PDGFRB
Platelet-derived growth factor receptor beta is a protein that in humans is encoded by the PDGFRB gene. Mutations in PDGFRB are mainly associated with the clonal eosinophilia class of malignancies.
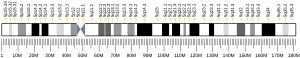
Gene
[edit]The PDGFRB gene is located on human chromosome 5 at position q32 (designated as 5q32) and contains 25 exons. The gene is flanked by the genes for granulocyte-macrophage colony-stimulating factor and Colony stimulating factor 1 receptor (also termed macrophage-colony stimulating factor receptor), all three of which may be lost together by a single deletional mutation thereby causing development of the 5q-syndrome.[5] Other genetic abnormalities in PDGFRB lead to various forms of potentially malignant bone marrow disorders: small deletions in and chromosome translocations causing fusions between PDGFRB and any one of at least 30 genes can cause Myeloproliferative neoplasms that commonly involve eosinophilia, eosinophil-induced organ injury, and possible progression to aggressive leukemia (see blow).[6]
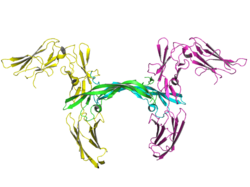
Structure
[edit]The PDGFRB gene encodes a typical receptor tyrosine kinase, which belongs to the type III tyrosine kinase receptor (RTK) family and is structurally characterized by five extracellular immunoglobulin-like domains, a single membrane-spanning helix domain, an intracellular juxtamembrane domain, a split tyrosine kinase domain and a carboxylic tail.[7] In the absence of ligand, PDGFRβ adopts an inactive conformation in which the activation loop folds over the catalytic site, the juxtamembrane region over a loop occluding the active site and the carboxy-terminal tail over the kinase domain. Upon PDGF binding the dimerization of receptor releases the inhibitory conformations due to auto-phosphorylation of regulatory tyrosine residues in trans fashion. Tyrosine residues 857 and 751 are major phosphorylation sites for the activation of PDGFRβ.[8]
The molecular mass of the mature, glycosylated PDGFRβ protein is approximately 180 kDa.
Modes of activation
[edit]Activation of PDGFRβ requires de-repression of the receptor's kinase activity. The ligand for PDGFRβ (PDGF) accomplishes this in the course of assembling a PDGFRβ dimer. Two of the five PDGF isoforms activate PDGFRβ (PDGF-B and PDGF-D). The activated receptor phosphorylates itself and other proteins, and thereby engages intracellular signaling pathways that trigger cellular responses such as migration and proliferation. There are also PDGF-independent modes of de-repressing the PDGFRβ's kinase activity and hence activating it. For instance, forcing PDGFRβ into close proximity of each other by overexpression or with antibodies directed against the extracellular domain. Alternatively, mutations in the kinase domain that stabilize a kinase active conformation result in constitutive activation.
