Platelet-derived growth factor receptor A
Platelet-derived growth factor receptor A, also termed CD140a, is a receptor located on the surface of a wide range of cell types. The protein is encoded in the human by the PDGFRA gene. This receptor binds to certain isoforms of platelet-derived growth factors (PDGFs) and thereby becomes active in stimulating cell signaling pathways that elicit responses such as cellular growth and differentiation. The receptor is critical for the embryonic development of certain tissues and organs, and for their maintenance, particularly hematologic tissues, throughout life. Mutations in PDGFRA, are associated with an array of clinically significant neoplasms, notably ones of the clonal hypereosinophilia class of malignancies, as well as gastrointestinal stromal tumors (GISTs).
Overall structure
[edit]This gene encodes a typical receptor tyrosine kinase, which is a transmembrane protein consisting of an extracellular ligand binding domain, a transmembrane domain and an intracellular tyrosine kinase domain. The molecular mass of the mature, glycosylated PDGFRα protein is approximately 170 kDA. cell surface tyrosine kinase receptor for members of the platelet-derived growth factor family.
Modes of activation
[edit]Activation of PDGFRA requires de-repression of the receptor's kinase activity. The ligand for PDGFRα (PDGF) accomplishes this in the course of assembling a PDGFRα dimer. Four of the five PDGF isoforms activate PDGFRα (PDGF-A, PDGF-B, PDGF-AB and PDGF-C). The activated receptor phosphorylates itself and other proteins, and thereby engages intracellular signaling pathways that trigger cellular responses such as migration and proliferation.
There are also PDGF-independent modes of de-repressing the PDGFRα's kinase activity and hence activating it. For instance, forcing PDGFRα into close proximity of each other by overexpression or with antibodies directed against the extracellular domain. Alternatively, mutations in the kinase domain that stabilize a kinase active conformation result in constitutive activation. Finally, growth factors outside of the PDGFR family (non-PDGFs) activate PDGFRα indirectly.[5] Non-PDGFs bind to their own receptors that trigger intracellular events that de-repress the kinase activity of PDGFRα monomers. The intracellular events by which non-PDGFs indirectly activate PDGFRα include elevation of reactive oxygen species that activate Src family kinases, which phosphorylate PDGFRα.
The mode of activation determines the duration that PDGFRα remains active. The PDGF-mediated mode, which dimerized PDGFRα, accelerates internalization and degradation of activated PDGFRα such that the half-life of PDGF-activated PDGFRα is approximately 5 min.[6][7] Enduring activation of PDGFRα (half-life greater than 120 min) occurs when PDGFRα monomers are activated.[8]
Role in physiology/pathology
[edit]The importance of PDGFRA during development is apparent from the observation that the majority of mice lacking a functional Pdgfra gene develop a plethora of embryonic defects, some of which are lethal; the mutant mice exhibit defects in kidney glomeruli because of a lack of mesangial cells but also suffer an ill-defined blood defect characterized by thrombocytopenic, a bleeding tendency, and severe anemia which could be due to blood loss. The mice die at or shortly before birth.[9] PDGF-A and PDGF-C seem to be the important activators of PDGFRα during development because mice lacking functional genes for both these PDGFRA activating ligands, i.e. Pdgfa/Pdgfc- double null mice show similar defects to Pdgra null mice.[10] Mice genetically engineered to express a constitutively (i.e. continuously) activated PDGFRα mutant receptor eventually develop fibrosis in the skin and multiple internal organs.[11] The studies suggest that PDGFRA plays fundamental roles in the development and function of mesodermal tissues, e.g., blood cells, connective tissue, and mesangial cells.
