User:Nikopants/sandbox
 | This is a user sandbox of Nikopants. You can use it for testing or practicing edits. This is not the sandbox where you should draft your assigned article for a dashboard.wikiedu.org course. To find the right sandbox for your assignment, visit your Dashboard course page and follow the Sandbox Draft link for your assigned article in the My Articles section. |
| Nikopants/sandbox | |
|---|---|
 |
Blunt trauma, blunt injury, non-penetrating trauma or blunt force trauma is physical trauma to a body part, either by impact, injury or physical attack. The latter is usually referred to as blunt force trauma. Blunt trauma is the initial trauma, from which develops more specific types such as contusions, abrasions, lacerations, and/or bone fractures. Blunt trauma is contrasted with penetrating trauma, in which an object such as a projectile or knife enters the body.
Classification
[edit]Blunt abdominal trauma
[edit]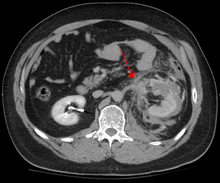
Blunt abdominal trauma (BAT) comprises 75% of all blunt trauma and is the most common example of this injury.[1] The majority occurs in motor vehicle accidents, in which rapid deceleration may propel the driver into the steering wheel, dashboard, or seatbelt[2] causing contusions in less serious cases, or rupture of internal organs from briefly increased intraluminal pressure in the more serious, depending on the force applied. It is important to note that initially there may be little in the way of overt clinical signs to indicate that serious internal abdominal injury has occurred, making assessment more challenging and requiring a high degree of clinical suspicion.[3]
There are two basic physical mechanisms at play with the potential of injury to intra-abdominal organs: compression and deceleration.[4] The former occurs from a direct blow, such as a punch, or compression against a non-yielding object such as a seat belt or steering column. This force may deform a hollow organ thereby increasing its intra-luminal or internal pressure, leading to rupture. Deceleration, on the other hand, causes stretching and shearing at the points at which mobile structures, such as the bowel, are anchored. This can cause tearing of the mesentery of the bowel, and injury to the blood vessels that travel within the mesentery. Classic examples of these mechanisms are a hepatic tear along the ligamentum teres and injuries to the renal arteries.
When blunt abdominal trauma is complicated by 'internal injury', the liver and spleen (see blunt splenic trauma) are most frequently involved, followed by the small intestine.
In rare cases, this injury has been attributed to medical techniques such as the Heimlich Maneuver,[5] attempts at cardiopulmonary resuscitation and manual thrusts to clear an airway. Although these are rare examples, it has been suggested that they are caused by applying excessive pressure when administering such techniques. Finally, the occurrence of splenic rupture with mild blunt abdominal trauma in those convalescing from infectious mononucleosis is well reported.[6]
Blunt thoracic trauma
[edit]The term blunt thoracic trauma or put simply, blunt chest injury, encompasses a variety of injuries to the chest. Broadly, this also includes damage caused by direct blunt force (such as a fist or a bat in an assault), acceleration or deceleration (such as that from a rear-end automotive accident), shear force, compression (such as a heavy object falling on a person), and blasts (such as an explosion of some sort). Common signs and symptoms include: bruising, hypoxia, ventilation-perfusion mismatch, hypovolemia, and reduced cardiac output. Blunt thoracic trauma is not always visible from the outside and such internal injuries may not show signs or symptoms at the time the trauma initially occurs or even until hours after. A high degree of clinical suspicion may sometimes be required to identify such injuries, computed tomography may prove useful in such instances. Those experiencing more obvious injuries from a blunt chest injury will likely undergo a focused assessment with sonography for trauma (FAST) which can reliably detect a significant amount of blood around the heart or in the lung. Only 10-15% of thoracic traumas require surgery, but they can have serious impacts on the heart, lungs, and great vessels. [7]
The most immediate life-threatening injuries that may occur include tension pneumothorax, open pneumothorax, hemothorax, flail chest, cardiac tamponade, airway obstruction/rupture. [8]
The injuries may necessitate a procedure, with the most common being the insertion of an intercostal drain, more commonly referred to as a chest tube. This tube is typically placed because it helps restore a certain balance in pressures (usually due to misplaced air or surrounding blood) that are impeding the lungs ability to inflate and thus exchange vital gases that allow the body to function.[9] A less common procedure that may be employed is a pericardiocentesis which by removing blood surrounding the heart, permits the heart to regain some ability to appropriately pump blood.[10] In certain dire circumstances an emergent thoracotomy may be employed.[11]
Blunt cranial trauma
[edit]See also: Traumatic Brain Injury
The primary clinical concern when blunt trauma to the head occurs is damage to the brain, although other structures, including the skull, face, orbits, and neck are also at risk.
