Ritonavir
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /rɪˈtɒnəˌvɪər/ rih-TO-nə-veer |
| Trade names | Norvir |
| Other names | RTV |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a696029 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 98–99% |
| Metabolism | Liver, CYP3A4 |
| Elimination half-life | 3–4 hours[6][7] |
| Excretion | Mostly fecal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.125.710 |
| Chemical and physical data | |
| Formula | C37H48N6O5S2 |
| Molar mass | 720.95 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Ritonavir, sold under the brand name Norvir, is an antiretroviral medication used along with other medications to treat HIV/AIDS.[4][5][8] This combination treatment is known as highly active antiretroviral therapy (HAART).[8] Ritonavir is a protease inhibitor, though it now mainly serves to boost the potency of other protease inhibitors.[8][9] It may also be used in combination with other medications to treat hepatitis C and COVID-19.[10][11] It is taken by mouth.[8]
Common side effects of ritonavir include nausea, vomiting, loss of appetite, diarrhea, and numbness of the hands and feet.[8] Serious side effects include liver complications, pancreatitis, allergic reactions, and arrhythmias.[8] Serious interactions may occur with a number of other medications including amiodarone and simvastatin.[8] At low doses, it is considered to be acceptable for use during pregnancy.[12] Ritonavir is of the protease inhibitor class.[8] However, it is also commonly used to inhibit the enzyme that metabolizes other protease inhibitors.[13] This inhibition allows lower doses of these latter medications to be used.[13]
Ritonavir was patented in 1989 and came into medical use in 1996.[14][15] It is on the World Health Organization's List of Essential Medicines.[16][17] Ritonavir capsules were approved as a generic medication in the United States in 2020.[18]
Medical uses
[edit]This section needs expansion with: a lead sentence that better describes the very important (pharmacokinetic-pharmakodynamic) PK-PD observations for this first-in-class inhibitor design, and its initial application. You can help by adding to it. (February 2020) |
HIV
[edit]Ritonavir is indicated in combination with other antiretroviral agents for the treatment of HIV-1-infected patients.[4][5][8] Though initially developed as an independent antiviral treatment, it is most commonly used as a pharmacokinetic enhancer, in order to increase the plasma concentrations of other antiretrovirals.[19][20] Ritonavir is effective in preventing the replication of HIV-1. Protease inhibitors, including ritonavir, effectively block HIV-1 protease, a crucial enzyme in the reproductive cycle of HIV-1.[21]
COVID-19
[edit]Two SARS-CoV-2 3CLpro inhibitors are prepackaged with ritonavir to enhance their blood concentration.[22]
In December 2021, the combination of nirmatrelvir and ritonavir was granted emergency use authorization by the US Food and Drug Administration (FDA) for the treatment of coronavirus disease COVID-19.[23][24][25] The co-packaged medications are sold under the brand name Paxlovid.[24][25][26] Paxlovid is not authorized for the pre-exposure or post-exposure prevention of COVID-19 or for initiation of treatment in those requiring hospitalization due to severe or critical COVID-19.[24] On December 31, 2021, the UK Medicines and Healthcare products Regulatory Agency (MHRA) approved the same combination "for people with mild to moderate COVID-19 who are at high risk of developing severe COVID-19".[27][28]
In January 2023, simnotrelvir/ritonavir was conditionally approved by China's National Medical Products Administration (NMPA) for COVID-19.[22]
Other uses
[edit]The use of ritonavir as a CYP3A inhibitor is also seen in the Hepatitis C medication ombitasvir/paritaprevir/ritonavir.[9]
Side effects
[edit]When administered at the initially tested higher doses effective for anti-HIV therapy, the side effects of ritonavir are those shown below.[4]
