–1674) and perhaps as early as the Thirty Years' War (1618–1648). One version states that jenever (or Dutch gin) was used by English soldiers for its calming effects before battle, and for its purported warming properties on the body in cold weather. Another version has it that English soldiers noted the bravery-inducing effects of jenever on Dutch soldiers.[293][294]
The Gin Craze was a period in the first half of the 18th century when the consumption of gin increased rapidly in Great Britain, especially in London. By 1743, England was drinking 2.2 gallons (10 litres) of gin per person per year. The Sale of Spirits Act 1750 (commonly known as the Gin Act 1751) was an Act of the Parliament of Great Britain (24 Geo. 2. c. 40) which was enacted to reduce the consumption of gin and other distilled spirits, a popular pastime[295] that was regarded as one of the primary causes of crime in London.[296]
Modern period
[edit]
The rum ration (also called the tot) was a daily amount of rum given to sailors on Royal Navy ships. It started 1866 and was abolished in 1970 after concerns that the intake of strong alcohol would lead to unsteady hands when working machinery.
The Andrew Johnson alcoholism debate is the dispute, originally conducted among the general public, and now typically a question for historians, about whether or not Andrew Johnson, the 17th president of the United States (1865–1869), drank to excess.
The Bratt System was a system that was used in Sweden (1919–1955) and similarly in Finland (1944–1970) to control alcohol consumption, by rationing of liquor. Every citizen allowed to consume alcohol was given a booklet called a motbok (viinakortti in Finland), in which a stamp was added each time a purchase was made at Systembolaget (in Sweden) and Alko (in Finland).[297] A similar system also existed in Estonia between July 1, 1920 to December 31, 1925.[298] The stamps were based on the amount of alcohol bought. When a certain amount of alcohol had been bought, the owner of the booklet had to wait until next month to buy more.
The Medicinal Liquor Prescriptions Act of 1933 was a law passed by Congress in response to the abuse of medicinal liquor prescriptions during Prohibition.
Gilbert Paul Jordan (aka The Boozing Barber) was a Canadian serial killer who is believed to have committed the so-called "alcohol murders" between 1965–c. 2004 in Vancouver, British Columbia.
See also
[edit]- Alcohol myopia
- Cannabis (drug)
- Glossary of alcohol (drug) terms
- Lean (drug)
- Rum-running
- Responsible drug use
- GABAergics
- GABRD (δ subunit-containing receptors)
- Pigovian taxes, which are to pay for the damage to society caused by these goods.
- Speedball (drug)
- Sin taxes are used to increase the price in an effort to lower their use, or failing that, to increase and find new sources of revenue.
References
[edit]- ^ WHO Expert Committee on Problems Related to Alcohol Consumption: second report. Geneva, Switzerland: World Health Organization. 2007. p. 23. ISBN 978-92-4-120944-1. Retrieved 3 March 2015.
...alcohol dependence (is) a substantial risk of regular heavy drinking...
- ^ Vengeliene V, Bilbao A, Molander A, Spanagel R (May 2008). "Neuropharmacology of alcohol addiction". British Journal of Pharmacology. 154 (2): 299–315. doi:10.1038/bjp.2008.30. PMC 2442440. PMID 18311194.
(Compulsive alcohol use) occurs only in a limited proportion of about 10–15% of alcohol users....
- ^ Gilman JM, Ramchandani VA, Crouss T, Hommer DW (January 2012). "Subjective and neural responses to intravenous alcohol in young adults with light and heavy drinking patterns". Neuropsychopharmacology. 37 (2): 467–77. doi:10.1038/npp.2011.206. PMC 3242308. PMID 21956438.
- ^ a b c d e f Principles of Addiction: Comprehensive Addictive Behaviors and Disorders. Academic Press. 17 May 2013. pp. 162–. ISBN 978-0-12-398361-9.
- ^ a b c Holford NH (November 1987). "Clinical pharmacokinetics of ethanol". Clinical Pharmacokinetics. 13 (5): 273–92. doi:10.2165/00003088-198713050-00001. PMID 3319346. S2CID 19723995.
- ^ a b c d Pohorecky LA, Brick J (1988). "Pharmacology of ethanol". Pharmacology & Therapeutics. 36 (2–3): 335–427. doi:10.1016/0163-7258(88)90109-x. PMID 3279433.
- ^ Becker CE (September 1970). "The clinical pharmacology of alcohol". California Medicine. 113 (3): 37–45. PMC 1501558. PMID 5457514.
- ^ a b Levine B (2003). Principles of Forensic Toxicology. Amer. Assoc. for Clinical Chemistry. pp. 161–. ISBN 978-1-890883-87-4.
- ^ Iber FL (26 November 1990). Alcohol and Drug Abuse as Encountered in Office Practice. CRC Press. pp. 74–. ISBN 978-0-8493-0166-7.
- ^ a b c Haynes WM, ed. (2011). CRC Handbook of Chemistry and Physics (92nd ed.). Boca Raton, Florida: CRC Press. p. 3.246. ISBN 1-4398-5511-0.
- ^ "The Origin Of The Word 'Alcohol'". Science Friday. Retrieved 30 September 2024.
- ^ Song F, Walker MP (8 November 2023). "Sleep, alcohol, and caffeine in financial traders". PLOS ONE. 18 (11): e0291675. Bibcode:2023PLoSO..1891675S. doi:10.1371/journal.pone.0291675. PMC 10631622. PMID 37939019.
- ^ Degenhardt L, et al. (GBD 2016 Alcohol and Drug Use Collaborators) (December 2018). "The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016". The Lancet. Psychiatry. 5 (12): 987–1012. doi:10.1016/S2215-0366(18)30337-7. PMC 6251968. PMID 30392731.
- ^ Costardi JV, Nampo RA, Silva GL, Ribeiro MA, Stella HJ, Stella MB, et al. (August 2015). "A review on alcohol: from the central action mechanism to chemical dependency". Revista da Associacao Medica Brasileira. 61 (4): 381–387. doi:10.1590/1806-9282.61.04.381. PMID 26466222.
- ^ a b c d e f "No level of alcohol consumption is safe for our health". World Health Organization. 4 January 2023.
- ^ a b Collins SE, Kirouac M (2013). "Alcohol Consumption". Encyclopedia of Behavioral Medicine. Springer. pp. 61–65. doi:10.1007/978-1-4419-1005-9_626. ISBN 978-1-4419-1004-2.
- ^ Różański M, Pielech-Przybylska K, Balcerek M (September 2020). "Influence of Alcohol Content and Storage Conditions on the Physicochemical Stability of Spirit Drinks". Foods. 9 (9): 1264. doi:10.3390/foods9091264. PMC 7555269. PMID 32916918.
- ^ Code of Canon Law, 1983 Archived 2006-06-19 at the Wayback Machine
- ^ a b Madrid P (March 1992). "Wrath of Grapes". This Rock. 3 (3). Archived from the original on 7 March 2007. Retrieved 16 March 2007.
The [Catholic] Church teaches ... that wine, like food, sex, laughter, and dancing, is a good thing when enjoyed in its proper time and context. To abuse any good thing is a sin, but the thing abused does not itself become sinful.
- ^ a b "Agents Classified by the IARC Monographs, Volumes 1–111" (PDF). Archived from the original (PDF) on 25 October 2011 – via monographs.iarc.fr.
- ^ a b Griswold MG, Fullman N, Hawley C, Arian N, Zimsen SR, Tymeson HD, et al. (September 2018). "Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016". Lancet. 392 (10152): 1015–1035. doi:10.1016/S0140-6736(18)31310-2. PMC 6148333. PMID 30146330.
- ^ a b Global status report on alcohol and health (PDF). World Health Organization. 2018. ISBN 978-92-4-156563-9.
- ^ "Over 3 million annual deaths due to alcohol and drug use, majority among men". wwho.int.
- ^ "Canada's Guidance on Alcohol and Health". ccsa.ca. Archived from the original on 11 September 2023. Retrieved 25 September 2023.
- ^ "Empfehlungen zum Umgang mit Alkohol" (PDF). Deutsche Hauptstelle für Suchtfragen (in German). Archived (PDF) from the original on 24 October 2023. Retrieved 30 October 2023.
- ^ "What Are the U.S. Guidelines for Drinking? - Rethinking Drinking". National Institute on Alcohol Abuse and Alcoholism (NIAAA).
- ^ Kimmel M (2008). Guyland. New York: Harper. ISBN 978-0-06-083134-9.
- ^ Klein J (11 February 2022). "Dry dating: The rise of sober love and sex". www.bbc.com.
- ^ McAlpine D (7 November 2011). "The Secret to Great Dating This Winter? Cut The Booze". HuffPost UK.
- ^ Thompson SJ (10 January 2019). "Trend for sober dating sees an increase as singles seek love during Dry January". Daily Record.
- ^ Yang C, Latkin C, Luan R, Nelson K (February 2013). "Factors associated with drinking alcohol before visiting female sex workers among men in Sichuan Province, China". AIDS and Behavior. 17 (2): 568–573. doi:10.1007/s10461-012-0260-8. PMC 4017933. PMID 22806054.