Traumatic Brain Injury
[edit]Traumatic brain injury is a significant cause of morbidity and mortality and is most commonly caused by falls, motor vehicle accidents, sports- and work-related injuries, and assaults.
Other Blunt Cranial Injuries
[edit]Blunt trauma to extremities
[edit]Injury to extremities is extremely common.[12] Falls are the most common etiology, comprising as much as 30% of upper & 60% of lower extremity injuries. The most common mechanism for solely upper extremity injuries is machine operation or tool use. Work related accidents and vehicle crashes are also common causes. [13] The injured extremity is examined for four major functional components which include soft tissues, nerves, vessels, and bones.[14] Vessels are examined for expanding hematoma, bruit, distal pulse exam, and signs/symptoms of ischemia.[15] In the absence of such obvious indications of vascular compromise, an injured extremity index or ankle-brachial index may be used to help guide whether further evaluation with computed tomography arteriography. [16] Soft tissue damage can lead to rhabdomyolysis or may potentially develop compartment syndrome. [17][18] Bones are evaluated with plain film x-ray or computed tomography if deformity, bruising, or joint laxity are observed. Neurologic evaluation involves testing of the major nerve functions of the axillary, radial, and median nerves in the upper extremity as well as the femoral, sciatic, deep peroneal, and tibial nerves in the lower extremity. Surgical treatment may be indicated depending on the extent of injury and involved structures, but many are managed nonoperatively. [19]
Blunt pelvic trauma
Diagnosis
[edit]In all but the most obviously trivial injuries, the first concern is to exclude anything that might be quickly or immediately life-threatening. This is resolved by ascertaining that the subject's airway is open and competent, that breathing is unlabored, and that circulation—i.e. pulses that can be felt—is present. This is sometimes described as the "A, B, C's"—Airway, Breathing, and Circulation—and is the first step in any resuscitation or triage. Then, the history of the accident or injury is amplified with any medical, dietary (timing of last oral intake) and past history, from whatever sources such as family, friends, previous treating physicians that might be available. This method is sometimes given the mnemonic "SAMPLE". The amount of time spent on diagnosis should be minimized and expedited by a combination of clinical assessment and appropriate use of technology,[20] such as diagnostic peritoneal lavage (DPL), or bedside ultrasound examination (FAST)[21] before proceeding to laparotomy if required. If time and the patient's stability permits, CT examination may be carried out if available.[22] Its advantages include superior definition of the injury, leading to grading of the injury and sometimes the confidence to avoid or postpone surgery. Its disadvantages include the time taken to acquire images, although this gets shorter with each generation of scanners, and the removal of the patient from the immediate view of the emergency or surgical staff.
Recently, criteria have been defined that might allow patients with blunt abdominal trauma to be discharged safely without further evaluation. The characteristics of such patients would include:
- absence of intoxication
- no evidence of lowered blood pressure or raised pulse rate
- no abdominal pain or tenderness
- no blood in the urine.
To be considered low risk, patients would need to meet all low-risk criteria.[23]
Blunt abdominal trauma in sports
[edit]In the US, the majority of contact-collision injuries, usually blunt trauma, should have been witnessed in high school or collegiate games where the athletic training staff are trained to keep their eyes on the play. This may allow some departure from Advanced Trauma Life Support guidelines in the initial assessment, although the principles always apply. The major priority then becomes separating contusions and musculo-tendinous injuries from injuries to solid organs and the gut and recognizing potential for developing blood loss, and reacting accordingly. Blunt injuries to the kidney from helmets, shoulder pads, and knees are also described in American football,[24] association football, martial arts, and all-terrain vehicle accidents.