- Asthenia, malaise
- Diarrhea
- Nausea and vomiting
- Abdominal pain
- Dizziness
- Insomnia
- Kidney failure
- Sweating
- Taste abnormality
- Metabolic effects, including
- Hypercholesterolemia
- Hypertriglyceridemia
- Elevated transaminases
- Elevated creatine kinase
Adverse drug reactions
[edit]Ritonavir exhibits hepatic activity.[29] It induces CYP1A2 and inhibits CYP3A4 and CYP2D6. Concomitant therapy of ritonavir with a variety of medications may result in serious and sometimes fatal drug interactions.[30]
Due to it being a strong inhibitor (that causes at least a five-fold increase in the plasma AUC values, or more than 80% decrease in clearance) of both cytochrome P450 enzymes CYP2D6 and CYP3A4, ritonavir can severely potentiate and prolong the half-life and/or increase the blood concentration of phenobarbital, primidone, carbamazepine, phenytoin, PDE5 inhibitors like sildenafil, opioids such as hydrocodone, oxycodone, pethidine and fentanyl, antiarrhythmic agents such as amiodarone, propafenone and disopyramide, immunosuppressants such as tacrolimus, voclosporin and sirolimus, neuroleptics like lurasidone and pimozide, as well as some chemotherapeutic agents, benzodiazepines and some ergot derivatives.[31][32] The FDA has issued a boxed warning for this type of drug interactions.[9]
CYP3A4 inducers can counteract the inhibiting effects of ritonavir and lead to drastically reduced levels of "boosted" drugs, increasing the risk of developing drug resistance. Other CYP3A4 inhibitors may have an additive effect with ritonavir, causing increased drug levels.[9]
Pharmacology
[edit]This section needs expansion with: with an accurate description of both its HIV protease and CYP3A4 binding characteristics and structural details. You can help by adding to it. (February 2020) |

Pharmacodynamics
[edit]Ritonavir was originally developed as an inhibitor of HIV protease,[33] one of a family of pseudo-C2-symmetric small molecule inhibitors.[34]
Ritonavir is rarely used for its own antiviral activity but remains widely used as a booster of other protease inhibitors. More specifically, ritonavir is used to inhibit a particular enzyme, in intestines, liver, and elsewhere, that normally metabolizes protease inhibitors, cytochrome P450-3A4 (CYP3A4). The drug binds to and inhibits CYP3A4, so a low dose can be used to enhance other protease inhibitors. This discovery drastically reduced the adverse effects and improved the efficacy of protease inhibitors and HAART.[35][36]. However, because of the general role of CYP3A4 in xenobiotic metabolism, dosing with ritonavir also affects the efficacy of numerous other medications, adding to the challenge of prescribing drugs concurrently. See § Adverse drug reactions above.[9][37]
Pharmacokinetics
[edit]Ritonavir at a 200 mg dose reaches maximum plasma concentration in about 3 hours and has a half life of 3–4 hours.[6][7] Importantly, the pharmacokinetics of Ritonavir are not linear—the half life increases at higher doses or under repeated dosing.[6] For instance, the half life of a 500 mg tablet is 4–6 hours rather than 3–4 hours for a 200 mg tablet.[6] The drug has high bioavailability but about 20% is lost due to first-pass metabolism.[6] Rivonavir capsules are not absorbed as quickly as Ritonavir tablets and may exhibit different bioavailability.[8]
Ritonavir was demonstrated to have an in vitro potency of EC50=0.02 μM on HIV-1 protease and highly sustained concentration in plasma after oral administration in several species.[38]
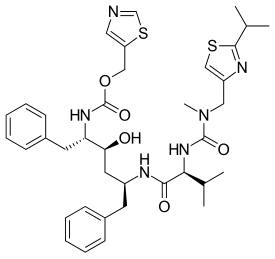
Chemistry
[edit]Ritonavir was initially derived from a moderately potent and orally bioavailable small molecule, A-80987. The P3 and P2′ heterocyclic groups of A-80987 were redesigned to create an analogue, now known as ritonavir, with improved pharmacokinetic properties to the original.[38]
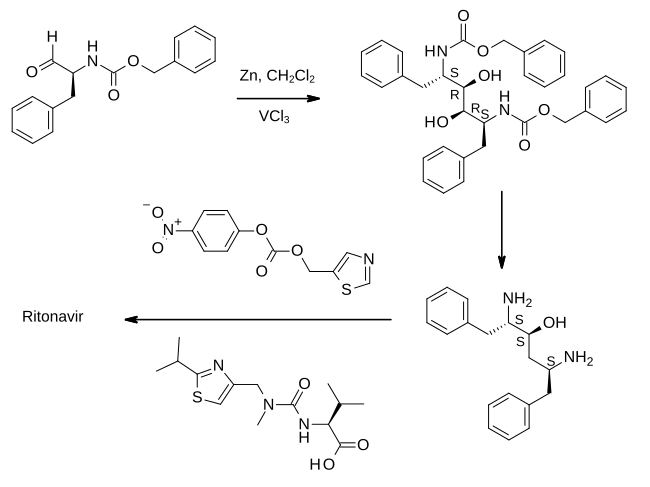
Full details of the synthesis of ritonavir were first published by scientists from Abbott Laboratories.