- ^ Beksinska A, Karlsen O, Gafos M, Beattie TS (2023). "Alcohol use and associated risk factors among female sex workers in low- and middle-income countries: A systematic review and meta-analysis". PLOS Global Public Health. 3 (6): e0001216. doi:10.1371/journal.pgph.0001216. PMC 10263362. PMID 37310993.
- ^ Malatesta VJ, Pollack RH, Crotty TD, Peacock LJ (February 1982). "Acute Alcohol Intoxication and Female Orgasmic Response". The Journal of Sex Research. 18 (1): 1–17. doi:10.1080/00224498209551130. JSTOR 3812507.
- ^ Jones E, Fear NT (April 2011). "Alcohol use and misuse within the military: a review". International Review of Psychiatry. 23 (2): 166–172. doi:10.3109/09540261.2010.550868. PMID 21521086.
- ^ Dworkin ER, Bergman HE, Walton TO, Walker DD, Kaysen DL (2018). "Co-Occurring Post-Traumatic Stress Disorder and Alcohol Use Disorder in U.S. Military and Veteran Populations". Alcohol Research. 39 (2): 161–169. PMC 6561402. PMID 31198655.
- ^ Richardson JD, St Cyr KC, McIntyre-Smith AM, Haslam D, Elhai JD, Sareen J (August 2012). "Examining the association between psychiatric illness and suicidal ideation in a sample of treatment-seeking Canadian peacekeeping and combat veterans with posttraumatic stress disorder PTSD". Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie. 57 (8): 496–504. doi:10.1177/070674371205700808. PMID 22854032.
- ^ Kalinowski K (21 July 2023). "Rosyjska armia pije na potęgę. To jeden z głównych powodów wysokiej śmiertelności wojsk Putina na froncie" [The Russian army drinks heavily. This is one of the main reasons for the high mortality of Putin's troops at the front]. Gazeta Wyborcza (in Polish). Retrieved 24 July 2023.
- ^ Hambling D. "Are Drugs Making Russian Soldiers Act Like Zombies?". Forbes. Retrieved 24 July 2023.
- ^ Lister T, Pleitgen F, Hak K (1 February 2023). "Fighting Wagner is like a 'zombie movie' says Ukrainian soldier". CNN. Retrieved 24 July 2023.
- ^ "Ukrainians warn of 'drug-fuelled' Russian 'zombie waves' on the frontline". Forces Network. 1 March 2023. Retrieved 24 July 2023.
- ^ "Composition of Foods Raw, Processed, Prepared USDA National Nutrient Database for Standard Reference, Release 26 Documentation and User Guide" (PDF). USDA. August 2013. p. 14. Archived (PDF) from the original on 25 September 2014. Retrieved 3 February 2014.
- ^ Metz R, Berger S, Mako M (August 1969). "Potentiation of the plasma insulin response to glucose by prior administration of alcohol. An apparent islet-priming effect" (PDF). Diabetes. 18 (8): 517–522. doi:10.2337/diab.18.8.517. PMID 4897290. S2CID 32072796. Archived (PDF) from the original on 22 February 2014. Retrieved 11 February 2014.
- ^ Shelmet JJ, Reichard GA, Skutches CL, Hoeldtke RD, Owen OE, Boden G (April 1988). "Ethanol causes acute inhibition of carbohydrate, fat, and protein oxidation and insulin resistance". The Journal of Clinical Investigation. 81 (4): 1137–1145. doi:10.1172/JCI113428. PMC 329642. PMID 3280601.
- ^ Leeds JS, Oppong K, Sanders DS (May 2011). "The role of fecal elastase-1 in detecting exocrine pancreatic disease". Nature Reviews. Gastroenterology & Hepatology. 8 (7): 405–415. doi:10.1038/nrgastro.2011.91. PMID 21629239.
- ^ Osborne VA, Sher KJ, Winograd RP (2011). "Disordered eating patterns and alcohol misuse in college students: Evidence for "drunkorexia"?". Comprehensive Psychiatry. 52 (6): e12. doi:10.1016/j.comppsych.2011.04.038.
- ^ "'Drunkorexia:' A Recipe for Disaster". ScienceDaily. 17 October 2011.
- ^ Kopelman MD, Thomson AD, Guerrini I, Marshall EJ (2009). "The Korsakoff syndrome: clinical aspects, psychology and treatment". Alcohol and Alcoholism. 44 (2): 148–154. doi:10.1093/alcalc/agn118. PMID 19151162.
- ^ Mégarbane B (24 August 2010). "Treatment of patients with ethylene glycol or methanol poisoning: focus on fomepizole". Open Access Emergency Medicine. 2: 67–75. doi:10.2147/OAEM.S5346. PMC 4806829. PMID 27147840.
- ^ British National Formulary: BNF 69 (69th ed.). British Medical Association. 2015. pp. 42, 838. ISBN 978-0-85711-156-2.
- ^ Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA (2002). "American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning". Journal of Toxicology. Clinical Toxicology. 40 (4): 415–46. doi:10.1081/CLT-120006745. PMID 12216995. S2CID 26495651.
- ^ "Our 'drinking culture' explored". www.linkedin.com. Retrieved 25 January 2024.
- ^ "Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings" (PDF). United States Substance Abuse and Mental Health Services Administration. United States Department of Health and Human Services. Retrieved 11 June 2015.
- ^ Esser MB, Hedden SL, Kanny D, Brewer RD, Gfroerer JC, Naimi TS (November 2014). "Prevalence of alcohol dependence among US adult drinkers, 2009–2011". Preventing Chronic Disease. 11: E206. doi:10.5888/pcd11.140329. PMC 4241371. PMID 25412029.
- ^ Renaud SC (2001). "Diet and stroke". The Journal of Nutrition, Health & Aging. 5 (3): 167–172. PMID 11458287.
- ^ Nyberg ST, Batty GD, Pentti J, Madsen IE, Alfredsson L, Bjorner JB, et al. (August 2022). "Association of alcohol use with years lived without major chronic diseases: A multicohort study from the IPD-Work consortium and UK Biobank". The Lancet Regional Health. Europe. 19: 100417. doi:10.1016/j.lanepe.2022.100417. PMC 9160494. PMID 35664051.
- ^ Perez-Araluce R, Bes-Rastrollo M, Martínez-González MÁ, Toledo E, Ruiz-Canela M, Barbería-Latasa M, et al. (February 2023). "Effect of Binge-Drinking on Quality of Life in the 'Seguimiento Universidad de Navarra' (SUN) Cohort". Nutrients. 15 (5): 1072. doi:10.3390/nu15051072. PMC 10004732. PMID 36904072.
- ^ Wakabayashi KT, Greeman EA, Barrett ST, Bevins RA (September 2021). "The Sugars in Alcohol Cocktails Matter". ACS Chemical Neuroscience. 12 (18): 3284–3287. doi:10.1021/acschemneuro.1c00526. PMC 8447180. PMID 34428024.
- ^ Calhoun BH, Maggs JL (November 2022). "Pregame Heavy Episodic Drinking and Its Association With Negative Consequences and Other Risky Substance Use Behaviors". Journal of Studies on Alcohol and Drugs. 83 (6): 793–801. doi:10.15288/jsad.20-00481. PMC 9756404. PMID 36484576.
- ^ Ing TS, Sam A, Tang HL, Lau KK (April 2024). "Severe Ethanol Poisoning Among United States College Fraternity Pledges". Cureus. 16 (4): e58650. doi:10.7759/cureus.58650. PMC 11032146. PMID 38644953.
- ^ a b c "Drinking Levels and Patterns Defined". National Institute on Alcohol Abuse and Alcoholism (NIAAA).
- ^ Neal DJ, Fromme K (November 2007). "Hook 'em horns and heavy drinking: alcohol use and collegiate sports". Addictive Behaviors. 32 (11): 2681–2693. doi:10.1016/j.addbeh.2007.06.020. PMC 2527738. PMID 17662537.
- ^ Kushnir V, Cunningham JA (November 2014). "Event-specific drinking in the general population". Journal of Studies on Alcohol and Drugs. 75 (6): 968–972. doi:10.15288/jsad.2014.75.968. PMC 4211338. PMID 25343654.
- ^ Kelly Grinsteinner (28 November 2005). "Controlled drinking experiment teaches valuable lesson". The Daily Tribune. Archived from the original on 23 February 2008.
- ^ Dumbili EW (January 2022). "'I just drink to feel abnormal for some time': Reconfiguring heavy drinking and intoxication as pleasurable". The International Journal on Drug Policy. 99: 103454. doi:10.1016/j.drugpo.2021.103454. PMID 34537478.
- ^ a b "Alcohol Use and Your Health". Alcohol Use. 11 June 2024.
- ^ Snetselaar LG, de Jesus JM, DeSilva DM, Stoody EE (November 2021). "Dietary Guidelines for Americans, 2020-2025: Understanding the Scientific Process, Guidelines, and Key Recommendations". Nutrition Today. 56 (6): 287–295. doi:10.1097/NT.0000000000000512. PMC 8713704. PMID 34987271.
- ^ Snetselaar LG, de Jesus JM, DeSilva DM, Stoody EE (November 2021). "Dietary Guidelines for Americans, 2020-2025: Understanding the Scientific Process, Guidelines, and Key Recommendations". Nutrition Today. 56 (6): 287–295. doi:10.1097/NT.0000000000000512. PMC 8713704. PMID 34987271.