Clinical significance
[edit]PDGFRA mutations
[edit]Myeloid and lymphoid cells
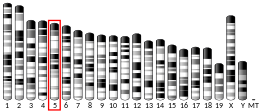
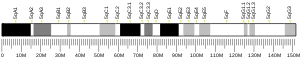
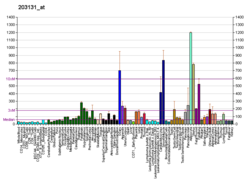
[edit]Somatic mutations that cause the fusion of the PDGFRA gene with certain other genes occur in hematopoietic stem cells and cause a hematological malignancy in the clonal hypereosinophilia class of malignancies. These mutations create fused genes which encode chimeric proteins that possess continuously active PDGFRA-derived tyrosine kinase. They thereby continuously stimulate cell growth and proliferation and lead to the development of leukemias, lymphomas, and myelodysplastic syndromes that are commonly associated with hypereosinophilia and therefore regarded as a sub-type of clonal eosinophilia. In the most common of these mutations, the PDGFRA gene on human chromosome 4 at position q12 (notated as 4q12) fuses with the FIP1L1 gene also located at position 4q12. This interstitial (i.e. on the same chromosome) fusion creates a FIP1L1-PDGFRA fusion gene while usually losing intervening genetic material, typically including either the CHIC2[12] or LNX gene. The fused gene encodes a FIP1L1-PDGFRA protein that causes: a) chronic eosinophilia which progresses to chronic eosinophilic leukemia; b) a form of myeloproliferative neoplasm/myeloblastic leukemia associated with little or no eosinophilia; c) T-lymphoblastic leukemia/lymphoma associated with eosinophilia; d) myeloid sarcoma with eosinophilia (see FIP1L1-PDGFRA fusion genes); or e) mixtures of these presentations. Variations in the type of malignancy formed likely reflects the specific type(s) of hematopoietic stem cells that bear the mutation.[13][14][15][16] The PDGFRA gene may also mutate through any one of several chromosome translocations to create fusion genes which, like the Fip1l1-PDGFRA fusion gene, encode a fusion protein that possesses continuously active PDGFRA-related tyrosine kinase and causes myeloid and/or lymphoid malignancies. These mutations, including the Fip1l1-PDGFRA mutation, along with the chromosomal location of PDGFRA's partner and the notation used to identify the fused gene are given in the following table.[13][14][17][18]
| Gene | locus | notation | gene | locus | notation | Gene | locus | notation | gene | locus | notation | gene | locus | notation | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FIP1L1 | 4q12 | t(4;4)(q12;q12) | KIF5B | 10p11 | t(4;11)(q12;p11) | CDK5RAP2 | 9q33 | t(5;9)(q12;q33) | STRN | 2p24 | t(2;4)(q24-p12) | ETV6 | 12p13.2 | (4;12)(q2?3;p1?2) | |||
| FOXP1 | 3p14 | t(3;4)(q14;p12 | TNKS2 | 10q23 | t(4;10)(q12;q23) | BCR | 22q11 | t(4;22)(q12;q11) | JAK2 | 9p24 | t(4;9)(q12-p24) |
Patients afflicted with any one of these translocation mutations, similar to those afflicted with the interstitial PDGFRA-FIP1l1 fusion gene: a) present with findings of chronic eosinophilia, hypereosinophilia, the hypereosinophilic syndrome, or chronic eosinophilic leukemia; myeloproliferative neoplasm/myeloblastic leukemia; a T-lymphoblastic leukemia/lymphoma; or myeloid sarcoma; b) are diagnosed cytogenetically, usually by analyses that detect breakpoints in the short arm of chromosome 4 using Fluorescence in situ hybridization; and c) where treated (many of the translocations are extremely rare and have not be fully tested for drug sensitivity), respond well or are anticipated to respond well to imatinib therapy as described for the treatment of diseases caused by FIP1L1-PDGFRA fusion genes.[13][14][15]
Gastrointestinal tract
[edit]Activating mutations in PDGFRA are also involved in the development of 2–15% of gastrointestinal stromal tumors (GISTs), which is the most common mesenchymal neoplasm of the gastrointestinal tract. GIST tumors are sarcomas derived from the GI tract's connective tissue whereas most GI tract tumors are adenocarcinomas derived from the tract's epithelium cells. GIST tumors occur throughout the GI tract but most (66%) occur in the stomach and when developing there have a lower malignant potential than GIST tumors found elsewhere in the GI tract. The most common PDGFRA mutations found in GIST tumors occur in exon 18 and are thought to stabilize PDGFRA's tyrosine kinase in an activated conformation. A single mutation, D842V, in this exon accounts for >70% of GIST tumors. The next most common GIST tumor mutation occurs in exon 18, accounts for <1% of GISTs tumors, and is a deletion of codons 