Unlike PDGFRα, PDGFRβ cannot be indirectly activated. This is because PDGFRβ recruits RasGAP and thereby attenuates Ras/PI3K activity, which is required to engage a feed-forward loop that is responsible for this mode of activation.[9][10]
Role in physiology/pathology
[edit]The phenotype of knock out mice demonstrates that PDGFRB is essential for vascular development, and that PDGFRB is responsible for activating PDGFRβ during embryogenesis. Eliminating either PDGFRB, or PDGF-B reduces the number of pericytes and vascular smooth muscle cells, and thereby compromises the integrity and/or functionality of the vasculature in multiple organs, including the brain, heart, kidney, skin and eye.[11][12][13][14]
In vitro studies using cultured cells indicate that endothelial cells secrete PDGF, which recruits PDGFRβ-expressing pericytes that stabilize nascent blood vessels.[15] Mice harboring a single activated allele of PDGFRB show a number of postnatal phenotypes including reduced differentiation of aortic vascular smooth muscle cells and brain pericytes. Similarly, differentiation of adipose from pericytes and mesenchymal cells is suppressed.[16] Misregulation of the PDGFRβ's kinase activity (typically activation) contributes to endemic diseases such as cancer and cardiovascular disease.[17][18][19]
PDGFRB mutations
[edit]5q- Syndrome
[edit]Human chromosome 5 deletions that remove three adjacent genes, those for granulocyte-macrophage colony-stimulating factor, PDGFRB, and Colony stimulating factor 1 receptor, cause the Chromosome 5q deletion syndrome (5q- syndrome). This syndrome is a unique type of myelodysplastic syndrome characterized by a prolonged disease course, a low rate of transformation to an aggressive form of leukemia, and an anemia which in many patients is profound, refractory to traditional therapies (e.g. iron supplements, Erythropoietin), and requiring maintenance red blood cell transfusions. The disease is treated with a chemotherapy drug, lenalidomide.[5][20]
PDGFRB Translocations
[edit]Human chromosome translocations between the PDGFRB gene and at least any one of 30 genes on other chromosomes lead to myeloid and/or lymphoid neoplasms that are many ways similar to the neoplasm caused by the fusion of the PDGFRA (i.e. platelet derived growth factor receptor A or alpha-type-platelet derived growth factor receptor) gene with the FIP1L1 gene (see FIP1L1-PDGFRA fusion gene. The most common of these rare mutations is the translocation of PDGFRB gene with the ETV6 gene (also termed ETS variant gene 6).
PDGFRB-ETV6 translocations
[edit]The ETV6 gene codes for a transcription factor protein that in mice appears to be required for hematopoiesis and maintenance of the developing vascular network. The gene is located on human chromosome 12 at the p13 position, consists of 14 exons, and is well-known to be involved in a large number of chromosomal rearrangements associated with leukemia and congenital fibrosarcoma.[21] Translocations between it and the PDGFRB gene, notated as t(5;12)(q33;p13), yield a PDGFRB-ETV6 fused gene that encodes a fusion protein, PDGFRB-ETV6. This chimeric protein, unlike the PDGFRB protein: a) has continuously active PDGFRB-mediated tyrosine kinase due to its forced dimerization by the PNT protein binding domain of the ETV6 protein; b) is highly stable due to its resistance to ubiquitin-Proteasome degradation; and c) therefore over-stimulates cell signaling pathways such as STAT5, NF-κB, and Extracellular signal-regulated kinases which promote cell growth and proliferation. This continuous signaling, it is presumed, leads to the development of myeloid and/or lymphoid neoplasms that commonly include increased numbers of blood born and tissue eosinophils, eosinophil-induced organ and tissue injury, and possible progression to aggressive form of leukemia.[22]
PDGFRB-ETV6 fusion protein-induced neoplasms often present with features that would classify them as Chronic myelomonocytic leukemias, juvenile myelomonocytic leukemia, Atypical or Philadelphia chromosome negative chronic myeloid leukemias, myelodysplastic syndromes, acute myelogenous leukemias, or acute lymphoblastic leukemias. The disease is now classified by the World Health Organization as one form of clonal eosinophilia.[23] It is critical that the PDGFRB-ETV6 fusion protein-driven disease be diagnostically distinguished from many of the just cited other diseases because of its very different treatment.