- ^ Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. (February 2015). "Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis". British Journal of Cancer. 112 (3): 580–593. doi:10.1038/bjc.2014.579. PMC 4453639. PMID 25422909.
- ^ Caprio GG, Picascia D, Dallio M, Vitiello PP, Giunta EF, De Falco V, et al. (2020). "Light Alcohol Drinking and the Risk of Cancer Development: A Controversial Relationship". Reviews on Recent Clinical Trials. 15 (3): 164–177. doi:10.2174/1574887115666200628143015. PMID 32598271.
- ^ de Menezes RF, Bergmann A, Thuler LC (2013). "Alcohol consumption and risk of cancer: a systematic literature review". Asian Pacific Journal of Cancer Prevention. 14 (9): 4965–4972. doi:10.7314/apjcp.2013.14.9.4965. PMID 24175760.
- ^ a b Gormley M, Creaney G, Schache A, Ingarfield K, Conway DI (November 2022). "Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors". British Dental Journal. 233 (9): 780–786. doi:10.1038/s41415-022-5166-x. PMC 9652141. PMID 36369568.
- ^ Yasinski E (12 January 2021). "Even If You Don't Drink Daily, Alcohol Can Mess With Your Brain". Discover.
- ^ a b Maani Hessari N, Petticrew M (March 2018). "What does the alcohol industry mean by 'Responsible drinking'? A comparative analysis". Journal of Public Health. 40 (1). Oxford, England: 90–97. doi:10.1093/pubmed/fdx040. PMID 28398571.
- ^ "Definition of SOCIAL DRINKER". Merriam-Webster. Retrieved 2 April 2024.
- ^ Gable RS (June 2004). "Comparison of acute lethal toxicity of commonly abused psychoactive substances" (PDF). Addiction. 99 (6): 686–96. doi:10.1111/j.1360-0443.2004.00744.x. PMID 15139867.
- ^ Riley JL 3rd, King C (September 2009). "Self-report of alcohol use for pain in a multi-ethnic community sample". The Journal of Pain. 10 (9): 944–52. doi:10.1016/j.jpain.2009.03.005. PMC 2734914. PMID 19712901.
- ^ Carrigan MH, Randall CL (March 2003). "Self-medication in social phobia: a review of the alcohol literature". Addictive Behaviors. 28 (2): 269–284. doi:10.1016/S0306-4603(01)00235-0. PMC 6683821. PMID 12573678. Archived from the original on 31 January 2018. Retrieved 5 April 2024.
- ^ Wetterling T, Junghanns K (December 2000). "Psychopathology of alcoholics during withdrawal and early abstinence". European Psychiatry. 15 (8): 483–488. doi:10.1016/S0924-9338(00)00519-8. PMID 11175926. S2CID 24094651.
- ^ Cowley DS (January 1992). "Alcohol abuse, substance abuse, and panic disorder". The American Journal of Medicine. 92 (1A): 41S–48S. doi:10.1016/0002-9343(92)90136-Y. PMID 1346485.
- ^ Cosci F, Schruers KR, Abrams K, Griez EJ (June 2007). "Alcohol use disorders and panic disorder: a review of the evidence of a direct relationship". The Journal of Clinical Psychiatry. 68 (6): 874–880. doi:10.4088/JCP.v68n0608. PMID 17592911.
- ^ Müller CP, Schumann G, Rehm J, Kornhuber J, Lenz B (July 2023). "Self-management with alcohol over lifespan: psychological mechanisms, neurobiological underpinnings, and risk assessment". Molecular Psychiatry. 28 (7): 2683–2696. doi:10.1038/s41380-023-02074-3. PMC 10615763. PMID 37117460.
- ^ Ferguson E, Fiore A, Yurasek AM, Cook RL, Boissoneault J (February 2023). "Association of therapeutic and recreational reasons for alcohol use with alcohol demand". Experimental and Clinical Psychopharmacology. 31 (1): 106–115. doi:10.1037/pha0000554. PMC 9399303. PMID 35201830.
- ^ "Myth busters". who.int. World Health Organization.
- ^ "Is drinking alcohol part of a healthy lifestyle?". American Heart Association. 2020.
- ^ Bhandari S (ed.). "Alcohol & Sleep: Nix the Nightcap?". Webmd. Retrieved 1 November 2015.
- ^ Penning R, van Nuland M, Fliervoet LA, Olivier B, Verster JC (June 2010). "The pathology of alcohol hangover". Current Drug Abuse Reviews. 3 (2): 68–75. doi:10.2174/1874473711003020068. PMID 20712596.
- ^ Wiese JG, Shlipak MG, Browner WS (June 2000). "The alcohol hangover". Annals of Internal Medicine. 132 (11): 897–902. doi:10.7326/0003-4819-132-11-200006060-00008. PMID 10836917.
- ^ Breene S (6 October 2016). "The best and worst foods to cure a hangover". The Atlanta Journal-Constitution. Retrieved 30 July 2017.
- ^ Acocella J (26 May 2008). "A Few Too Many: Is there any hope for the hung over?". The New Yorker.
- ^ Harding A (21 December 2010). "10 Hangover Remedies: What Works?". Health.com. Retrieved 30 July 2017.
- ^ Howard J (17 March 2017). "What to eat to beat a hangover". CNN. Retrieved 30 July 2017.
- ^ Szabo G, Saha B (2015). "Alcohol's Effect on Host Defense". Alcohol Research. 37 (2): 159–170. PMC 4590613. PMID 26695755.
- ^ O'Callaghan P (March 1992). "The Spirit of True Christianity". Word Magazine. Antiochian Orthodox Christian Archdiocese of North America: 8–9. Retrieved 16 March 2007.
So alcohol, sex, the body, money, television, and music are all good things. It is only the abuse of these things that is bad—drunkenness, pornography, compulsive gambling, etc. Even drugs marijuana, cocaine, heroin—all have good uses for medical and other reasons. It's only the abuse of them for pleasure that is wrong.
- ^ Ethical Investment Advisory Group (January 2005). "Alcohol: An inappropriate investment for Anglicanism" (PDF). Church of England. Archived from the original (PDF) on 26 February 2007. Retrieved 8 February 2007.
Christians who are committed to total abstinence have sometimes interpreted biblical references to wine as meaning unfermented grape juice, but this is surely inconsistent with the recognition of both good and evil in the biblical attitude to wine. It is self-evident that human choice plays a crucial role in the use or abuse of alcohol.
- ^ "Responding to Opportunities for 'Interim Eucharistic Sharing'" (PDF). Evangelical Lutheran Church in America. Archived from the original (PDF) on 14 February 2007. Retrieved 24 February 2007.
While many Lutheran congregations also provide grape juice or unfermented wine as an alternative, Lutherans have more emphasized the historical and ecumenical continuities which wine provides, as well as the richness and multivalences of its symbolic associations.
- ^ "Theology and Practice of The Lord's Supper - Part I" (PDF). Lutheran Church–Missouri Synod. May 1983. Retrieved 24 February 2007.
- ^ "Alcohol". Presbyterian 101. Presbyterian Church (USA). Archived from the original on 13 April 2003. Retrieved 24 February 2007.
- ^ "Introduction to Worship in the United Church of Christ" (PDF). Book of Worship. United Church of Christ. 1986. pp. Footnote 27. Archived from the original (PDF) on 8 June 2012. Retrieved 24 February 2007.
- ^ "Alcohol". Christian Reformed Church in North America. 1996–2007. Archived from the original on 21 October 2012. Retrieved 24 February 2007.
- ^ "Alcohol, Beverage use of". Presbyterian Church in America, 8th General Assembly. 1980. Archived from the original on 12 September 2017. Retrieved 24 February 2007.
- ^ "Maintain a Balanced View Of Alcohol". Watch Tower Bible and Tract Society of Pennsylvania. 2004. Retrieved 24 November 2012.
- ^ Soileau M (August 2012). "Spreading the Sofra: Sharing and Partaking in the Bektashi Ritual Meal". History of Religions. 52 (1): 1–30. doi:10.1086/665961. JSTOR 10.1086/665961.
- ^ Bocking B (1997). A popular dictionary of Shintō (Rev. ed.). Richmond, Surrey [U.K.]: Curzon Press. ISBN 0-7007-1051-5. OCLC 264474222.
- ^ "Civil Commitment: About This Policy". Alcohol Policy Information System. NIAAA. Retrieved 15 March 2024.
- ^ Popova S, Dozet D, Shield K, Rehm J, Burd L (September 2021). "Alcohol's Impact on the Fetus". Nutrients. 13 (10): 3452. doi:10.3390/nu13103452. PMC 8541151. PMID 34684453.
- ^ Chung DD, Pinson MR, Bhenderu LS, Lai MS, Patel RA, Miranda RC (August 2021). "Toxic and Teratogenic Effects of Prenatal Alcohol Exposure on Fetal Development, Adolescence, and Adulthood". International Journal of Molecular Sciences. 22 (16): 8785. doi:10.3390/ijms22168785. PMC 8395909. PMID 34445488.
- ^ "Facts about FASDs". 16 April 2015. Archived from the original on 23 May 2015. Retrieved 10 June 2015.
- ^ "More than 3 million US women at risk for alcohol-exposed pregnancy". Centers for Disease Control and Prevention. 2 February 2016. Retrieved 3 March 2016.