In the first step shown, an aldehyde derived from phenylalanine is treated with zinc dust in the presence of vanadium(III) chloride. This results in a pinacol coupling reaction which dimerizes the material to provide an intermediate which is converted to its epoxide and then reduced to (2S,3S,5S)-2,5-diamino-1,6-diphenylhexan-3-ol. Importantly, this retains the absolute stereochemistry of the amino acid precursor. The diamine is then treated sequentially with two thiazole derivatives, each linked by an amide bond, to provide ritonavir.[33][39]
History
[edit]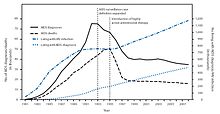
Ritonavir is sold as Norvir by AbbVie, Inc.[4][5] The US Food and Drug Administration (FDA) approved ritonavir on March 1, 1996,[41][42] As a result of the introduction of "highly active antiretroviral thearap[ies]" the annual U.S. HIV-associated death rate fell from over 50,000 to about 18,000 over a period of two years.[40]
In 2014, the FDA approved a combination of ombitasvir/paritaprevir/ritonavir for the treatment of hepatitis C virus (HCV) genotype 4.[10]
After the start of the COVID pandemic in 2020, many antivirals, including protease inhibitors in general and ritonavir in particular, were repurposed in an effort to treat the new infection. Lopinavir/ritonavir was found not to work in severe COVID-19.[43] Virtual screening followed by molecular dynamics analysis predicted ritonavir blocks the binding of the SARS-CoV-2 spike (S) protein to the human angiotensin-converting enzyme 2 (hACE2) receptor, which is critical for the virus entry into human cells.[44]
Finally in 2021, a combination of ritonavir with nirmatrelvir, a newly developed orally active 3C-like protease inhibitor, was developed for the treatment of COVID-19.[45][46][47][48] Ritonavir serves to slow down metabolism of nirmatrelvir by cytochrome enzymes to maintain higher circulating concentrations of the main drug.[49] In November that year, Pfizer announced positive phase 2/3 results, including 89% reduction in hospitalizations when given within three days after symptom onset.[50][51]
Polymorphism and temporary market withdrawal
[edit]Ritonavir was originally dispensed as a capsule that did not require refrigeration. This contained a crystal form of ritonavir that is now called form I.[52] However, like many drugs, crystalline ritonavir can exhibit polymorphism, i.e., the same molecule can crystallize into more than one crystal type, or polymorph, each of which contains the same repeating molecule but in different crystal packings/arrangements. The solubility and hence the bioavailability can vary in the different arrangements, and this was observed for forms I and II of ritonavir.[53]
During development—ritonavir was introduced in 1996—only the crystal form now called form I was found; however, in 1998, a lower free energy,[54] more stable polymorph, form II, was discovered. This more stable crystal form was less soluble, which resulted in significantly lower bioavailability. The compromised oral bioavailability of the drug led to temporary removal of the oral capsule formulation from the market.[53] As a consequence of the fact that even a trace amount of form II can result in the conversion of the more bioavailable form I into form II, the presence of form II threatened the ruin of existing supplies of the oral capsule formulation of ritonavir; and indeed, form II was found in production lines, effectively halting ritonavir production.[52] Abbott (now AbbVie) withdrew the capsules from the market, and prescribing physicians were encouraged to switch to a Norvir suspension.[citation needed] It has been estimated that Abbott lost more than US$250 million as a result, and the incident is often cited as a high-profile example of disappearing polymorphs.[55]