Patients with the PDGFRB-ETV6 fusion protein-driven disease are more often adult males but rarely children. They present with anemia, increases in blood eosinophils and monocytes, splenomegaly, and, less often, lymphadenopathy. Bone marrow examination may reveal cellular features similar to that seen in the aforementioned diseases. Diagnosis is may by conventional cytogenetic examination of blood or bone marrow cells to test for PDGFRB rearrangements using Fluorescence in situ hybridization or to test for the fused FDGFRB-ATV6 fluorescence in situ hybridization and/or Real-time polymerase chain reaction using appropriate nucleotide probes.[22] These patients, unlike many patients with similarly appearing neoplasms, respond well to the tyrosine kinase inhibitor, imatinib. The drug often causes long-term complete hematological and cytogenic remissions as doses well below those used to treat chronic myelogenous leukemia. Primary or acquired drug resistance to this drug is very rare. Additional adjuvant chemotherapy may be necessary if a patient's disease is unresponsive to tyrosine kinase inhibitor therapy and/or progresses to more aggressive disease phase similar to that seen in the blast crisis of chronic myelogenous leukemia.[22][6]
Other PDGFRB translocations
[edit]The PDGFRB gene has been found to fuse with at least 36 other genes to form fusion genes that encode chimeric proteins that are known or presumed to possess: a) continuously active PDGFRB-derived tyrosine kinase activity; b) the ability to continuously stimulate the growth and proliferation of hematological stem cells; and c) the ability to cause myeloid and lymphoid neoplasms that commonly but not always are associated with eosinophilia. In all instances, these gene fusion diseases are considered types of clonal eosinophilia with recommended treatment regimens very different than those of similar hematological malignancies. The genes fusing to PDGFRB, their chromosomal location, and the notations describing their fused genes are given in the following table.[6][22]
| Gene | locus | notation | gene | locus | notation | Gene | locus | notation | gene | locus | notation | gene | locus | notation | gene | locus | notation | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TPM3 | 1q21 | t(1;5)(q21;q32) | PDE4DIP | 1q22 | t(1;5)(q22;q32) | SPTBN1 | 2p16 | t(2;5)(p16;q32) | GOLGA4 | 3p21-25 | t(3;5)(p21-25;q31-35) | WRD48[24] | 3p21-22 | t(1;3;5)(p36;p21;q32) | PRKG2[25] | 4q21 | t(4;5)(p21;q32) | |||||
| CEP85L[26] | 6q22 | t(5;6)(q32;q22) | HIP1 | 7q11 | t(5;7)(q32;q11) | KANK1 | 9q24 | t(5;9)(q32;q24) | BCR | 9q34 | t(5;9)(q32;q34) | CCDC6 | 10q21 | t(5;10)(q32;q21 | H4(D10S170)[27] | 10q21.2 | t(5;10)(q32;q21.2) | |||||
| GPIAP1[28] | 11p13 | multiple | ETV6 | 12p13 | t(5;12)q32;p13) | ERC1 | 12p13.3 | t(5;12)(q32;p13.3) | GIT2 | 12q24 | t(5;12)(q31-33;q24) | NIN[29] | 14q24 | t(5;14)(q32;q24 | TRIP11 | 14q32 | t(5;14)(q32;q32) | |||||
| CCDC88C[30] | 14q32 | t(5;14)(q33;q32) | TP53BP1 | 15q22 | t(5;15)q33;22) | NDE1 | 16p13 | t(5;16)(q33;p13) | SPECC1 | 17p11 | t(5;17)(q32;p11.2) | NDEL1 | 17p13 | t(5;17)(q32;p13) | MYO18A | 17q11.2 | t(5;17)(q32;q11.2) | |||||
| BIN2[31] | 12q13 | t(5;12)(q32;q13) | COL1A1 | 17q22 | t(5;17)q32;q22) | DTD1[32] | 20p11 | t(5;20)(q32;p11) | CPSF6 | 12q15 | t(5;12)(q32;q15) | RABEP1 | 17p13 | t(5;17)(q32;p13) | MPRIP | 17p11 | t(5;17)(q32;p11) | |||||
| SPTBN1 | 2p16 | t(5;2)(q32;p16) | WDR48[24] | 3p22 | t(5;3)q32;p22) | GOLGB1 | 3q12 | t(3;5)(q12;q32) | DIAPH1 | 5q31 | t(5;5)(q32;q31) | TNIP1 | 5q33 | t(5;5)(q32;q33) | SART3 | 12q23 | t(5;12)(q32;q23) |