'drinking any alcohol at any stage of pregnancy can cause a range of disabilities for their child,' said Coleen Boyle, Ph.D., director of CDC's National Center on Birth Defects and Developmental Disabilities.
- ^ Riley EP, Infante MA, Warren KR (June 2011). "Fetal alcohol spectrum disorders: an overview". Neuropsychology Review. 21 (2): 73–80. doi:10.1007/s11065-011-9166-x. PMC 3779274. PMID 21499711.
- ^ Oliver A, Overton C (May 2014). "Diagnosis and management of miscarriage". The Practitioner. 258 (1771): 25–8, 3. PMID 25055407.
- ^ Van Nguyen JM, Abenhaim HA (October 2013). "Sudden infant death syndrome: review for the obstetric care provider". American Journal of Perinatology. 30 (9): 703–714. doi:10.1055/s-0032-1331035. PMID 23292938. S2CID 25034518.
- ^ Phillips DP, Brewer KM, Wadensweiler P (March 2011). "Alcohol as a risk factor for sudden infant death syndrome (SIDS)". Addiction. 106 (3): 516–525. doi:10.1111/j.1360-0443.2010.03199.x. PMID 21059188. Archived from the original on 6 September 2017. Retrieved 6 September 2017.
- ^ O'Leary CM, Jacoby PJ, Bartu A, D'Antoine H, Bower C (March 2013). "Maternal alcohol use and sudden infant death syndrome and infant mortality excluding SIDS". Pediatrics. 131 (3): e770–e778. doi:10.1542/peds.2012-1907. PMID 23439895. S2CID 2523083.
- ^ a b c d e Friedman HS (26 August 2011). The Oxford Handbook of Health Psychology. Oxford University Press, USA. pp. 699–. ISBN 978-0-19-534281-9.
- ^ "No level of alcohol consumption is safe for our health". www.who.int. Retrieved 13 October 2023.
- ^ Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, et al. (October 2018). "Global statistics on alcohol, tobacco and illicit drug use: 2017 status report". Addiction. 113 (10): 1905–1926. doi:10.1111/add.14234. hdl:11343/283940. PMID 29749059.
- ^ Reimold D (29 May 2012). "College Word of the Year Contest contenders: Drunkorexia, shmacked and FOMO". The Washington Post. Retrieved 16 November 2012.
- ^ a b Alcohol-Related Psychosis at eMedicine
- ^ Tien AY, Anthony JC (August 1990). "Epidemiological analysis of alcohol and drug use as risk factors for psychotic experiences". The Journal of Nervous and Mental Disease. 178 (8): 473–480. doi:10.1097/00005053-199017880-00001. PMID 2380692.
- ^ Cargiulo T (March 2007). "Understanding the health impact of alcohol dependence". American Journal of Health-System Pharmacy. 64 (5 Suppl 3): S5-11. doi:10.2146/ajhp060647. PMID 17322182.
- ^ Schuckit MA (November 1983). "Alcoholism and other psychiatric disorders". Hospital & Community Psychiatry. 34 (11): 1022–1027. doi:10.1176/ps.34.11.1022. PMID 6642446.
- ^ Monnot, M., Nixon, S., Lovallo, W., & Ross, E. (2001). Altered emotional perception in alcoholics: Deficits in affective prosody comprehension. [Article]. Alcoholism: Clinical and Experimental Research, 25(3), 362–369.
- ^ Taieb O, Corcos M, Loas G, Speranza M, Guilbaud O, Perez-Diaz F, et al. (May 2002). "[Alexithymia and alcohol dependence]". Annales de Médecine Interne. 153 (3 Suppl): 1S51–1S60. PMID 12218885.
- ^ Uekermann J, Daum I (May 2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5). Wiley-Blackwell: 726–735. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
- ^ a b Hendler RA, Ramchandani VA, Gilman J, Hommer DW (2013). "Stimulant and sedative effects of alcohol". Current Topics in Behavioral Neurosciences. 13: 489–509. doi:10.1007/7854_2011_135. ISBN 978-3-642-28719-0. PMID 21560041.
- ^ a b c Dumain T. Pathak N (ed.). "Peptic Ulcer Disease (Stomach Ulcers) Cause, Symptoms, Treatments". Webmd.com. Retrieved 27 April 2013.
- ^ Patel S, Behara R, Swanson GR, Forsyth CB, Voigt RM, Keshavarzian A (October 2015). "Alcohol and the Intestine". Biomolecules. 5 (4): 2573–88. doi:10.3390/biom5042573. PMC 4693248. PMID 26501334.
- ^ Stephens R, Ling J, Heffernan TM, Heather N, Jones K (23 January 2008). "A review of the literature on the cognitive effects of alcohol hangover". Alcohol and Alcoholism. 43 (2): 163–170. doi:10.1093/alcalc/agm160. PMID 18238851.
- ^ "Hangxiety: why alcohol can leave you feeling anxious". Queensland Health. Queensland Health. The State of Queensland. 26 July 2023. Retrieved 2 October 2024.
- ^ a b Pittler MH, Verster JC, Ernst E (December 2005). "Interventions for preventing or treating alcohol hangover: systematic review of randomised controlled trials". BMJ. 331 (7531): 1515–1518. doi:10.1136/bmj.331.7531.1515. PMC 1322250. PMID 16373736.
- ^ "A get-sober pill?". Science News (Paper magazine). 202 (9): 4. 19 November 2022.
- ^ Verster JC, Stephens R, Penning R, Rohsenow D, McGeary J, Levy D, et al. (Alcohol Hangover Research Group) (June 2010). "The alcohol hangover research group consensus statement on best practice in alcohol hangover research". Current Drug Abuse Reviews. 3 (2): 116–126. doi:10.2174/1874473711003020116. PMC 3827719. PMID 20712593.
- ^ Jain A, Yelamanchili VS, Brown KN, Goel A (2024). "Holiday Heart Syndrome". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30725870. Retrieved 15 February 2024.
- ^ "Holiday heart syndrome – definition". Biology-Online.org.
- ^ Rosenthal L, Stokken GT, Smith RH, Daubert JP, Weiss HS, Budzikowski AS (17 October 2021). Talavera F, Compton SJ, Dizon JM (eds.). "Holiday Heart Syndrome: Background, Pathophysiology, Epidemiology". Medscape.
- ^ Ettinger PO, Wu CF, De La Cruz C, Weisse AB, Ahmed SS, Regan TJ (May 1978). "Arrhythmias and the "Holiday Heart": alcohol-associated cardiac rhythm disorders". American Heart Journal. 95 (5): 555–562. doi:10.1016/0002-8703(78)90296-x. PMID 636996.
- ^ Tonelo D, Providência R, Gonçalves L (August 2013). "Holiday heart syndrome revisited after 34 years". Arquivos Brasileiros de Cardiologia. 101 (2): 183–189. doi:10.5935/abc.20130153. PMC 3998158. PMID 24030078.
- ^ Brown KN, Yelamanchili VS, Goel A (2022). "Holiday Heart Syndrome". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 30725870. Retrieved 26 August 2022.
- ^ Money KE, Myles WS (February 1974). "Heavy water nystagmus and effects of alcohol". Nature. 247 (5440): 404–405. Bibcode:1974Natur.247..404M. doi:10.1038/247404a0. PMID 4544739. S2CID 4166559.
- ^ a b Brooks PJ, Enoch MA, Goldman D, Li TK, Yokoyama A (March 2009). "The alcohol flushing response: an unrecognized risk factor for esophageal cancer from alcohol consumption". PLOS Medicine. 6 (3): e50. doi:10.1371/journal.pmed.1000050. PMC 2659709. PMID 19320537.
- ^ McMurran M (3 October 2012). Alcohol-Related Violence: Prevention and Treatment. John Wiley & Sons. p. 37. ISBN 978-1-118-41106-3.
- ^ Adams KE, Rans TS (December 2013). "Adverse reactions to alcohol and alcoholic beverages". Annals of Allergy, Asthma & Immunology. 111 (6): 439–45. doi:10.1016/j.anai.2013.09.016. PMID 24267355.
- ^ "Alcohol Flush Signals Increased Cancer Risk among East Asians". News Release. National Institutes of Health (NIH). 23 March 2009. Archived from the original on 16 February 2012.
- ^ Lee CH, Lee JM, Wu DC, Goan YG, Chou SH, Wu IC, et al. (March 2008). "Carcinogenetic impact of ADH1B and ALDH2 genes on squamous cell carcinoma risk of the esophagus with regard to the consumption of alcohol, tobacco and betel quid". International Journal of Cancer. 122 (6): 1347–1356. doi:10.1002/ijc.23264. PMID 18033686.
- ^ "Unravelling the commercial determinants of health". The Lancet (Editorial). 401 (10383): 1131. 23 March 2023. doi:10.1016/S0140-6736(23)00590-1. PMID 36966781.
- ^ "Just four industries cause 2.7 million deaths in the European Region every year". World Health Organization. 12 June 2024. Retrieved 12 June 2024.
Four corporate products – tobacco, ultra-processed foods, fossil fuels and alcohol – cause 19 million deaths per year globally, or 34% of all deaths.
