Adrenaline: Difference between revisions
No edit summary |
No edit summary |
||
| Line 34: | Line 34: | ||
| PubChem = 5816 |
| PubChem = 5816 |
||
| IUPHAR_ligand = 479 |
| IUPHAR_ligand = 479 |
||
| IUPHAR_ligand = 509 |
|||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} |
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} |
||
| DrugBank = DB00668 |
| DrugBank = DB00668 |
||
Revision as of 15:17, 16 August 2012
 | |
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603002 |
| Pregnancy category |
|
| Routes of administration | IV, IM, endotracheal, IC |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Nil (oral) |
| Metabolism | adrenergic synapse (MAO and COMT) |
| Elimination half-life | 2 minutes |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.090 |
| Chemical and physical data | |
| Formula | C9H13NO3 |
| Molar mass | 183.204 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Epinephrine (also known as adrenaline or adrenalin) is a hormone and a neurotransmitter.[1] Epinephrine has many functions in the body, regulating heart rate, blood vessel and air passage diameters, and metabolic shifts; epinephrine release is a crucial component of the fight-or-flight response of the sympathetic nervous system.[2] In chemical terms, epinephrine is one of a group of monoamines called the catecholamines. It is produced in some neurons of the central nervous system, and in the chromaffin cells of the adrenal medulla from the amino acids phenylalanine and tyrosine.[3]
Terminology
This chemical is widely referred to as "adrenaline" outside the United States; however, its United States Adopted Name and International Nonproprietary Name is epinephrine. Epinephrine was chosen as the generic name in the United States because John Abel, who prepared extracts from the adrenal glands in 1897, used that name for his extracts.[4] In 1901, Jokichi Takamine patented a purified adrenal extract, and called it "adrenalin", which was trademarked by Parke, Davis & Co in the U.S.[4] In the belief that Abel's extract was the same as Takamine's, a belief since disputed, epinepherine became the generic name in the U.S.[4] The British Approved Name and European Pharmacopoeia term for this chemical is adrenaline and is indeed now one of the few differences between the INN and BAN systems of names.[5]
Among American health professionals and scientists, the term epinephrine is used over adrenaline. However, pharmaceuticals that mimic the effects of epinephrine are often called adrenergics, and receptors for epinephrine are called adrenergic receptors or adrenoceptors.
Discovery
Extracts of the adrenal gland were first obtained by Polish physiologist Napoleon Cybulski in 1895. These extracts, which he called nadnerczyna, contained adrenaline and other catecholamines.[6] Japanese chemist Jokichi Takamine and his assistant Keizo Uenaka independently discovered adrenaline in 1900.[7][8] In 1901, Takamine successfully isolated and purified the hormone from the adrenal glands of sheep and oxen.[9] Adrenaline was first synthesized in the laboratory by Friedrich Stolz and Henry Drysdale Dakin, independently, in 1904.[8]
Mechanism of action
| Organ | Effects |
|---|---|
| Heart | Increases heart rate |
| Lungs | Increases respiratory rate |
| Systemic | Vasoconstriction or vasodilation |
| Liver | Stimulates glycogenolysis |
| Systemic | Triggers lipolysis |
| Systemic | Muscle contraction |
As a hormone and neurotransmitter, adrenaline acts on nearly all body tissues. Its actions vary by tissue type and tissue expression of adrenergic receptors. For example, high levels of adrenaline causes smooth muscle relaxation in the airways but causes contraction of the smooth muscle that lines most arterioles.
Adrenaline acts by binding to a variety of adrenergic receptors. Adrenaline is a nonselective agonist of all adrenergic receptors, including the major subtypes α1, α2, β1, β2, and β3.[10] Epinephrine's binding to these receptors triggers a number of metabolic changes. Binding to α-adrenergic receptors inhibits insulin secretion by the pancreas, stimulates glycogenolysis in the liver and muscle, and stimulates glycolysis in muscle.[11] β-Adrenergic receptor binding triggers glucagon secretion in the pancreas, increased adrenocorticotropic hormone (ACTH) secretion by the pituitary gland, and increased lipolysis by adipose tissue. Together, these effects lead to increased blood glucose and fatty acids, providing substrates for energy production within cells throughout the body.[11]
Medical uses

Adrenaline is used to treat a number of conditions including: cardiac arrest, anaphylaxis, and superficial bleeding.[12] It has been used historically for bronchospasm and hypoglycemia, but newer treatments for these, such as salbutamol, a synthetic epinephrine derivative, and dextrose, respectively, are currently preferred.[12]
Cardiac arrest
Adrenaline is used as a drug to treat cardiac arrest and other cardiac dysrhythmias resulting in diminished or absent cardiac output. Its actions are to increase peripheral resistance via α1receptor-dependent vasoconstriction and to increase cardiac output via its binding to β1 receptors.