Similar to PDGFRB-ETV6 translocations, these translocations are generally in-frame and encode for fusion proteins with their PDGFRB-derived tyrosine kinase being continuously active and responsible for causing the potentially malignant growth of its myeloid and/or lymphoid harboring cells. Patients are usually middle-aged men. They commonly present with anemia, eosinophilia, monocytosis, and splenomegaly and have their disease classified as chronic myelomonocytic leukemia, atypical chronic myelomonocytic leukemia, juvenile myelomonocytic leukemia, myelodysplastic syndrome, acute myelogenous leukemia, acute lymphoblastic leukemia, or T lymphoblastic lymphoma. Diagnosis relies on cytogenetic analyses to detect breakpoints in the long arm of chromosome 5 by Fluorescence in situ hybridization. These patients usually respond well to imatinib therapy.[6][22][33]
Primary familial brain calcification
[edit]Primary familial brain calcification (see Fahr's syndrome) is a rare disease involving bilateral calcifications in the brain, predominantly in basal ganglia but also cerebellum, thalamus, and brainstem in patients presenting with diverse neurologic (e.g. movement disorders, parkinsonism, seizures, headache) features and psychiatric (e.g. cognitive impairment, mood disorders, psychotic symptoms, and obsessive-compulsive) disturbances. In a minority of cases, the disease is associated with apparent autosomal dominant loss of function mutations in PDGFRB or the gene which encodes a ligand that simulates PDGFRB, Platelet-derived growth factor, PDGFB. PDGFRB is extensively expressed in the neurons, chorioid plexus, vascular smooth muscle cells, and pericytes of the human brain, particularly the basal ganglia and the dentate nucleus. It is proposed that signal transduction through PDGFRB maintains blood–brain barrier integrity and that loss of the PDGFRB receptor or its ligand, PDGFB, disrupts the blood–brain barrier, subsequently promoting (peri)vascular calcium deposition and thereby causing the dysfunction and death of neurons.[34][35]
Interactions
[edit]PDGFRB has been shown to interact with:
Notes
[edit]
The 2017 version of this article was updated by an external expert under a dual publication model. The corresponding academic peer reviewed article was published in Gene and can be cited as: Andrius Kazlauskas (3 March 2017). "PDGFs and their receptors". Gene. Gene Wiki Review Series. 614: 1–7. doi:10.1016/J.GENE.2017.03.003. ISSN 0378-1119. PMC 6728141. PMID 28267575. Wikidata Q39166181. |
See also
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000113721 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000024620 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b "PDGFRB platelet derived growth factor receptor beta [Homo sapiens (human)] - Gene - NCBI".
- ^ a b c d Reiter A, Gotlib J (2017). "Myeloid neoplasms with eosinophilia". Blood. 129 (6): 704–714. doi:10.1182/blood-2016-10-695973. PMID 28028030.
- ^ Heldin CH, Lennartsson J (August 2013). "Structural and functional properties of platelet-derived growth factor and stem cell factor receptors". Cold Spring Harbor Perspectives in Biology. 5 (8): a009100. doi:10.1101/cshperspect.a009100. PMC 3721287. PMID 23906712.
- ^ Kelly JD, Haldeman BA, Grant FJ, Murray MJ, Seifert RA, Bowen-Pope DF, et al. (May 1991). "Platelet-derived growth factor (PDGF) stimulates PDGF receptor subunit dimerization and intersubunit trans-phosphorylation". The Journal of Biological Chemistry. 266 (14): 8987–92. doi:10.1016/S0021-9258(18)31541-2. PMID 1709159.
- ^ Lei H, Kazlauskas A (2014). "A reactive oxygen species-mediated, self-perpetuating loop persistently activates platelet-derived growth factor receptor α". Molecular and Cellular Biology. 34 (1): 110–22. doi:10.1128/MCB.00839-13. PMC 3911282. PMID 24190966.
- ^ Lei H, Qian CX, Lei J, Haddock LJ, Mukai S, Kazlauskas A (2015). "RasGAP Promotes Autophagy and Thereby Suppresses Platelet-Derived Growth Factor Receptor-Mediated Signaling Events, Cellular Responses, and Pathology". Molecular and Cellular Biology. 35 (10): 1673–85. doi:10.1128/MCB.01248-14. PMC 4405646. PMID 25733681.