- ^ Bawden A, Campbell D (12 June 2024). "Tobacco, alcohol, processed foods and fossil fuels 'kill 2.7m a year in Europe'". The Guardian. Retrieved 12 June 2024.
- ^ Mathurin P, Deltenre P (May 2009). "Effect of binge drinking on the liver: an alarming public health issue?". Gut. 58 (5): 613–17. doi:10.1136/gut.2007.145573. PMID 19174416. S2CID 43370272.
- ^ Mekonen T, Chan GC, Connor J, Hall W, Hides L, Leung J (October 2021). "Treatment rates for alcohol use disorders: a systematic review and meta-analysis". Addiction. 116 (10): 2617–2634. doi:10.1111/add.15357. PMID 33245581. S2CID 227180779.
- ^ a b c Butcher JN, Hooley JM, Mineka SM (25 June 2013). Abnormal Psychology. Pearson Education. p. 370. ISBN 978-0-205-97175-6.
- ^ Bakalar N (27 August 2018). "How Much Alcohol Is Safe to Drink? None, Say These Researchers". The New York Times. Retrieved 17 September 2018.
- ^ Kilian C, Manthey J, Carr S, Hanschmidt F, Rehm J, Speerforck S, et al. (May 2021). "Stigmatization of people with alcohol use disorders: An updated systematic review of population studies". Alcoholism: Clinical and Experimental Research. 45 (5): 899–911. doi:10.1111/acer.14598. PMID 33970504.
- ^ Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC (2011). "The stigma of alcohol dependence compared with other mental disorders: a review of population studies". Alcohol and Alcoholism. 46 (2): 105–112. doi:10.1093/alcalc/agq089. PMID 21169612.
- ^ Tomlinson A (26 June 2018). "Tips and Tricks on How to Cut Down on the Booze". The West Australian. Seven West Media (WA). Retrieved 22 March 2019.
- ^ "Alcohol". British Liver Trust. Archived from the original on 11 July 2019. Retrieved 22 March 2019.
- ^ "What to Know About Dry Drunk Syndrome".
- ^ Brook DW, Spitz HI (23 September 2002). The Group Therapy of Substance Abuse. CRC Press. p. 73. ISBN 978-0-7890-1782-6.
- ^ Benton SA (2009). Understanding the High-Functioning Alcoholic – Professional Views and Personal Insights. Greenwood Publishing Group. ISBN 978-0-313-35280-5.
- ^ Brody J (4 May 2009). "High Functioning, but Still Alcoholics". The New York Times. Retrieved 18 February 2012.
- ^ "What is a High Functioning Alcoholic? | Definition & Signs". Alcohol.org. Retrieved 29 January 2021.
- ^ Szlemko WJ, Wood JW, Thurman PJ (October 2006). "Native Americans and alcohol: past, present, and future". The Journal of General Psychology. 133 (4). Heldref Publications: 435–451. doi:10.3200/GENP.133.4.435-451. PMID 17128961. S2CID 43082343.
- ^ a b Arts NJ, Walvoort SJ, Kessels RP (27 November 2017). "Korsakoff's syndrome: a critical review". Neuropsychiatric Disease and Treatment. 13: 2875–2890. doi:10.2147/NDT.S130078. PMC 5708199. PMID 29225466.
- ^ Ridley NJ, Draper B, Withall A (25 January 2013). "Alcohol-related dementia: an update of the evidence". Alzheimer's Research & Therapy. 5 (1): 3. doi:10.1186/alzrt157. PMC 3580328. PMID 23347747.
- ^ synd/2922 at Who Named It?
- ^ E. Marchiafava, A. Bignami. Sopra un'alterazione del corpo calloso osservata da sogetti alcoolisti. Rivista di patologia nervosa e mentale, 1903, 8 (12): 544–549.
- ^ Raina, Sujeet & M Mahesh, D & Mahajan, J & S Kaushal, S & Gupta, D & Dhiman, Dalip. (2008). MarchiafavaBignami Disease. The Journal of the Association of Physicians of India. 56. 633-5.
- ^ Bruha R, Dvorak K, Petrtyl J (March 2012). "Alcoholic liver disease". World Journal of Hepatology. 4 (3): 81–90. doi:10.4254/wjh.v4.i3.81. PMC 3321494. PMID 22489260.
- ^ 15th Report on Carcinogens. National Toxicology Program (NTP) (Report). doi:10.22427/ntp-other-1003. S2CID 245412518.
- ^ Hashibe M, Brennan P, Chuang SC, Boccia S, Castellsague X, Chen C, et al. (February 2009). "Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium". Cancer Epidemiology, Biomarkers & Prevention. 18 (2): 541–550. doi:10.1158/1055-9965.EPI-08-0347. PMC 3051410. PMID 19190158.
- ^ Petticrew M, Maani Hessari N, Knai C, Weiderpass E (March 2018). "How alcohol industry organisations mislead the public about alcohol and cancer" (PDF). Drug and Alcohol Review. 37 (3): 293–303. doi:10.1111/dar.12596. PMID 28881410.
- ^ a b Piano MR (2017). "Alcohol's Effects on the Cardiovascular System". Alcohol Research. 38 (2): 219–241. PMC 5513687. PMID 28988575.
- ^ Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G (March 2010). "Alcohol consumption and mortality in patients with cardiovascular disease: a meta-analysis". Journal of the American College of Cardiology. 55 (13): 1339–1347. doi:10.1016/j.jacc.2010.01.006. PMID 20338495.
- ^ "Alcohol and Heart Health". American Heart Association. 15 August 2014.
- ^ Arora M, ElSayed A, Beger B, Naidoo P, Shilton T, Jain N, et al. (2022). "The Impact of Alcohol Consumption on Cardiovascular Health: Myths and Measures" (PDF). Global Heart. 17 (1): 45. doi:10.5334/gh.1132. PMC 9306675. PMID 36051324.
- ^ a b Salamon M (May 2022). "Want a healthier heart? Seriously consider skipping the drinks". Harvard Health.
- ^ Piano MR (May 2002). "Alcoholic cardiomyopathy: incidence, clinical characteristics, and pathophysiology". Chest. 121 (5): 1638–1650. doi:10.1378/chest.121.5.1638. PMC 1923411. PMID 12006456.
- ^ a b Bellé M, Sartori Sd, Rossi AG (January 2007). "Alcoholism: effects on the cochleo-vestibular apparatus". Brazilian Journal of Otorhinolaryngology. 73 (1): 110–116. doi:10.1016/s1808-8694(15)31132-0. PMC 9443585. PMID 17505609.
- ^ Upile T, Sipaul F, Jerjes W, Singh S, Nouraei SA, El Maaytah M, et al. (September 2007). "The acute effects of alcohol on auditory thresholds". BMC Ear, Nose and Throat Disorders. 7: 4. doi:10.1186/1472-6815-7-4. PMC 2031886. PMID 17877829.
- ^ Qian P, Zhao Z, Liu S, Xin J, Liu Y, Hao Y, et al. (2023). "Alcohol as a risk factor for hearing loss: A systematic review and meta-analysis". PLOS ONE. 18 (1): e0280641. Bibcode:2023PLoSO..1880641Q. doi:10.1371/journal.pone.0280641. PMC 9858841. PMID 36662896.
- ^ Ashworth M, Gerada C (August 1997). "ABC of mental health. Addiction and dependence – II: Alcohol". BMJ. 315 (7104): 358–360. doi:10.1136/bmj.315.7104.358. PMC 2127236. PMID 9270461.
- ^ Fisher GL, Roget NA, eds. (2009). "Withdrawal: Alcohol". Encyclopedia of substance abuse prevention, treatment, & recovery. Los Angeles: SAGE. p. 1005. ISBN 978-1-4522-6601-5. Archived from the original on 22 December 2015.
- ^ McClure EA, Gipson CD, Malcolm RJ, Kalivas PW, Gray KM (2014). "Potential role of N-acetylcysteine in the management of substance use disorders". CNS Drugs. 28 (2): 95–106. doi:10.1007/s40263-014-0142-x. PMC 4009342. PMID 24442756.
- ^ Qu L, Ma XP, Simayi A, Wang XL, Xu GP (May 2024). "Comparative efficacy of various pharmacologic treatments for alcohol withdrawal syndrome: a systematic review and network meta-analysis". International Clinical Psychopharmacology. 39 (3): 148–162. doi:10.1097/YIC.0000000000000526. PMID 38170803.
- ^ Gillman M.A, Lichtigfeld, F.J. 2004 Enlarged double-blind randomised trial of benzodiazepines against psychotropic analgesic nitrous oxide for alcohol withdrawal, Addictive Behaviors, Volume 29, Issue 6, Pages 1183–1187
- ^ Ebrahimpour-Koujan S, Saneei P, Larijani B, Esmaillzadeh A (2020). "Consumption of sugar sweetened beverages and dietary fructose in relation to risk of gout and hyperuricemia: a systematic review and meta-analysis". Critical Reviews in Food Science and Nutrition. 60 (1): 1–10. doi:10.1080/10408398.2018.1503155. PMID 30277800. S2CID 52909165.
- ^ Singh JA, Reddy SG, Kundukulam J (March 2011). "Risk factors for gout and prevention: a systematic review of the literature". Current Opinion in Rheumatology. 23 (2): 192–202. doi:10.1097/BOR.0b013e3283438e13. PMC 4104583. PMID 21285714.