The company's research and development teams ultimately solved the problem by replacing the capsule formulation with a refrigerated gelcap.[when?][citation needed] In 2000, Abbott (now AbbVie) received FDA-approval for a tablet formulation of lopinavir/ritonavir (Kaletra) which contained a preparation of ritonavir that did not require refrigeration.[56] Ritonavir tablets produced in a solid dispersion by melt-extrusion was found to remain in form I, and was re-introduced commercially in 2010.[57]
Society and culture
[edit]Economics
[edit]In 2003, Abbott (AbbVie, Inc.) raised the price of a Norvir course from US$1.71 per day to US$8.57 per day, leading to claims of price gouging by patients' groups and some members of Congress. Consumer group Essential Inventions petitioned the NIH to override the Norvir patent, but the NIH announced on August 4, 2004, that it lacked the legal right to allow generic production of Norvir.[58]
References
[edit]- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved October 22, 2023.
- ^ "Notice: Nirmatrelvir (COVID-19) added to Prescription Drug List (PDL)". Health Canada. January 17, 2022. Archived from the original on May 29, 2022. Retrieved June 25, 2022.
- ^ "Norvir Product information". Health Canada. April 25, 2012. Retrieved June 25, 2022.
- ^ a b c d e "Norvir- ritonavir tablet, film coated Norvir- ritonavir solution Norvir- ritonavir powder". DailyMed. Archived from the original on November 18, 2021. Retrieved November 17, 2021.
- ^ a b c d "Norvir EPAR". European Medicines Agency (EMA). September 17, 2018. Archived from the original on October 2, 2018. Retrieved August 20, 2020. Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^ a b c d e Hsu A, Granneman GR, Witt G, Locke C, Denissen J, Molla A, et al. (May 1997). "Multiple-dose pharmacokinetics of ritonavir in human immunodeficiency virus-infected subjects". Antimicrobial Agents and Chemotherapy. 41 (5): 898–905. doi:10.1128/aac.41.5.898. PMC 163822. PMID 9145841.
- ^ a b Danner SA, Carr A, Leonard JM, Lehman LM, Gudiol F, Gonzales J, Raventos A, Rubio R, Bouza E, Pintado V, Aguado AG, Garcia de Lomas J, Delgado R, Borleffs JC, Hsu A, Valdes JM, Boucher CA, Cooper DA (December 1995). "A short-term study of the safety, pharmacokinetics, and efficacy of ritonavir, an inhibitor of HIV-1 protease. European-Australian Collaborative Ritonavir Study Group". The New England Journal of Medicine. 333 (23): 1528–1533. doi:10.1056/NEJM199512073332303. hdl:2445/121979. PMID 7477167.
- ^ a b c d e f g h i j "Ritonavir". The American Society of Health-System Pharmacists. Archived from the original on October 17, 2015. Retrieved October 23, 2015.
- ^ a b c d e Talha B, Dhamoon AS (August 8, 2023). "Ritonavir". StatPearls. StatPearls Publishing. PMID 31335032. Retrieved January 6, 2024.
- ^ a b "FDA approves Viekira Pak to treat hepatitis C" (Press release). U.S. Food and Drug Administration (FDA). December 19, 2014. Archived from the original on October 31, 2015.
- ^ Akinosoglou K, Schinas G, Gogos C (November 2022). "Oral Antiviral Treatment for COVID-19: A Comprehensive Review on Nirmatrelvir/Ritonavir". Viruses. 14 (11): 2540. doi:10.3390/v14112540. PMC 9696049. PMID 36423149.