- ^ Soriano P (1994). "Abnormal kidney development and hematological disorders in PDGF beta-receptor mutant mice". Genes & Development. 8 (16): 1888–96. doi:10.1101/gad.8.16.1888. PMID 7958864.
- ^ Lindahl P, Johansson BR, Levéen P, Betsholtz C (1997). "Pericyte loss and microaneurysm formation in PDGF-B-deficient mice". Science. 277 (5323): 242–5. doi:10.1126/science.277.5323.242. PMID 9211853.
- ^ Lindahl P, Hellström M, Kalén M, Karlsson L, Pekny M, Pekna M, Soriano P, Betsholtz C (1998). "Paracrine PDGF-B/PDGF-Rbeta signaling controls mesangial cell development in kidney glomeruli". Development. 125 (17): 3313–22. doi:10.1242/dev.125.17.3313. PMID 9693135.
- ^ Levéen P, Pekny M, Gebre-Medhin S, Swolin B, Larsson E, Betsholtz C (1994). "Mice deficient for PDGF B show renal, cardiovascular, and hematological abnormalities". Genes & Development. 8 (16): 1875–87. doi:10.1101/gad.8.16.1875. PMID 7958863.
- ^ Darland DC, D'Amore PA (1999). "Blood vessel maturation: vascular development comes of age". The Journal of Clinical Investigation. 103 (2): 157–8. doi:10.1172/JCI6127. PMC 407889. PMID 9916126.
- ^ Olson LE, Soriano P (2011). "PDGFRβ signaling regulates mural cell plasticity and inhibits fat development". Developmental Cell. 20 (6): 815–26. doi:10.1016/j.devcel.2011.04.019. PMC 3121186. PMID 21664579.
- ^ Andrae J, Gallini R, Betsholtz C (2008). "Role of platelet-derived growth factors in physiology and medicine". Genes & Development. 22 (10): 1276–312. doi:10.1101/gad.1653708. PMC 2732412. PMID 18483217.
- ^ Heldin CH (2013). "Targeting the PDGF signaling pathway in tumor treatment". Cell Communication and Signaling. 11: 97. doi:10.1186/1478-811X-11-97. PMC 3878225. PMID 24359404.
- ^ Heldin CH (2014). "Targeting the PDGF signaling pathway in the treatment of non-malignant diseases". Journal of Neuroimmune Pharmacology. 9 (2): 69–79. doi:10.1007/s11481-013-9484-2. PMID 23793451. S2CID 17343813.
- ^ Nimer SD (2006). "Clinical management of myelodysplastic syndromes with interstitial deletion of chromosome 5q". Journal of Clinical Oncology. 24 (16): 2576–82. doi:10.1200/JCO.2005.03.6715. PMID 16735711.
- ^ "ETV6 ETS variant 6 [Homo sapiens (human)] - Gene - NCBI".
- ^ a b c d e Vega F, Medeiros LJ, Bueso-Ramos CE, Arboleda P, Miranda RN (2015). "Hematolymphoid neoplasms associated with rearrangements of PDGFRA, PDGFRB, and FGFR1". American Journal of Clinical Pathology. 144 (3): 377–92. doi:10.1309/AJCPMORR5Z2IKCEM. PMID 26276769.
- ^ Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW (2016). "The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia". Blood. 127 (20): 2391–405. doi:10.1182/blood-2016-03-643544. PMID 27069254.
- ^ a b "WDR48 WD repeat domain 48 [Homo sapiens (human)] - Gene - NCBI".
- ^ "PRKG2 protein kinase cGMP-dependent 2 [Homo sapiens (human)] - Gene - NCBI".
- ^ "CEP85L centrosomal protein 85 like [Homo sapiens (human)] - Gene - NCBI".
- ^ "CCDC6 coiled-coil domain containing 6 [Homo sapiens (human)] - Gene - NCBI".
- ^ "CAPRIN1 cell cycle associated protein 1 [Homo sapiens (human)] - Gene - NCBI".
- ^ "NIN ninein [Homo sapiens (human)] - Gene - NCBI".
- ^ "CCDC88C coiled-coil domain containing 88C [Homo sapiens (human)] - Gene - NCBI".