- ^ Roddy E, Mallen CD, Doherty M (October 2013). "Gout". BMJ. 347 (oct01 3): f5648. doi:10.1136/bmj.f5648. PMID 24473446. S2CID 220212466.
- ^ Allison MG, McCurdy MT (May 2014). "Alcoholic metabolic emergencies". Emergency Medicine Clinics of North America. 32 (2): 293–301. doi:10.1016/j.emc.2013.12.002. PMID 24766933.
- ^ Howard RD, Bokhari SR (January 2019). Alcoholic Ketoacidosis (AKA). PMID 28613672.
- ^ a b McGuire LC, Cruickshank AM, Munro PT (June 2006). "Alcoholic ketoacidosis". Emergency Medicine Journal. 23 (6): 417–420. doi:10.1136/emj.2004.017590. PMC 2564331. PMID 16714496.
- ^ Palzes VA, Parthasarathy S, Chi FW, Kline-Simon AH, Lu Y, Weisner C, et al. (December 2020). "Associations Between Psychiatric Disorders and Alcohol Consumption Levels in an Adult Primary Care Population". Alcoholism: Clinical and Experimental Research. 44 (12): 2536–2544. doi:10.1111/acer.14477. PMC 7756330. PMID 33151592.
- ^ Jané-Llopis E, Matytsina I (November 2006). "Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs". Drug and Alcohol Review. 25 (6): 515–536. doi:10.1080/09595230600944461. PMID 17132571.
- ^ Shi X, Li M, Yao J, Li MD, Yang Z (July 2024). "Alcohol drinking, DNA methylation and psychiatric disorders: A multi-omics Mendelian randomization study to investigate causal pathways". Addiction. 119 (7): 1226–1237. doi:10.1111/add.16465. PMID 38523595.
- ^ Georgiadou SP, Manoulakas E, Makaritsis KP, Dalekos GN (May 2018). "A chronic alcoholic man with high fever, neck rigidity and loss of consciousness: remember the Austrian syndrome a commonly unrecognised invasive pneumococcus triad". BMJ Case Reports. 2018: bcr–2018–225010. doi:10.1136/bcr-2018-225010. PMC 5976089. PMID 29848535.
- ^ Starek-Świechowicz B, Budziszewska B, Starek A (February 2023). "Alcohol and breast cancer". Pharmacological Reports. 75 (1): 69–84. doi:10.1007/s43440-022-00426-4. PMC 9889462. PMID 36310188.
- ^ "Shouldn't we know this already? The link between alcohol and breast cancer". www.who.int.
- ^ "Alcohol". Drugs and Lactation Database (LactMed) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development. September 2024. PMID 30000529.
- ^ "Neonatal abstinence Syndrome". MedlinePlus. US Library of Medicine. 2017. Retrieved 27 July 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ Ghazanfarpour M, Najafi MN, Roozbeh N, Mashhadi ME, Keramat-Roudi A, Mégarbane B, et al. (June 2019). "Therapeutic approaches for neonatal abstinence syndrome: a systematic review of randomized clinical trials". Daru: Journal of Faculty of Pharmacy, Tehran University of Medical Sciences. 27 (1): 423–431. doi:10.1007/s40199-019-00266-3. PMC 6593026. PMID 31093953.
- ^ Ko JY, Wolicki S, Barfield WD, Patrick SW, Broussard CS, Yonkers KA, et al. (2017). "CDC Grand Rounds: Public Health Strategies to Prevent Neonatal Abstinence Syndrome". MMWR. Morbidity and Mortality Weekly Report. 66 (9): 242–245. doi:10.15585/mmwr.mm6609a2. PMC 5687191. PMID 28278146.
- ^ Meyrel M, Rolland B, Geoffroy PA (April 2020). "Alterations in circadian rhythms following alcohol use: A systematic review". Progress in Neuro-Psychopharmacology & Biological Psychiatry. 99: 109831. doi:10.1016/j.pnpbp.2019.109831. PMID 31809833.
- ^ "What Causes Insomnia?". NHLBI. 13 December 2011. Archived from the original on 28 July 2016. Retrieved 9 August 2016.
- ^ "Restless Legs Syndrome Fact Sheet". National Institute of Neurological Disorders and Stroke. Archived from the original on 28 July 2017. Retrieved 7 July 2019.
- ^ "Sleep Apnea - Causes and Risk Factors". National Heart, Lung, and Blood Institute (NHLBI). 24 March 2022. Archived from the original on 6 February 2024. Retrieved 6 February 2024.
- ^ Nimish V (June 2021). "Gastritis - Digestive Disorders". MSD Manual Consumer Version. Merck & Co. Archived from the original on 13 August 2021. Retrieved 25 February 2022.
- ^ "Gastritis". The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). 27 November 2013. Archived from the original on 6 March 2015. Retrieved 1 March 2015.
- ^ Rehm J, Samokhvalov AV, Neuman MG, Room R, Parry C, Lönnroth K, et al. (December 2009). "The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review". BMC Public Health. 9: 450. doi:10.1186/1471-2458-9-450. PMC 2796667. PMID 19961618.
- ^ Lönnroth K, Williams BG, Stadlin S, Jaramillo E, Dye C (August 2008). "Alcohol use as a risk factor for tuberculosis - a systematic review". BMC Public Health. 8: 289. doi:10.1186/1471-2458-8-289. PMC 2533327. PMID 18702821.
- ^ Sorkin T, Sheppard MN (September 2017). "Sudden unexplained death in alcohol misuse (SUDAM) patients have different characteristics to those who died from sudden arrhythmic death syndrome (SADS)". Forensic Science, Medicine, and Pathology. 13 (3): 278–283. doi:10.1007/s12024-017-9877-2. PMC 5554285. PMID 28668989.
- ^ Sveinsson O, Andersson T, Mattsson P, Carlsson S, Tomson T (January 2020). "Clinical risk factors in SUDEP: A nationwide population-based case-control study". Neurology. 94 (4): e419–e429. doi:10.1212/WNL.0000000000008741. PMC 7079690. PMID 31831600.
- ^ Ricci E, Al Beitawi S, Cipriani S, Candiani M, Chiaffarino F, Viganò P, et al. (January 2017). "Semen quality and alcohol intake: a systematic review and meta-analysis". Reproductive Biomedicine Online. 34 (1): 38–47. doi:10.1016/j.rbmo.2016.09.012. PMID 28029592.
- ^ Klop B, do Rego AT, Cabezas MC (August 2013). "Alcohol and plasma triglycerides". Current Opinion in Lipidology. 24 (4): 321–326. doi:10.1097/MOL.0b013e3283606845. PMID 23511381.
- ^ "Pancreatitis". A.D.A.M., Inc. Archived from the original on 30 December 2012. Retrieved 5 January 2013.
- ^ Apte MV, Pirola RC, Wilson JS (June 2009). "Pancreas: alcoholic pancreatitis—it's the alcohol, stupid". Nature Reviews. Gastroenterology & Hepatology. 6 (6): 321–2. doi:10.1038/nrgastro.2009.84. PMID 19494819. S2CID 6580794.
- Lay summary in: Apte MV, Pirola RC, Wilson JS. "Pancreas: Alcoholic Pancreatitis—It's the Alcohol, Stupid". Medscape Today.
- ^ Yadav D, Hawes RH, Brand RE, Anderson MA, Money ME, Banks PA, et al. (June 2009). "Alcohol consumption, cigarette smoking, and the risk of recurrent acute and chronic pancreatitis". Archives of Internal Medicine. 169 (11): 1035–45. doi:10.1001/archinternmed.2009.125. PMC 6785300. PMID 19506173.
- ^ "Pancreatitis Explained". Better Health Channel. State Government of Victoria. 2011. Archived from the original on 13 May 2010.
- ^ Johnson CD, Hosking S (November 1991). "National statistics for diet, alcohol consumption, and chronic pancreatitis in England and Wales, 1960–88". Gut. 32 (11): 1401–5. doi:10.1136/gut.32.11.1401. PMC 1379177. PMID 1752477.
- ^ Porphyria Cutanea Tarda at eMedicine
- ^ Hart MG, Hooper G (July 2005). "Clinical associations of Dupuytren's disease". Postgraduate Medical Journal. 81 (957): 425–428. doi:10.1136/pgmj.2004.027425. PMC 1743313. PMID 15998816.
- ^ Burge P, Hoy G, Regan P, Milne R (March 1997). "Smoking, alcohol and the risk of Dupuytren's contracture". The Journal of Bone and Joint Surgery. British Volume. 79 (2): 206–210. doi:10.1302/0301-620x.79b2.6990. PMID 9119843.
- ^ Cardet JC, White AA, Barrett NA, Feldweg AM, Wickner PG, Savage J, et al. (2014). "Alcohol-induced respiratory symptoms are common in patients with aspirin exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. In Practice. 2 (2): 208–13. doi:10.1016/j.jaip.2013.12.003. PMC 4018190. PMID 24607050.
- ^ Wei B, Liu Y, Li H, Peng Y, Luo Z (February 2023). "Impact of alcohol consumption on coronavirus disease 2019 severity: A systematic review and meta-analysis". Journal of Medical Virology. 95 (2): e28547. doi:10.1002/jmv.28547. PMID 36734064.