Anaphylaxis
Due to its vasoconstrictive effects, adrenaline is the drug of choice for treating anaphylaxis. Allergy[13] patients undergoing immunotherapy may receive an adrenaline rinse before the allergen extract is administered, thus reducing the immune response to the administered allergen.
Because of various expressions of α1 or β2 receptors, depending on the patient, administration of adrenaline may raise or lower blood pressure, depending on whether or not the net increase or decrease in peripheral resistance can balance the positive inotropic and chronotropic effects of adrenaline on the heart, effects that increase the contractility and rate, respectively, of the heart.[citation needed]
The usual concentration for SQ or IM injection is 0.3 - 0.5 mg 1:1,000.
Asthma
Adrenaline is also used as a bronchodilator for asthma if specific β2 agonists are unavailable or ineffective.[14]
When given by the subcutaneous or intramuscular routes for asthma, an appropriate dose is 300-500mcg[15][16].
Croup
Racemic epinephrine has historically been used for the treatment of croup.[17][18] Racemic adrenaline is a 1:1 mixture of the dextrorotatory (d) and levorotatory (l) isomers of adrenaline.[19] The l- form is the active component.[19] Racemic adrenaline works by stimulation of the α-adrenergic receptors in the airway, with resultant mucosal vasoconstriction and decreased subglottic edema, and by stimulation of the β-adrenergic receptors, with resultant relaxation of the bronchial smooth muscle.[18]
In local anesthetics
Adrenaline is added to injectable forms of a number of local anesthetics, such as bupivacaine and lidocaine, as a vasoconstrictor to slow the absorption and, therefore, prolong the action of the anesthetic agent. Some of the adverse effects of local anesthetic use, such as apprehension, tachycardia, and tremor, may be caused by adrenaline. Epinephrine/adrenalin is frequently combined with dental and spinal anesthetics and can cause panic attacks in susceptible patients at a time when they may be unable to move or speak due to twilight drugs. [20]
Autoinjectors
Adrenaline is available in an autoinjector delivery system. EpiPens, Anapens, and Twinjects all use adrenaline as their active ingredient. Twinjects contain a second dose of adrenaline in a separate syringe and needle delivery system contained within the body of the autoinjector.
Though both EpiPen and Twinject are trademark names, common usage of the terms is drifting toward the generic context of any adrenaline autoinjector.[citation needed]
Adverse effects
Adverse reactions to adrenaline include palpitations, tachycardia, arrhythmia, anxiety, headache, tremor, hypertension, and acute pulmonary edema.[21]
Use is contraindicated in people on nonselective β-blockers, because severe hypertension and even cerebral hemorrhage may result.[10] Although commonly believed that administration of adrenaline may cause heart failure by constricting coronary arteries, this is not the case. Coronary arteries have only β2 receptors, which cause vasodilation in the presence of adrenaline.[22] Even so, administering high-dose adrenaline has not been definitively proven to improve survival or neurologic outcomes in adult victims of cardiac arrest.[23]
Measurement in biological fluids
Adrenaline may be quantified in blood, plasma, or serum as a diagnostic aid, to monitor therapeutic administration, or to identify the causative agent in a potential poisoning victim. Endogenous plasma adrenaline concentrations in resting adults are normally less than 10 ng/L, but may increase by 10-fold during exercise and by 50-fold or more during times of stress. Pheochromocytoma patients often have plasma adrenaline levels of 1000-10,000 ng/L. Parenteral administration of adrenaline to acute-care cardiac patients can produce plasma concentrations of 10,000 to 100,000 ng/L.[24][25]
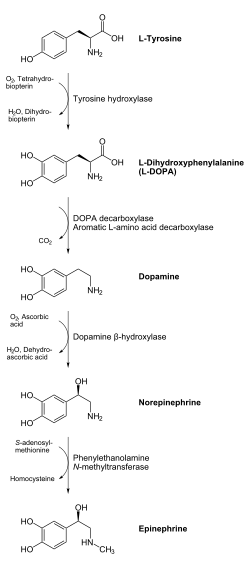
Biosynthesis and regulation
Adrenaline is synthesized in the medulla of the adrenal gland in an enzymatic pathway that converts the amino acid tyrosine into a series of intermediates and, ultimately, adrenaline. Tyrosine is first oxidized to L-DOPA, which is subsequently decarboxylated to give dopamine. Oxidation gives norepinephrine, which is methylated to give epinephrine.