- ^ "Ritonavir Pregnancy and Breastfeeding Warnings". drugs.com. Archived from the original on September 7, 2015. Retrieved October 23, 2015.
- ^ a b British National Formulary 69 (69 ed.). Pharmaceutical Pr. March 31, 2015. p. 426. ISBN 9780857111562.
- ^ Hacker M (2009). Pharmacology principles and practice. Amsterdam: Academic Press/Elsevier. p. 550. ISBN 9780080919225. Archived from the original on June 17, 2020. Retrieved September 10, 2017.
- ^ Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 509. ISBN 9783527607495. Archived from the original on June 20, 2021. Retrieved August 27, 2020.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- ^ "First Generic Drug Approvals". U.S. Food and Drug Administration (FDA). Archived from the original on January 26, 2021. Retrieved February 13, 2021.
- ^ "Ritonavir - Patient". clinicalinfo.hiv.gov. Retrieved January 11, 2023.
- ^ "Ritonavir". go.drugbank.com. Retrieved January 11, 2023.
- ^ "Protease". clinicalinfo.hiv.gov. Retrieved January 11, 2023.
- ^ a b Zhu KW (September 2023). "Deuremidevir and Simnotrelvir-Ritonavir for the Treatment of COVID-19". ACS Pharmacology & Translational Science. 6 (9): 1306–1309. doi:10.1021/acsptsci.3c00134. PMC 10496140. PMID 37705591.
- ^ "Paxlovid- nirmatrelvir and ritonavir kit". DailyMed. Archived from the original on December 31, 2021. Retrieved December 30, 2021.
- ^ a b c "FDA Authorizes First Oral Antiviral for Treatment of COVID-19". U.S. Food and Drug Administration (FDA) (Press release). December 22, 2021. Archived from the original on December 27, 2021. Retrieved December 22, 2021.
- ^ a b "Pfizer Receives U.S. FDA Emergency Use Authorization for Novel COVID-19 Oral Antiviral Treatment" (Press release). Pfizer. December 22, 2021. Archived from the original on December 22, 2021. Retrieved December 22, 2021 – via Business Wire.
- ^ "Frequently Asked Questions on the Emergency Use Authorization for Paxlovid for Treatment of COVID-19" (PDF). U.S. Food and Drug Administration (FDA). December 22, 2021. Archived from the original on January 5, 2022. Retrieved January 3, 2022.
- ^ "Oral COVID-19 antiviral, Paxlovid, approved by UK regulator" (Press release). Medicines and Healthcare products Regulatory Agency. December 31, 2021. Archived from the original on January 11, 2022. Retrieved January 3, 2022.
- ^ Reed J (December 31, 2021). "Paxlovid: UK medicines regulator approves second Covid antiviral pill". BBC News Online. Archived from the original on January 1, 2022. Retrieved January 3, 2022.
- ^ Yeh RF, Gaver VE, Patterson KB, Rezk NL, Baxter-Meheux F, Blake MJ, et al. (May 2006). "Lopinavir/ritonavir induces the hepatic activity of cytochrome P450 enzymes CYP2C9, CYP2C19, and CYP1A2 but inhibits the hepatic and intestinal activity of CYP3A as measured by a phenotyping drug cocktail in healthy volunteers". Journal of Acquired Immune Deficiency Syndromes. 42 (1): 52–60. doi:10.1097/01.qai.0000219774.20174.64. PMID 16639344. S2CID 39632668.
- ^ "Ritonavir: Drug Information Provided by Lexi-Comp: Merck Manual Professional". Merck Manuals Professional Edition. April 30, 2008. Archived from the original on April 30, 2008.
- ^ Stader F, Khoo S, Stoeckle M, Back D, Hirsch HH, Battegay M, Marzolini C (October 2020). "Stopping lopinavir/ritonavir in COVID-19 patients: duration of the drug interacting effect". The Journal of Antimicrobial Chemotherapy. 75 (10): 3084–3086. doi:10.1093/jac/dkaa253. PMC 7337877. PMID 32556272.