- ^ Park SH, Kim DJ (October 2020). "Global and regional impacts of alcohol use on public health: Emphasis on alcohol policies". Clinical and Molecular Hepatology. 26 (4): 652–661. doi:10.3350/cmh.2020.0160. PMC 7641561. PMID 33053937.
- ^ Iida-Ueno A, Enomoto M, Tamori A, Kawada N (April 2017). "Hepatitis B virus infection and alcohol consumption". World Journal of Gastroenterology. 23 (15): 2651–2659. doi:10.3748/wjg.v23.i15.2651. PMC 5403744. PMID 28487602.
- ^ Maintz L, Novak N (May 2007). "Histamine and histamine intolerance". The American Journal of Clinical Nutrition. 85 (5): 1185–1196. doi:10.1093/ajcn/85.5.1185. PMID 17490952.
- ^ Kushner MG, Abrams K, Borchardt C (March 2000). "The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings". Clinical Psychology Review. 20 (2): 149–171. doi:10.1016/s0272-7358(99)00027-6. PMID 10721495.
- ^ Castillo-Carniglia A, Keyes KM, Hasin DS, Cerdá M (December 2019). "Psychiatric comorbidities in alcohol use disorder". The Lancet. Psychiatry. 6 (12): 1068–1080. doi:10.1016/S2215-0366(19)30222-6. PMC 7006178. PMID 31630984.
- ^ Kessler RC (November 2004). "The epidemiology of dual diagnosis". Biological Psychiatry. 56 (10): 730–737. doi:10.1016/j.biopsych.2004.06.034. PMID 15556117.
- ^ Puddephatt JA, Irizar P, Jones A, Gage SH, Goodwin L (June 2022). "Associations of common mental disorder with alcohol use in the adult general population: a systematic review and meta-analysis". Addiction. 117 (6): 1543–1572. doi:10.1111/add.15735. PMC 9300028. PMID 34729837.
- ^ Greydanus DE, Shek D (September 2009). "Deliberate self-harm and suicide in adolescents". The Keio Journal of Medicine. 58 (3): 144–151. doi:10.2302/kjm.58.144. hdl:10397/4495. PMID 19826208.
- ^ Bolton J, Cox B, Clara I, Sareen J (November 2006). "Use of alcohol and drugs to self-medicate anxiety disorders in a nationally representative sample". The Journal of Nervous and Mental Disease. 194 (11): 818–825. doi:10.1097/01.nmd.0000244481.63148.98. PMID 17102705. S2CID 7515999.
- ^ Peters GL, Rosselli JL, Kerr JL. "Overview of Peptic Ulcer Disease: Etiology and Pathophysiology". Medscape.com. Retrieved 27 April 2013.
- ^ D'Souza S, Mayock S, Salt A (December 2017). "A review of in vivo and in vitro aspects of alcohol-induced dose dumping". AAPS Open. 3 (1). doi:10.1186/s41120-017-0014-9. ISSN 2364-9534.
- ^ a b c Yost DA (2002). "Acute care for alcohol intoxication" (PDF). Postgraduate Medicine Online. 112 (6). Archived from the original (PDF) on 14 December 2010. Retrieved 29 September 2007.
- ^ Lukas SE, Orozco S (October 2001). "Ethanol increases plasma Delta(9)-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers". Drug and Alcohol Dependence. 64 (2): 143–9. doi:10.1016/S0376-8716(01)00118-1. PMID 11543984.
- ^ TOMSO entry in PiHKAL
- ^ "Harmful Interactions". National Institute on Alcohol Abuse and Alcoholism (NIAAA).
- ^ Repchinsky C (ed.) (2012). Compendium of pharmaceuticals and specialties, Ottawa: Canadian Pharmacists Association.[full citation needed]
- ^ "Alcohol & Diabetes – ADA". American Diabetes Association. Retrieved 30 November 2022.
- ^ Agrawal N (June 1991). "Risk factors for gastrointestinal ulcers caused by nonsteroidal anti-inflammatory drugs (NSAIDs)". The Journal of Family Practice. 32 (6): 619–624. PMID 2040888.
- ^ "Aspirin information from Drugs.com". Drugs.com. Archived from the original on 9 May 2008. Retrieved 8 May 2008.
- ^ "Oral Aspirin information". First DataBank. Archived from the original on 18 September 2000. Retrieved 8 May 2008.
- ^ Curran CP, Marczinski CA (December 2017). "Taurine, caffeine, and energy drinks: Reviewing the risks to the adolescent brain". Birth Defects Research. 109 (20): 1640–1648. doi:10.1002/bdr2.1177. PMC 5737830. PMID 29251842.
- ^ Arria AM, Caldeira KM, Kasperski SJ, O'Grady KE, Vincent KB, Griffiths RR, et al. (June 2010). "Increased alcohol consumption, nonmedical prescription drug use, and illicit drug use are associated with energy drink consumption among college students". Journal of Addiction Medicine. 4 (2): 74–80. doi:10.1097/ADM.0b013e3181aa8dd4. PMC 2923814. PMID 20729975.
- ^ "Energy drinks and risk to future substance use". www.drugabuse.gov. National Institute on Drug Abuse. 8 August 2017. Archived from the original on 18 February 2020. Retrieved 29 March 2019.
- ^ Laizure SC, Mandrell T, Gades NM, Parker RB (January 2003). "Cocaethylene metabolism and interaction with cocaine and ethanol: role of carboxylesterases". Drug Metabolism and Disposition. 31 (1): 16–20. doi:10.1124/dmd.31.1.16. PMID 12485948.
- ^ Pergolizzi J, Breve F, Magnusson P, LeQuang JA, Varrassi G (February 2022). "Cocaethylene: When Cocaine and Alcohol Are Taken Together". Cureus. 14 (2): e22498. doi:10.7759/cureus.22498. PMC 8956485. PMID 35345678.
- ^ Markowitz JS, Logan BK, Diamond F, Patrick KS (August 1999). "Detection of the novel metabolite ethylphenidate after methylphenidate overdose with alcohol coingestion". Journal of Clinical Psychopharmacology. 19 (4): 362–6. doi:10.1097/00004714-199908000-00013. PMID 10440465.
- ^ Markowitz JS, DeVane CL, Boulton DW, Nahas Z, Risch SC, Diamond F, et al. (June 2000). "Ethylphenidate formation in human subjects after the administration of a single dose of methylphenidate and ethanol". Drug Metabolism and Disposition. 28 (6): 620–4. PMID 10820132.
- ^ Verplaetse TL, McKee SA (March 2017). "An overview of alcohol and tobacco/nicotine interactions in the human laboratory". The American Journal of Drug and Alcohol Abuse. 43 (2): 186–196. doi:10.1080/00952990.2016.1189927. PMC 5588903. PMID 27439453.
- ^ McCoy HG, Cipolle RJ, Ehlers SM, Sawchuk RJ, Zaske DE (November 1979). "Severe methanol poisoning. Application of a pharmacokinetic model for ethanol therapy and hemodialysis". The American Journal of Medicine. 67 (5): 804–7. doi:10.1016/0002-9343(79)90766-6. PMID 507092.
- ^ Weathermon R, Crabb DW (1999). "Alcohol and medication interactions". Alcohol Research & Health. 23 (1): 40–54. PMC 6761694. PMID 10890797.
- ^ "PRODUCT INFORMATION COUMADIN" (PDF). TGA eBusiness Services. Aspen Pharma Pty Ltd. 19 January 2010. Archived from the original on 17 October 2015. Retrieved 11 December 2013.
- ^ "Warfarin Anticoagulant Medication". Archived from the original on 1 July 2020. Retrieved 30 June 2020.
- ^ "Isoniazid tablet". DailyMed. 18 October 2018. Archived from the original on 13 March 2019. Retrieved 24 January 2020.
- ^ Saukkonen JJ, Cohn DL, Jasmer RM, Schenker S, Jereb JA, Nolan CM, et al. (October 2006). "An official ATS statement: hepatotoxicity of antituberculosis therapy". American Journal of Respiratory and Critical Care Medicine. 174 (8): 935–952. doi:10.1164/rccm.200510-1666ST. PMID 17021358. S2CID 36384722.
- ^ a b Lobo IA, Harris RA (July 2008). "GABA(A) receptors and alcohol". Pharmacology Biochemistry and Behavior. 90 (1): 90–94. doi:10.1016/j.pbb.2008.03.006. PMC 2574824. PMID 18423561.
- ^ "Acetate, Ion chromatography standard solution, Safety Data Sheet". Thermo Fisher Scientific. 1 April 2024. p. 4.
- ^ Maxwell CR, Spangenberg RJ, Hoek JB, Silberstein SD, Oshinsky ML (December 2010). "Acetate causes alcohol hangover headache in rats". PLOS ONE. 5 (12): e15963. Bibcode:2010PLoSO...515963M. doi:10.1371/journal.pone.0015963. PMC 3013144. PMID 21209842.
- ^ 'Is coffee the real cure for a hangover?' by Bob Holmes, New Scientist, Jan. 15 2011, p. 17.
- ^ Narahashi T, Kuriyama K, Illes P, Wirkner K, Fischer W, Mühlberg K, et al. (May 2001). "Neuroreceptors and ion channels as targets of alcohol". Alcoholism: Clinical and Experimental Research. 25 (5 Suppl ISBRA): 182S–188S. doi:10.1097/00000374-200105051-00030. PMID 11391069.