Adrenaline is synthesized via methylation of the primary distal amine of noradrenaline by phenylethanolamine N-methyltransferase (PNMT) in the cytosol of adrenergic neurons and cells of the adrenal medulla (so-called chromaffin cells). PNMT is found in the cytosol of only cells of adrenal medullary cells. PNMT uses S-adenosylmethionine (SAMe) as a cofactor to donate the methyl group to noradrenaline, creating adrenaline.[citation needed]
For noradrenaline to be acted upon by PNMT in the cytosol, it must first be shipped out of granules of the chromaffin cells. This may occur via the catecholamine-H+ exchanger VMAT1. VMAT1 is also responsible for transporting newly synthesized adrenaline from the cytosol back into chromaffin granules in preparation for release.[citation needed]
In liver cells, adrenaline binds to the β-adrenergic receptor, which changes conformation and helps Gs, a G protein, exchange GDP to GTP. This trimeric G protein dissociates to Gs alpha and Gs beta/gamma subunits. Gs alpha binds to adenyl cyclase, thus converting ATP into cyclic AMP. Cyclic AMP binds to the regulatory subunit of protein kinase A: Protein kinase A phosphorylates phosphorylase kinase. Meanwhile, Gs beta/gamma binds to the calcium channel and allows calcium ions to enter the cytoplasm. Calcium ions bind to calmodulin proteins, a protein present in all eukaryotic cells, which then binds to phosphorylase kinase and finishes its activation. Phosphorylase kinase phosphorylates glycogen phosphorylase, which then phosphorylates glycogen and converts it to glucose-6-phosphate. [citation needed]
Regulation
The major physiologic triggers of adrenaline release center upon stresses, such as physical threat, excitement, noise, bright lights, and high ambient temperature. All of these stimuli are processed in the central nervous system.[26]
Adrenocorticotropic hormone (ACTH) and the sympathetic nervous system stimulate the synthesis of adrenaline precursors by enhancing the activity of tyrosine hydroxylase and dopamine-β-hydroxylase, two key enzymes involved in catecholamine synthesis.[citation needed] ACTH also stimulates the adrenal cortex to release cortisol, which increases the expression of PNMT in chromaffin cells, enhancing adrenaline synthesis. This is most often done in response to stress.[citation needed] The sympathetic nervous system, acting via splanchnic nerves to the adrenal medulla, stimulates the release of adrenaline. Acetylcholine released by preganglionic sympathetic fibers of these nerves acts on nicotinic acetylcholine receptors, causing cell depolarization and an influx of calcium through voltage-gated calcium channels. Calcium triggers the exocytosis of chromaffin granules and, thus, the release of adrenaline (and noradrenaline) into the bloodstream.[citation needed]
Adrenaline (as with noradrenaline) does exert negative feedback to down-regulate its own synthesis at the presynaptic alpha-2 adrenergic receptor.[citation needed] Abnormally elevated levels of adrenaline can occur in a variety of conditions, such as surreptitious epinephrine administration, pheochromocytoma, and other tumors of the sympathetic ganglia.
Its action is terminated with reuptake into nerve terminal endings, some minute dilution, and metabolism by monoamine oxidase and catechol-O-methyl transferase.
Chemical synthesis
Epinephrine may be synthesized by the reaction of catechol (1) with chloroacetyl chloride (2), followed by the reaction with methylamine to give the ketone (4), which is reduced to the desired hydroxy compound (5). The racemic mixture may be separated using tartaric acid.

For isolation from the adrenal glands tissue of livestock:
- J. Takamine, J. Soc. Chem. Ind., 20, 746 (1901).
- J. B. Aldrich, Am. J. Physiol., 5, 457 (1901).
Synthetic production:
- A. F. Stolz, Chem. Ber., 37, 4149 (1904).
- K. R. Payne, Ind. Chem. Chem. Manuf., 37, 523 (1961).
- H. Loewe, Arzneimittel-Forsch., 4, 583 (1954).
- Farbenwerke Meister Lucins & Bruning in Hochst a.M., DE 152814 (1903).
- Farbenwerke Meister Lucins & Bruning in Hochst a.M., DE 157300 (1903).
- Farbenwerke Meister Lucins & Bruning in Hochst a.M., DE 222451 (1908).
- Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1021/ja01186a024, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1021/ja01186a024instead. - D. Flacher, Z. Physiol. Chem., 58, 189 (1908).
Adrenaline junkie
Adrenaline junkie is a non-medical colloquial term used to describe somebody appearing to be addicted to endogenous epinephrine. The "high" is caused by self-inducing a fight-or-flight response by intentionally engaging in stressful or risky behavior, which causes a release of epinephrine by the adrenal gland. The term adrenaline junkie was popularly used in the 1991 movie Point Break to describe individuals enjoying dangerous activities (such as extreme sports, e.g. BASE jumping) for the adrenaline "rush". Adrenaline junkies appear to favor stressful activities for the release of epinephrine as a stress response. Whether or not the positive response is caused specifically by epinephrine is difficult to determine, as endorphins are also released during the fight-or-flight response to such activities.[27][28]
Notes
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6278965, please use {{cite journal}} with
|pmid=6278965instead. - ^ Cannon, W. B. (1929). American Journal of Physiology. 89: 84–107.