- ^ "BIN2 bridging integrator 2 [Homo sapiens (human)] - Gene - NCBI".
- ^ "DTD1 D-tyrosyl-tRNA deacylase 1 [Homo sapiens (human)] - Gene - NCBI".
- ^ Gotlib J (2015). "World Health Organization-defined eosinophilic disorders: 2015 update on diagnosis, risk stratification, and management". American Journal of Hematology. 90 (11): 1077–89. doi:10.1002/ajh.24196. PMID 26486351. S2CID 42668440.
- ^ Tadic V, Westenberger A, Domingo A, Alvarez-Fischer D, Klein C, Kasten M (2015). "Primary familial brain calcification with known gene mutations: a systematic review and challenges of phenotypic characterization". JAMA Neurology. 72 (4): 460–7. doi:10.1001/jamaneurol.2014.3889. PMID 25686319.
- ^ Batla A, Tai XY, Schottlaender L, Erro R, Balint B, Bhatia KP (2017). "Deconstructing Fahr's disease/syndrome of brain calcification in the era of new genes" (PDF). Parkinsonism & Related Disorders (Submitted manuscript). 37: 1–10. doi:10.1016/j.parkreldis.2016.12.024. PMID 28162874.
- ^ Matsumoto T, Yokote K, Take A, Takemoto M, Asaumi S, Hashimoto Y, Matsuda M, Saito Y, Mori S (April 2000). "Differential interaction of CrkII adaptor protein with platelet-derived growth factor alpha- and beta-receptors is determined by its internal tyrosine phosphorylation". Biochem. Biophys. Res. Commun. 270 (1): 28–33. doi:10.1006/bbrc.2000.2374. PMID 10733900.
- ^ Yamamoto M, Toya Y, Jensen RA, Ishikawa Y (March 1999). "Caveolin is an inhibitor of platelet-derived growth factor receptor signaling". Exp. Cell Res. 247 (2): 380–8. doi:10.1006/excr.1998.4379. PMID 10066366.
- ^ a b c Braverman LE, Quilliam LA (February 1999). "Identification of Grb4/Nckbeta, a src homology 2 and 3 domain-containing adapter protein having similar binding and biological properties to Nck". J. Biol. Chem. 274 (9): 5542–9. doi:10.1074/jbc.274.9.5542. PMID 10026169.
- ^ Arvidsson AK, Rupp E, Nånberg E, Downward J, Rönnstrand L, Wennström S, Schlessinger J, Heldin CH, Claesson-Welsh L (October 1994). "Tyr-716 in the platelet-derived growth factor beta-receptor kinase insert is involved in GRB2 binding and Ras activation". Mol. Cell. Biol. 14 (10): 6715–26. doi:10.1128/mcb.14.10.6715. PMC 359202. PMID 7935391.
- ^ Tang J, Feng GS, Li W (October 1997). "Induced direct binding of the adapter protein Nck to the GTPase-activating protein-associated protein p62 by epidermal growth factor". Oncogene. 15 (15): 1823–32. doi:10.1038/sj.onc.1201351. PMID 9362449.
- ^ Li W, Hu P, Skolnik EY, Ullrich A, Schlessinger J (December 1992). "The SH2 and SH3 domain-containing Nck protein is oncogenic and a common target for phosphorylation by different surface receptors". Mol. Cell. Biol. 12 (12): 5824–33. doi:10.1128/MCB.12.12.5824. PMC 360522. PMID 1333047.
- ^ Chen M, She H, Davis EM, Spicer CM, Kim L, Ren R, Le Beau MM, Li W (September 1998). "Identification of Nck family genes, chromosomal localization, expression, and signaling specificity". J. Biol. Chem. 273 (39): 25171–8. doi:10.1074/jbc.273.39.25171. PMID 9737977.
- ^ Chen M, She H, Kim A, Woodley DT, Li W (November 2000). "Nckbeta adapter regulates actin polymerization in NIH 3T3 fibroblasts in response to platelet-derived growth factor bb". Mol. Cell. Biol. 20 (21): 7867–80. doi:10.1128/mcb.20.21.7867-7880.2000. PMC 86398. PMID 11027258.