842 to 845. Exon 12 is the second most commonly mutated PDGFRA exon in GIST, being found in ~1% of GIST tumors. Mutations in PDGFRA's exon 14 are found in <1% of GIST tumors. While some PDGFRA mutation-induced GIST tumors are sensitive to the tyrosine kinase inhibitor, imatinib, the most common mutation, D842V, as well as some very rare mutations are resistant to this drug: median overall survival is reported to be only 12.8 months in patients whose tumors bear the D842V mutation compared to 48–60 months in large series of imatinib-treated patients with other types of GIST mutations. Consequently, it is critical to define the exact nature of PDGFR-induced mutant GIST tumors in order to select appropriate therapy particularly because a novel PDGFRA selective kinase inhibitor, crenolanib, is under investigation for treating D842V-induced and other imatinib-resistant GIST tumors.[19] A randomized trial testing the efficacy of crenolanib in patients with GIST tumors bearing the D842V mutation is under recruitment.[20]
Olaratumab (LY3012207) is a human IgG1 monoclonal antibody designed to bind to human PDGFRα with high affinity and block PDGF-AA, PDGF-BB, and PDGF-CC ligands from binding to the receptor. Numerous studies using it to treat soft tissue sarcomas including GIST are ongoing. Studies on GIST have focused on inoperable, metastatic, and/or recurrent disease and have tested olagatumab with Doxorubicin versus doxorubicin along.[21] The US FDA granted approval for the use of olaratumab-dcoxorbicin therapy of soft tissue sarcomas under its Accelerated Approval Program based on the results of the phase II trial, (NCT01185964). In addition, the European Medicines Agency granted conditional approval for olaratumab in this indication in November 2016 following a review under the EMA's Accelerated Assessment Program.[22]
Nervous system
[edit]Gain-of-function H3K27M mutations in protein histone H3 lead to inactivation of polycomb repressive complex 2 (PRC2) methyltransferase and result in global hypomethylation of H3K27me3 and transcriptional derepression of potential oncogenes. About 40% of these mutation are associated with gain of function or amplifications mutations in the PDGFRA gene in cases of pediatric diffuse Gliomas of the pons. It appears that the initial histone H3 mutations alone are insufficient but rather require cooperating secondary mutations such as PDGFRA-activating mutations or PDGFRA amplifications to develop this type of brain tumor.[23] In a small non-randomized trial study, imatinib therapy in patients with glioblastoma selected on the basis of having imatinib-inhibitable tyrosine kinases in biopsy tissue caused marginal disease improvement compared to similar treatment of patients with unselected recurrent glioblastoma. This suggests that patient sub-populations with excessive PDGFRA-related or other tyrosine kinase-related over-activity might benefit from imatinib therapy.[24] Several phase I and Phase II clinical glioma/glioblastoma studies have been conducted using imatinib but no decisive follow-up phase III studies have been reported.[25]
Interactions
[edit]PDGFRA has been shown to interact with:
Notes
[edit]
The 2017 version of this article was updated by an external expert under a dual publication model. The corresponding academic peer reviewed article was published in Gene and can be cited as: Andrius Kazlauskas (3 March 2017). "PDGFs and their receptors". Gene. Gene Wiki Review Series. 614: 1–7. doi:10.1016/J.GENE.2017.03.003. ISSN 0378-1119. PMC 6728141. PMID 28267575. Wikidata Q39166181. |
See also
[edit]References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000134853 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000029231 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Lei H, Kazlauskas A (March 2009). "Growth factors outside of the platelet-derived growth factor (PDGF) family employ reactive oxygen species/Src family kinases to activate PDGF receptor alpha and thereby promote proliferation and survival of cells". The Journal of Biological Chemistry. 284 (10): 6329–6336. doi:10.1074/jbc.M808426200. PMC 2649107. PMID 19126548.
- ^ Rosenkranz S, Ikuno Y, Leong FL, Klinghoffer RA, Miyake S, Band H, Kazlauskas A (March 2000). "Src family kinases negatively regulate platelet-derived growth factor alpha receptor-dependent signaling and disease progression". The Journal of Biological Chemistry. 275 (13): 9620–9627. doi:10.1074/jbc.275.13.9620. PMID 10734113.