Treatment
[edit]In every case where the presumption of internal injury has been sufficient to trigger the diagnostic steps outlined above, intravenous access will be established and crystalloid solutions and/or blood will be administered at rates sufficient to maintain the circulation. Thereafter, further treatment will depend on the grade of organ damage estimated by the prior investigations and will vary from close observation with the ability to intervene quickly, or surgery, open or laparoscopic.[25] In the case of blunt abdominal trauma, there is no shown benefit from surgery unless bleeding is present.[26]
Outcomes
[edit]Epidemiology
[edit]Special populations
[edit]See also
[edit]References
[edit]- ^ Isenhour JL, Marx J (August 2007). "Advances in abdominal trauma". Emerg Med Clin North Am. 25 (3): 713–33, ix. doi:10.1016/j.emc.2007.06.002. PMID 17826214.
- ^ Bansal V, Conroy C, Tominaga GT, Coimbra R (December 2009). "The utility of seat belt signs to predict intra-abdominal injury following motor vehicle crashes". Traffic Inj Prev. 10 (6): 567–72. doi:10.1080/15389580903191450. PMID 19916127.
- ^ Fitzgerald, J.E.F.; Larvin, Mike (2009). "Chapter 15: Management of Abdominal Trauma". In Baker, Qassim; Aldoori, Munther (eds.). Clinical Surgery: A Practical Guide. CRC Press. pp. 192–204. ISBN 9781444109627.
- ^ Mukhopadhyay M (October 2009). "Intestinal Injury from Blunt Abdominal Trauma: A Study of 47 Cases". Oman Med J. 24 (4): 256–259. doi:10.5001/omj.2009.52. PMC 3243872. PMID 22216378.
- ^ Mack L, Forbes TL, Harris KA (January 2002). "Acute aortic thrombosis following incorrect application of the Heimlich maneuver". Ann Vasc Surg. 16 (1): 130–3. doi:10.1007/s10016-001-0147-z. PMID 11904818.
- ^ O'Connor TE, Skinner LJ, Kiely P, Fenton JE (August 2011). "Return to contact sports following infectious mononucleosis: the role of serial ultrasonography". Ear Nose Throat J. 90 (8): E21–4. PMID 21853428.
- ^ Blyth, Andrew (2014-03-07). "Thoracic Trauma". BMJ. 348: bmj.g1137. doi:10.1136/bmj.g1137. ISSN 0959-8138. PMID 24609501.
- ^ Blyth, Andrew (2014-03-07). "Thoracic Trauma". BMJ. 348: bmj.g1137. doi:10.1136/bmj.g1137. ISSN 1756-1833. PMID 24609501.
- ^ Falter, Florian; Nair, Sukumaran (2012), "Intercostal Chest Drain Insertion", Bedside Procedures in the ICU, Springer, London, pp. 105–111, doi:10.1007/978-1-4471-2259-3_10, ISBN 9781447122586, retrieved 2018-12-13
- ^ Maisch, Bernhard; Ristić, Arsen D.; Seferović, Petar M.; Tsang, Teresa S. M. (2011). "Interventional Pericardiology". doi:10.1007/978-3-642-11335-2.
{{cite journal}}: Cite journal requires|journal=(help) - ^ "Thoracic Trauma: Injuries, Evaluation, and Treatment". Surgical Clinics of North America. 97 (4): 783–799. 2017-08-01. doi:10.1016/j.suc.2017.03.004. ISSN 0039-6109.
- ^ de Mestral, Charles; Sharma, Sunjay; Haas, Barbara; Gomez, David; Nathens, Avery B. (2013-2). "A contemporary analysis of the management of the mangled lower extremity". The Journal of Trauma and Acute Care Surgery. 74 (2): 597–603. doi:10.1097/TA.0b013e31827a05e3. ISSN 2163-0763. PMID 23354257.