- ^ Olsen RW, Li GD, Wallner M, Trudell JR, Bertaccini EJ, Lindahl E, et al. (March 2014). "Structural models of ligand-gated ion channels: sites of action for anesthetics and ethanol". Alcoholism: Clinical and Experimental Research. 38 (3): 595–603. doi:10.1111/acer.12283. PMC 3959612. PMID 24164436.
- ^ Charlet K, Beck A, Heinz A (2013). "The dopamine system in mediating alcohol effects in humans". Current Topics in Behavioral Neurosciences. 13: 461–88. doi:10.1007/7854_2011_130. ISBN 978-3-642-28719-0. PMID 21533679.
- ^ Méndez M, Morales-Mulia M (June 2008). "Role of mu and delta opioid receptors in alcohol drinking behaviour". Current Drug Abuse Reviews. 1 (2): 239–52. doi:10.2174/1874473710801020239. PMID 19630722.
- ^ Tillonen J. Ethanol, acetaldehyde and gastrointestinal flora (PDF) (Ph.D. thesis). Helsingin Yliopisto.
- ^ "Drunkest driver in SA arrested". SowetanLIVE. Retrieved 12 April 2024.
- ^ Zaridze D, Brennan P, Boreham J, Boroda A, Karpov R, Lazarev A, et al. (June 2009). "Alcohol and cause-specific mortality in Russia: a retrospective case-control study of 48,557 adult deaths". Lancet. 373 (9682): 2201–2214. doi:10.1016/S0140-6736(09)61034-5. PMC 2715218. PMID 19560602.
- ^ US Drug Enforcement Administration (May 2003). "Speaking Out Against Drug Legalization" (PDF). U.S. Department of Justice. Archived from the original (PDF) on 27 June 2006. Retrieved 21 October 2016.
- ^ Mokdad AH, Marks JS, Stroup DF, Gerberding JL (March 2004). "Actual causes of death in the United States, 2000" (PDF). JAMA. 291 (10): 1238–45. doi:10.1001/jama.291.10.1238. PMID 15010446. Archived from the original (PDF) on 17 September 2011.
- ^ NIAAA (August 2001). "Number of deaths and age-adjusted death rates per 100,000 population for categories of alcohol-related (A-R) mortality, United States and States, 1979–96". Database Resources / Statistical Tables. National Institute on Alcohol Abuse and Alcoholism (NIAAA). Archived from the original on 7 August 2007. Retrieved 20 October 2007.
- ^ Guillén-Mancina E, Calderón-Montaño JM, López-Lázaro M (February 2018). "Avoiding the ingestion of cytotoxic concentrations of ethanol may reduce the risk of cancer associated with alcohol consumption". Drug and Alcohol Dependence. 183: 201–204. doi:10.1016/j.drugalcdep.2017.11.013. PMID 29289868.
- ^ Lieber CS (1990). "Mechanism of ethanol induced hepatic injury". Pharmacology & Therapeutics. 46 (1): 1–41. doi:10.1016/0163-7258(90)90032-w. PMID 2181486.
- ^ Brust JC (April 2010). "Ethanol and cognition: indirect effects, neurotoxicity and neuroprotection: a review". International Journal of Environmental Research and Public Health. 7 (4): 1540–57. doi:10.3390/ijerph7041540. PMC 2872345. PMID 20617045.
- ^ "Hornets can hold their alcohol like no other animal on Earth". New Scientist.
- ^ Lachenmeier DW, Rehm J (January 2015). "Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach". Scientific Reports. 5: 8126. doi:10.1038/srep08126. PMC 4311234. PMID 25634572.
- ^ Clark J, Farmer S, Kennepohl D, Kabrhel J, Ashenhurst J, Ashenhurst J (26 August 2015). "17.7: Oxidation of Alcohols". Chemistry LibreTexts.
- ^ Burcham PC (19 November 2013). An Introduction to Toxicology. Springer Science & Business Media. pp. 42–. ISBN 978-1-4471-5553-9.
- ^ "Distillation: Some Purity Considerations". Moonshine Still. Retrieved 5 May 2015.
- ^ Blumenthal P, Steger MC, Einfalt D, Rieke-Zapp J, Quintanilla Bellucci A, Sommerfeld K, et al. (April 2021). "Methanol Mitigation during Manufacturing of Fruit Spirits with Special Consideration of Novel Coffee Cherry Spirits". Molecules. 26 (9): 2585. doi:10.3390/molecules26092585. PMC 8125215. PMID 33925245.
- ^ Ma HL, Yang XP, Zuo Y (15 April 2006). "Study on Method of Decreasing Methanol in Apple Pomace Spirit". Food Science. 27 (4): 138–142.
- ^ "Redefine alcohol: WHO's urgent call for Europe to rethink alcohol's place in society". www.who.int.
- ^ "What Is Intermittent Sobriety—and Why Is Everyone Talking About It Right Now?". Real Simple.
- ^ "Are You Trying 'Sober October'? Experts Reveal the Surprising Benefits of 'Intermittent Sobriety'". Health.
- ^ Goddiksen MK (4 January 2023). "Sober Curious er det nye sort'" [Sober Curious is the new kind] (in Danish).
- ^ Moore MH, Gerstein DR (1981). Alcohol and Public Policy. National Academies. pp. 90–93.
- ^ "Marijuana Research Report:Is marijuana a gateway drug?". National Institute on Drug Abuse. July 2020. Retrieved 7 November 2020.
- ^ Kirby T, Barry AE (2012). "Alcohol as a gateway drug: A study of US 12th graders" (PDF). Journal of School Health. 82 (8): 371–9. doi:10.1111/j.1746-1561.2012.00712.x. PMID 22712674. Archived from the original (PDF) on 4 June 2016. Retrieved 26 May 2016.
- ^ Vidrih R, Hribar J (2016), Kristbergsson K, Oliveira J (eds.), "Mead: The Oldest Alcoholic Beverage", Traditional Foods, Boston, MA: Springer US, pp. 325–338, doi:10.1007/978-1-4899-7648-2_26, ISBN 978-1-4899-7646-8, retrieved 19 December 2024
- ^ Eger II EI, Saidman LJ, Westhorpe RN (14 September 2013). The Wondrous Story of Anesthesia. Springer Science & Business Media. pp. 4–. ISBN 978-1-4614-8441-7. Archived from the original on 18 September 2017.
- ^ Shah JB (September 2011). "The history of wound care". The Journal of the American College of Certified Wound Specialists. 3 (3): 65–66. doi:10.1016/j.jcws.2012.04.002. PMC 3601883. PMID 24525756.
- ^ John Gill's Exposition of the Bible Classic Bible Commentaries
- ^ "Dutch". Oxford English Dictionary (2nd ed.). Oxford University Press. 1989.
- ^ Byrne E (26 July 2013). "What is the origin of the phrase 'Dutch Courage'?". History Extra. Retrieved 26 December 2022.
- ^ Martin G. "Dutch courage". Phrases. UK. Retrieved 26 December 2022.
- ^ "History of Alcohol" (PDF). Archived from the original (PDF) on 21 August 2013. Retrieved 11 May 2015.
- ^ "Gin Act". Britannica Online Encyclopedia.
- ^ "Motbok" [Counter book]. Förvaltningshistorisk ordbok [Administrative history dictionary] (in Swedish). Retrieved 3 November 2022.
- ^ Arjakas K (8 November 2008). "Alkoholikeeldudest Eestis" [Alcohol bans in Estonia]. Postimees (in Estonian). Retrieved 27 March 2024.
Further reading
[edit]- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (1988). Alcohol Drinking. International Agency for Research on Cancer.
External links
[edit]- "ETOH Database Search". hazelden.org.
- The National Institute on Alcohol Abuse and Alcoholism maintains a database of alcohol-related health effects. ETOH Archival Database (1972–2003) Alcohol and Alcohol Problems Science Database.
- "Harmful Interactions". National Institute on Alcohol Abuse and Alcoholism (NIAAA).
- WHO fact sheet on alcohol
- ChEBI – biology related
- Kyoto Encyclopedia of Genes and Genomes signal transduction pathway: KEGG – human alcohol addiction
- 5-HT3 agonists
- AMPA receptor antagonists
- Adenosine reuptake inhibitors
- Alcohol-related crimes
- Alcohol
- Alcohol abuse
- Alcohol and health
- Alcohol dehydrogenase inhibitors
- Alcohol law
- Alcohols
- Analgesics
- Anaphrodisia
- Anxiolytics
- Calcium channel blockers
- Chemical hazards
- Depressogens
- Diuretics
- Drinking culture
- Drug culture
- Drugs acting on the nervous system
- Drugs with unknown mechanisms of action
- Emetics
- Ethanol
- Euphoriants
- GABAA receptor positive allosteric modulators
- General anesthetics
- Glycine reuptake inhibitors
- Hepatotoxins
- Human metabolites
- Hypnotics
- IARC Group 1 carcinogens
- Kainate receptor antagonists
- NMDA receptor antagonists
- Neurotoxins
- Nicotinic agonists
- Ototoxicity
- Psychoactive drugs
- Sedatives
- Teratogens