- ^ Avrov K, Kazlauskas A (December 2003). "The role of c-Src in platelet-derived growth factor alpha receptor internalization". Experimental Cell Research. 291 (2): 426–434. doi:10.1016/j.yexcr.2003.08.001. PMID 14644164.
- ^ Lei H, Kazlauskas A (January 2014). "A reactive oxygen species-mediated, self-perpetuating loop persistently activates platelet-derived growth factor receptor α". Molecular and Cellular Biology. 34 (1): 110–122. doi:10.1128/MCB.00839-13. PMC 3911282. PMID 24190966.
- ^ Soriano P (August 1994). "Abnormal kidney development and hematological disorders in PDGF beta-receptor mutant mice". Genes & Development. 8 (16): 1888–1896. doi:10.1101/gad.8.16.1888. PMID 7958864.
- ^ Ding H, Wu X, Boström H, Kim I, Wong N, Tsoi B, et al. (October 2004). "A specific requirement for PDGF-C in palate formation and PDGFR-alpha signaling". Nature Genetics. 36 (10): 1111–1116. doi:10.1038/ng1415. PMID 15361870.
- ^ Olson LE, Soriano P (February 2009). "Increased PDGFRalpha activation disrupts connective tissue development and drives systemic fibrosis". Developmental Cell. 16 (2): 303–313. doi:10.1016/j.devcel.2008.12.003. PMC 2664622. PMID 19217431.
- ^ "CHIC2 cysteine rich hydrophobic domain 2 [Homo sapiens (Human)] - Gene - NCBI".
- ^ a b c Vega F, Medeiros LJ, Bueso-Ramos CE, Arboleda P, Miranda RN (September 2015). "Hematolymphoid neoplasms associated with rearrangements of PDGFRA, PDGFRB, and FGFR1". American Journal of Clinical Pathology. 144 (3): 377–392. doi:10.1309/AJCPMORR5Z2IKCEM. PMID 26276769.
- ^ a b c Reiter A, Gotlib J (February 2017). "Myeloid neoplasms with eosinophilia". Blood. 129 (6): 704–714. doi:10.1182/blood-2016-10-695973. PMID 28028030.
- ^ a b Gotlib J (November 2015). "World Health Organization-defined eosinophilic disorders: 2015 update on diagnosis, risk stratification, and management". American Journal of Hematology. 90 (11): 1077–1089. doi:10.1002/ajh.24196. PMID 26486351. S2CID 42668440.
- ^ Boyer DF (October 2016). "Blood and Bone Marrow Evaluation for Eosinophilia". Archives of Pathology & Laboratory Medicine. 140 (10): 1060–1067. doi:10.5858/arpa.2016-0223-RA. PMID 27684977.
- ^ Appiah-Kubi K, Lan T, Wang Y, Qian H, Wu M, Yao X, et al. (January 2017). "Platelet-derived growth factor receptors (PDGFRs) fusion genes involvement in hematological malignancies". Critical Reviews in Oncology/Hematology. 109: 20–34. doi:10.1016/j.critrevonc.2016.11.008. PMID 28010895.
- ^ De Braekeleer E, Douet-Guilbert N, Morel F, Le Bris MJ, Basinko A, De Braekeleer M (August 2012). "ETV6 fusion genes in hematological malignancies: a review". Leukemia Research. 36 (8): 945–961. doi:10.1016/j.leukres.2012.04.010. PMID 22578774.
- ^ Barnett CM, Corless CL, Heinrich MC (October 2013). "Gastrointestinal stromal tumors: molecular markers and genetic subtypes". Hematology/Oncology Clinics of North America. 27 (5): 871–888. doi:10.1016/j.hoc.2013.07.003. PMID 24093165.
- ^ "CTG Labs - NCBI".
- ^ "CTG Labs - NCBI".
- ^ Shirley M (January 2017). "Olaratumab: First Global Approval". Drugs. 77 (1): 107–112. doi:10.1007/s40265-016-0680-2. PMID 27995580. S2CID 3604814.