- ^ Rupp E, Siegbahn A, Rönnstrand L, Wernstedt C, Claesson-Welsh L, Heldin CH (October 1994). "A unique autophosphorylation site in the platelet-derived growth factor alpha receptor from a heterodimeric receptor complex". Eur. J. Biochem. 225 (1): 29–41. doi:10.1111/j.1432-1033.1994.00029.x. PMID 7523122.
- ^ Seifert RA, Hart CE, Phillips PE, Forstrom JW, Ross R, Murray MJ, Bowen-Pope DF (May 1989). "Two different subunits associate to create isoform-specific platelet-derived growth factor receptors". J. Biol. Chem. 264 (15): 8771–8. doi:10.1016/S0021-9258(18)81860-9. PMID 2542288.
- ^ Keilhack H, Müller M, Böhmer SA, Frank C, Weidner KM, Birchmeier W, Ligensa T, Berndt A, Kosmehl H, Günther B, Müller T, Birchmeier C, Böhmer FD (January 2001). "Negative regulation of Ros receptor tyrosine kinase signaling. An epithelial function of the SH2 domain protein tyrosine phosphatase SHP-1". J. Cell Biol. 152 (2): 325–34. doi:10.1083/jcb.152.2.325. PMC 2199605. PMID 11266449.
- ^ Lechleider RJ, Sugimoto S, Bennett AM, Kashishian AS, Cooper JA, Shoelson SE, Walsh CT, Neel BG (October 1993). "Activation of the SH2-containing phosphotyrosine phosphatase SH-PTP2 by its binding site, phosphotyrosine 1009, on the human platelet-derived growth factor receptor". J. Biol. Chem. 268 (29): 21478–81. doi:10.1016/S0021-9258(20)80562-6. PMID 7691811.
- ^ Farooqui T, Kelley T, Coggeshall KM, Rampersaud AA, Yates AJ (1999). "GM1 inhibits early signaling events mediated by PDGF receptor in cultured human glioma cells". Anticancer Res. 19 (6B): 5007–13. PMID 10697503.
- ^ Ekman S, Kallin A, Engström U, Heldin CH, Rönnstrand L (March 2002). "SHP-2 is involved in heterodimer specific loss of phosphorylation of Tyr771 in the PDGF beta-receptor". Oncogene. 21 (12): 1870–5. doi:10.1038/sj.onc.1205210. PMID 11896619.
- ^ Yokote K, Mori S, Hansen K, McGlade J, Pawson T, Heldin CH, Claesson-Welsh L (May 1994). "Direct interaction between Shc and the platelet-derived growth factor beta-receptor". J. Biol. Chem. 269 (21): 15337–43. doi:10.1016/S0021-9258(17)36611-5. PMID 8195171.
- ^ Maudsley S, Zamah AM, Rahman N, Blitzer JT, Luttrell LM, Lefkowitz RJ, Hall RA (November 2000). "Platelet-derived growth factor receptor association with Na(+)/H(+) exchanger regulatory factor potentiates receptor activity". Mol. Cell. Biol. 20 (22): 8352–63. doi:10.1128/mcb.20.22.8352-8363.2000. PMC 102142. PMID 11046132.
Further reading
[edit]- Hart CE, Bowen-Pope DF (1990). "Platelet-derived growth factor receptor: current views of the two-subunit model". J. Invest. Dermatol. 94 (6 Suppl): 53S – 57S. doi:10.1111/1523-1747.ep12875065. PMID 2161888.
- Steer EJ, Cross NC (2002). "Myeloproliferative disorders with translocations of chromosome 5q31-35: role of the platelet-derived growth factor receptor Beta". Acta Haematol. 107 (2): 113–22. doi:10.1159/000046641. PMID 11919393. S2CID 202646911.
External links
[edit]- CD140B+Antigen at the U.S. National Library of Medicine Medical Subject Headings (MeSH)