- ^ Carpenter M, Berry H, Pelletier AL (May 2019). "Clinically Relevant Drug-Drug Interactions in Primary Care". American Family Physician. 99 (9): 558–564. PMID 31038898.
- ^ a b WO 1994014436, Kempf DJ, Norbeck DW, Sham HL, Zhao C, Sowin TJ, Reno DS, Haight AR, Cooper AJ, "Retroviral protease inhibiting compounds", published July 7, 1994, assigned to Abbott Laboratories.
- ^ Kempf DJ, Norbeck DW, Codacovi L, Wang XC, Kohlbrenner WE, Wideburg NE, et al. (October 1990). "Structure-based, C2 symmetric inhibitors of HIV protease". Journal of Medicinal Chemistry. 33 (10): 2687–2689. doi:10.1021/jm00172a002. PMID 2213822.
- ^ Zeldin RK, Petruschke RA (January 2004). "Pharmacological and therapeutic properties of ritonavir-boosted protease inhibitor therapy in HIV-infected patients". The Journal of Antimicrobial Chemotherapy. 53 (1): 4–9. doi:10.1093/jac/dkh029. PMID 14657084.
- ^ Merry C, Barry MG, Mulcahy F, Ryan M, Heavey J, Tjia JF, et al. (March 1997). "Saquinavir pharmacokinetics alone and in combination with ritonavir in HIV-infected patients". AIDS. 11 (4): F29 – F33. doi:10.1097/00002030-199704000-00001. PMID 9084785.
- ^ "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". U.S. Food and Drug Administration (FDA). December 3, 2019. Archived from the original on March 12, 2020. Retrieved February 17, 2020.
- ^ a b Kempf DJ, Sham HL, Marsh KC, Flentge CA, Betebenner D, Green BE, et al. (February 1998). "Discovery of ritonavir, a potent inhibitor of HIV protease with high oral bioavailability and clinical efficacy". Journal of Medicinal Chemistry. 41 (4): 602–617. doi:10.1021/jm970636+. PMID 9484509.
- ^ Vardanyan R, Hruby V (2016). "34: Antiviral Drugs". Synthesis of Best-Seller Drugs. pp. 698–701. doi:10.1016/B978-0-12-411492-0.00034-1. ISBN 9780124114920. S2CID 75449475.
- ^ a b c Centers for Disease Control Prevention (CDC) (June 2011). "HIV surveillance--United States, 1981-2008" (PDF). MMWR. Morbidity and Mortality Weekly Report. 60 (21): 689–93. PMID 21637182. Archived from the original (PDF) on September 24, 2015.
- ^ "Ritonavir FDA approval package" (PDF). March 1, 1996. Archived (PDF) from the original on March 1, 2021. Retrieved August 20, 2020.
- ^ "FDA Approval of HIV Medicines". HIVINFO. Retrieved September 29, 2022.
- ^ Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. (May 2020). "A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19". The New England Journal of Medicine. 382 (19): 1787–1799. doi:10.1056/NEJMoa2001282. PMC 7121492. PMID 32187464.
- ^ Bagheri M, Niavarani A (October 2020). "Molecular dynamics analysis predicts ritonavir and naloxegol strongly block the SARS-CoV-2 spike protein-hACE2 binding". Journal of Biomolecular Structure & Dynamics. 40 (4): 1597–1606. doi:10.1080/07391102.2020.1830854. PMID 33030105. S2CID 222217607.
- ^ Vandyck K, Deval J (August 2021). "Considerations for the discovery and development of 3-chymotrypsin-like cysteine protease inhibitors targeting SARS-CoV-2 infection". Current Opinion in Virology. 49: 36–40. doi:10.1016/j.coviro.2021.04.006. PMC 8075814. PMID 34029993.