- ^ Vanan MI, Underhill DA, Eisenstat DD (April 2017). "Targeting Epigenetic Pathways in the Treatment of Pediatric Diffuse (High Grade) Gliomas". Neurotherapeutics. 14 (2): 274–283. doi:10.1007/s13311-017-0514-2. PMC 5398987. PMID 28233220.
- ^ Hassler MR, Vedadinejad M, Flechl B, Haberler C, Preusser M, Hainfellner JA, et al. (2014). "Response to imatinib as a function of target kinase expression in recurrent glioblastoma". SpringerPlus. 3: 111. doi:10.1186/2193-1801-3-111. PMC 4320134. PMID 25674429.
- ^ "CTG Labs - NCBI".
- ^ Yokote K, Hellman U, Ekman S, Saito Y, Rönnstrand L, Saito Y, et al. (March 1998). "Identification of Tyr-762 in the platelet-derived growth factor alpha-receptor as the binding site for Crk proteins". Oncogene. 16 (10): 1229–1239. doi:10.1038/sj.onc.1201641. PMID 9546424. S2CID 23147812.
- ^ Matsumoto T, Yokote K, Take A, Takemoto M, Asaumi S, Hashimoto Y, et al. (April 2000). "Differential interaction of CrkII adaptor protein with platelet-derived growth factor alpha- and beta-receptors is determined by its internal tyrosine phosphorylation". Biochemical and Biophysical Research Communications. 270 (1): 28–33. doi:10.1006/bbrc.2000.2374. PMID 10733900.
- ^ Yamamoto M, Toya Y, Jensen RA, Ishikawa Y (March 1999). "Caveolin is an inhibitor of platelet-derived growth factor receptor signaling". Experimental Cell Research. 247 (2): 380–388. doi:10.1006/excr.1998.4379. PMID 10066366.
- ^ Bonita DP, Miyake S, Lupher ML, Langdon WY, Band H (August 1997). "Phosphotyrosine binding domain-dependent upregulation of the platelet-derived growth factor receptor alpha signaling cascade by transforming mutants of Cbl: implications for Cbl's function and oncogenicity". Molecular and Cellular Biology. 17 (8): 4597–4610. doi:10.1128/mcb.17.8.4597. PMC 232313. PMID 9234717.
- ^ Gilbertson DG, Duff ME, West JW, Kelly JD, Sheppard PO, Hofstrand PD, et al. (July 2001). "Platelet-derived growth factor C (PDGF-C), a novel growth factor that binds to PDGF alpha and beta receptor". The Journal of Biological Chemistry. 276 (29): 27406–27414. doi:10.1074/jbc.M101056200. PMID 11297552.
- ^ Rupp E, Siegbahn A, Rönnstrand L, Wernstedt C, Claesson-Welsh L, Heldin CH (October 1994). "A unique autophosphorylation site in the platelet-derived growth factor alpha receptor from a heterodimeric receptor complex". European Journal of Biochemistry. 225 (1): 29–41. doi:10.1111/j.1432-1033.1994.00029.x. PMID 7523122.
- ^ Seifert RA, Hart CE, Phillips PE, Forstrom JW, Ross R, Murray MJ, Bowen-Pope DF (May 1989). "Two different subunits associate to create isoform-specific platelet-derived growth factor receptors". The Journal of Biological Chemistry. 264 (15): 8771–8778. doi:10.1016/S0021-9258(18)81860-9. PMID 2542288.
- ^ Eriksson A, Nånberg E, Rönnstrand L, Engström U, Hellman U, Rupp E, et al. (March 1995). "Demonstration of functionally different interactions between phospholipase C-gamma and the two types of platelet-derived growth factor receptors". The Journal of Biological Chemistry. 270 (13): 7773–7781. doi:10.1074/jbc.270.13.7773. PMID 7535778.
- ^ Maudsley S, Zamah AM, Rahman N, Blitzer JT, Luttrell LM, Lefkowitz RJ, Hall RA (November 2000). "Platelet-derived growth factor receptor association with Na(+)/H(+) exchanger regulatory factor potentiates receptor activity". Molecular and Cellular Biology. 20 (22): 8352–8363. doi:10.1128/mcb.20.22.8352-8363.2000. PMC 102142. PMID 11046132.