{{cite journal}}: Check date values in:|date=(help) - ^ Søreide, K. (2009). "Epidemiology of major trauma". BJS. 96 (7): 697–698. doi:10.1002/bjs.6643. ISSN 1365-2168.
- ^ Johansen, Kaj; Helfet, D. L.; Howey, T.; Dairies, M.; Sanders, R.; Hansen, S. T. (1989-06-01). "Objective Criteria Accurately Predict Amputation Following Lower Extremity Trauma". Journal of Orthopaedic Trauma. 3 (2). doi:10.1097/00005131-198906000-00030. ISSN 0890-5339.
- ^ www.facs.org https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/ntdb%20annual%20report%202012.ashx. Retrieved 2018-12-16.
{{cite web}}: Missing or empty|title=(help) - ^ Lynch, K.; Johansen, K. (1991-12). "Can Doppler pressure measurement replace "exclusion" arteriography in the diagnosis of occult extremity arterial trauma?". Annals of Surgery. 214 (6): 737–741. ISSN 0003-4932. PMC 1358501. PMID 1741655.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - ^ Egan, Aileen F.; Cahill, Kevin C. (2017-11-09). "Compartment Syndrome". New England Journal of Medicine. 377 (19): 1877–1877. doi:10.1056/NEJMicm1701729. ISSN 0028-4793. PMID 29117495.
- ^ Bosch, Xavier; Poch, Esteban; Grau, Josep M. (2009-07-02). "Rhabdomyolysis and Acute Kidney Injury". New England Journal of Medicine. 361 (1): 62–72. doi:10.1056/NEJMra0801327. ISSN 0028-4793. PMID 19571284.
- ^ KENNEDY, ROBERT H. (1932-09-01). "Emergency Treatment of Extremity Fractures". New England Journal of Medicine. 207 (9): 393–395. doi:10.1056/NEJM193209012070903. ISSN 0028-4793.
- ^ Woods SD (February 1995). "Assessment of blunt abdominal trauma". Aust N Z J Surg. 65 (2): 75–6. doi:10.1111/j.1445-2197.1995.tb07263.x. PMID 7857232.
- ^ Marco GG, Diego S, Giulio A, Luca S (October 2005). "Screening US and CT for blunt abdominal trauma: a retrospective study". Eur J Radiol. 56 (1): 97–101. doi:10.1016/j.ejrad.2005.02.001. PMID 16168270.
- ^ Jansen JO, Yule SR, Loudon MA (April 2008). "Investigation of blunt abdominal trauma". BMJ. 336 (7650): 938–42. doi:10.1136/bmj.39534.686192.80. PMC 2335258. PMID 18436949.
- ^ Kendall JL, Kestler AM, Whitaker KT, Adkisson MM, Haukoos JS (November 2011). "Blunt abdominal trauma patients are at very low risk for intra-abdominal injury after emergency department observation". West J Emerg Med. 12 (4): 496–504. doi:10.5811/westjem.2010.11.2016. PMC 3236146. PMID 22224146.
- ^ Brophy RH, Gamradt SC, Barnes RP, et al. (January 2008). "Kidney injuries in professional American football: implications for management of an athlete with 1 functioning kidney". Am J Sports Med. 36 (1): 85–90. doi:10.1177/0363546507308940. PMID 17986635.
- ^ D'Errico E, Goffre B, Mazza D (2009). "Blunt abdominal trauma: current management". Chir Ital. 61 (5–6): 601–6. PMID 20380265.
- ^ Oyo-Ita, Angela; Chinnock, Paul; Ikpeme, Ikpeme A. (2015-11-13). "Surgical versus non-surgical management of abdominal injury". The Cochrane Database of Systematic Reviews (11): CD007383. doi:10.1002/14651858.CD007383.pub3. ISSN 1469-493X. PMID 26568111.
Category:Injuries Category:Medical emergencies Category:Causes of death Category:Trauma types