- ^ Schooley RT, Carlin AF, Beadle JR, Valiaeva N, Zhang XQ, Clark AE, et al. (September 2021). "Rethinking Remdesivir: Synthesis, Antiviral Activity, and Pharmacokinetics of Oral Lipid Prodrugs". Antimicrobial Agents and Chemotherapy. 65 (10): e0115521. doi:10.1128/AAC.01155-21. ISSN 0066-4804. PMC 8448143. PMID 34310217. S2CID 236450769.
- ^ Ahmad B, Batool M, Ain QU, Kim MS, Choi S (August 2021). "Exploring the Binding Mechanism of PF-07321332 SARS-CoV-2 Protease Inhibitor through Molecular Dynamics and Binding Free Energy Simulations". International Journal of Molecular Sciences. 22 (17): 9124. doi:10.3390/ijms22179124. PMC 8430524. PMID 34502033.
- ^ "Pfizer begins dosing in Phase II/III trial of antiviral drug for Covid-19". Clinical Trials Arena. September 2, 2021. Archived from the original on November 5, 2021. Retrieved November 5, 2021.
- ^ Woodley M (October 19, 2021). "What is Australia's potential new COVID treatment?". Newsgp. Archived from the original on November 5, 2021. Retrieved November 6, 2021.
- ^ "Pfizer's Novel COVID-19 Oral Antiviral Treatment Candidate Reduced Risk Of Hospitalization Or Death By 89% In Interim Analysis Of Phase 2/3 EPIC-HR Study". November 5, 2021. Archived from the original on November 16, 2021. Retrieved November 17, 2021.
- ^ Weintraub K (November 5, 2021). "Pfizer antiviral drug could nearly end deaths from COVID-19, company study suggests". USA Today. Archived from the original on November 5, 2021. Retrieved November 5, 2021.
- ^ a b Bauer J, Spanton S, Henry R, Quick J, Dziki W, Porter W, Morris J (June 2001). "Ritonavir: an extraordinary example of conformational polymorphism". Pharmaceutical Research. 18 (6): 859–866. doi:10.1023/A:1011052932607. PMID 11474792. S2CID 20923508.
- ^ a b Morissette SL, Soukasene S, Levinson D, Cima MJ, Almarsson O (March 2003). "Elucidation of crystal form diversity of the HIV protease inhibitor ritonavir by high-throughput crystallization". Proceedings of the National Academy of Sciences of the United States of America. 100 (5): 2180–2184. doi:10.1073/pnas.0437744100. PMC 151315. PMID 12604798.
- ^ Lüttge A (February 1, 2006). "Crystal dissolution kinetics and Gibbs free energy". Journal of Electron Spectroscopy and Related Phenomena. 150 (2): 248–259. Bibcode:2006JESRP.150..248L. doi:10.1016/j.elspec.2005.06.007.
- ^ Bučar DK, Lancaster RW, Bernstein J (June 2015). "Disappearing polymorphs revisited". Angewandte Chemie. 54 (24): 6972–6993. doi:10.1002/anie.201410356. PMC 4479028. PMID 26031248.
- ^ "Kaletra FAQ". AbbVie's Kaletra product information. AbbVie. 2011. Archived from the original on July 7, 2014. Retrieved July 5, 2014.
- ^ Zhang C, Matzger AJ (February 2017). "A Newly Discovered Racemic Compound of Pioglitazone Hydrochloride Is More Stable than the Commercial Conglomerate". Crystal Growth & Design. 17 (2): 414–417. Bibcode:2017CrGrD..17..414Z. doi:10.1021/acs.cgd.6b01638. PMC 6752731. PMID 31537981.
- ^ Connolly C (August 5, 2004). "NIH Declines to Enter AIDS Drug Price Battle". The Washington Post. Archived from the original on August 20, 2008. Retrieved January 16, 2006.
Further reading
[edit]- Chemburkar SR, Bauer J, Deming K, Spiwek H, Patel K, Morris J, et al. (2000). "Dealing with the Impact of Ritonavir Polymorphs on the Late Stages of Bulk Drug Process Development". Organic Process Research & Development. 4 (5): 413–417. doi:10.1021/op000023y.