Further reading
[edit]- Olson LE, Soriano P (February 2009). "Increased PDGFRalpha activation disrupts connective tissue development and drives systemic fibrosis". Developmental Cell. 16 (2): 303–313. doi:10.1016/j.devcel.2008.12.003. PMC 2664622. PMID 19217431.
- Heinrich MC, Corless CL, Duensing A, McGreevey L, Chen CJ, Joseph N, et al. (January 2003). "PDGFRA activating mutations in gastrointestinal stromal tumors". Science. 299 (5607): 708–710. Bibcode:2003Sci...299..708H. doi:10.1126/science.1079666. PMID 12522257. S2CID 11725958.
- Soriano P (July 1997). "The PDGF alpha receptor is required for neural crest cell development and for normal patterning of the somites". Development. 124 (14): 2691–2700. doi:10.1242/dev.124.14.2691. PMID 9226440.
- Ding H, Wu X, Boström H, Kim I, Wong N, Tsoi B, et al. (October 2004). "A specific requirement for PDGF-C in palate formation and PDGFR-alpha signaling". Nature Genetics. 36 (10): 1111–1116. doi:10.1038/ng1415. PMID 15361870.
- Heinrich MC, Corless CL, Demetri GD, Blanke CD, von Mehren M, Joensuu H, et al. (December 2003). "Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor". Journal of Clinical Oncology. 21 (23): 4342–4349. doi:10.1200/JCO.2003.04.190. PMID 14645423.
- Heldin CH (December 2013). "Targeting the PDGF signaling pathway in tumor treatment". Cell Communication and Signaling. 11: 97. doi:10.1186/1478-811X-11-97. PMC 3878225. PMID 24359404.
- Andrae J, Gallini R, Betsholtz C (May 2008). "Role of platelet-derived growth factors in physiology and medicine". Genes & Development. 22 (10): 1276–1312. doi:10.1101/gad.1653708. PMC 2732412. PMID 18483217.
- Lewandowski SA, Fredriksson L, Lawrence DA, Eriksson U (November 2016). "Pharmacological targeting of the PDGF-CC signaling pathway for blood-brain barrier restoration in neurological disorders". Pharmacology & Therapeutics. 167: 108–119. doi:10.1016/j.pharmthera.2016.07.016. PMC 5341142. PMID 27524729.
- Pennock S, Kim LA, Kazlauskas A (September 2016). "Vascular Endothelial Cell Growth Factor A Acts via Platelet-Derived Growth Factor Receptor α To Promote Viability of Cells Enduring Hypoxia". Molecular and Cellular Biology. 36 (18): 2314–2327. doi:10.1128/MCB.01019-15. PMC 5007796. PMID 27325673.
- Lei H, Velez G, Hovland P, Hirose T, Gilbertson D, Kazlauskas A (July 2009). "Growth factors outside the PDGF family drive experimental PVR". Investigative Ophthalmology & Visual Science. 50 (7): 3394–3403. doi:10.1167/iovs.08-3042. PMC 2798136. PMID 19324843.
- Lei H, Rheaume MA, Cui J, Mukai S, Maberley D, Samad A, et al. (September 2012). "A novel function of p53: a gatekeeper of retinal detachment". The American Journal of Pathology. 181 (3): 866–874. doi:10.1016/j.ajpath.2012.05.036. PMC 3432438. PMID 22901751.
- Hart CE, Bowen-Pope DF (June 1990). "Platelet-derived growth factor receptor: current views of the two-subunit model". The Journal of Investigative Dermatology. 94 (6 Suppl): 53S – 57S. doi:10.1111/1523-1747.ep12875065. PMID 2161888.
- Corless CL, Schroeder A, Griffith D, Town A, McGreevey L, Harrell P, et al. (August 2005). "PDGFRA mutations in gastrointestinal stromal tumors: frequency, spectrum and in vitro sensitivity to imatinib". Journal of Clinical Oncology. 23 (23): 5357–5364. doi:10.1200/JCO.2005.14.068. PMID 15928335.
- Lasota J, Miettinen M (May 2006). "KIT and PDGFRA mutations in gastrointestinal stromal tumors (GISTs)". Seminars in Diagnostic Pathology. 23 (2): 91–102. doi:10.1053/j.semdp.2006.08.006. PMID 17193822.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.