{{cite journal}}: Missing or empty|title=(help)[full citation needed] - ^ von Bohlen und Halbach, O; Dermietzel, R (2006). Neurotransmitters and neuromodulators: handbook of receptors and biological effects. Wiley-VCH. p. 125. ISBN 978-3-527-31307-5.
- ^ a b c Aronson, Jeffrey K (19). ""Where name and image meet"—the argument for "adrenaline"". British Medical Journal. 320 (2733): 506–509. doi:10.1136/bmj.320.7233.506. PMC 1127537. PMID 10678871.
{{cite journal}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|month=ignored (help) - ^ Changes to medicines names: BANs to rINNs, Medicines and Healthcare products Regulatory Agency
- ^ "Polish Thread in the History of Circulatory Physiology". Retrieved 2011-04-24.
- ^ Yamashima T (2003). "Jokichi Takamine (1854–1922), the samurai chemist, and his work on adrenalin". J Med Biogr. 11 (2): 95–102. PMID 12717538.
- ^ a b Bennett M (1999). "One hundred years of adrenaline: the discovery of autoreceptors". Clin Auton Res. 9 (3): 145–59. doi:10.1007/BF02281628. PMID 10454061.
- ^ Takamine J (1901). The isolation of the active principle of the suprarenal gland. Great Britain: Cambridge University Press. pp. xxix–xxx.
{{cite book}}:|work=ignored (help) - ^ a b Shen, Howard (2008). Illustrated Pharmacology Memory Cards: PharMnemonics. Minireview. p. 4. ISBN 1-59541-101-1.
- ^ a b Sabyasachi Sircar (2007). Medical Physiology. Thieme Publishing Group. p. 536. ISBN 3-13-144061-9.
- ^ a b "Epinephrine". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- ^ Sicherer, Scott H. (2006). Understanding and Managing Your Child's Food Allergy. Baltimore: The Johns Hopkins University Press. ISBN 0-8018-8491-8.
- ^ "Asthma Causes, Types, Symptoms, Treatment, Medication, Facts and the Link to Allergies by MedicineNet.com".
- ^ Soar, Perkins, et al (2010) European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. Oct. pp.1400-1433
- ^ Fisher, Brown, Cooke (Eds) (2006) Joint Royal Colleges Ambulance Liaison Committee. UK Ambulance Clinical Practice Guidelines.
- ^ Bjornson CL, Johnson DW (2008). "Croup". The Lancet. 371 (9609): 329–339. doi:10.1016/S0140-6736(08)60170-1. PMID 18295000.
- ^ a b Thomas LP, Friedland LR (1998). "The cost-effective use of nebulized racemic adrenaline in the treatment of croup". American Journal of Emergency Medicine. 16 (1): 87–89. doi:10.1016/S0735-6757(98)90073-0. PMID 9451322.
- ^ a b Malhotra A, Krilov LR (2001). "Viral Croup". Pediatrics in Review. 22 (1): 5–12. doi:10.1542/pir.22-1-5. PMID 11139641.
- ^ R. Rahn and B. Ball. Local Anesthesia in Dentistry, 3M ESPE AG, ESPE Platz, Seefeld, Germany, 2001, 44 pp.
- ^ About.com - "The Definition of Epinephrine"
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12147535, please use {{cite journal}} with
|pmid=12147535instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 1522840, please use {{cite journal}} with
|pmid=1522840instead. - ^ Raymondos, K.; Panning, B.; Leuwer, M.; Brechelt, G.; Korte, T.; Niehaus, M.; Tebbenjohanns, J.; Piepenbrock, S. (2000). "Absorption and hemodynamic effects of airway administration of adrenaline in patients with severe cardiac disease". Ann. Intern. Med. 132 (10): 800–803. PMID 10819703.
- ^ Baselt, R. (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 545–547. ISBN 0-9626523-7-7.
- ^ Nelson, L.; Cox, M. (2004). Lehninger Principles of Biochemstry (4th ed.). New York: Freeman. p. 908. ISBN 0-7167-4339-6.
- ^ What Is An Adrenaline Junkie? What Can You Do If You Are One? by Elizabeth Scott, M.S. (updated: November 1, 2007) About.com Health's Disease and Condition content is reviewed by the Medical Review Board.
- ^ Fight-or-flight reaction - Explanations - Brain -ChangingMinds.org.
References
- Boron WF, Boulpaep EL (2005). Medical Physiology: A Cellular And Molecular Approach. Philadelphia, PA: Elsevier/Saunders. ISBN 1-4160-2328-3. OCLC 56191776.
- Voet D, Voet J (2004). Biochemistry (3rd ed.). USA: Wiley. ISBN 0-471-19350-X. OCLC 154657578.
