Complement factor I
| CFI | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | CFI, AHUS3, ARMD13, C3BINA, C3b-INA, FI, IF, KAF, complement factor I | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 217030; MGI: 105937; HomoloGene: 171; GeneCards: CFI; OMA:CFI - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Complement factor I, also known as C3b/C4b inactivator, is a protein that in humans is encoded by the CFI gene. Complement factor I (factor I) is a protein of the complement system, first isolated in 1966 in guinea pig serum,[5] that regulates complement activation by cleaving cell-bound or fluid phase C3b and C4b.[6] It is a soluble glycoprotein that circulates in human blood at an average concentration of 35 μg/mL.[7]
Synthesis
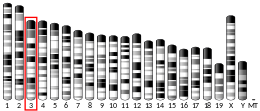
[edit]The gene for Factor I in humans is located on chromosome 4.[8] Factor I is synthesized mostly in the liver, but also in monocytes, fibroblasts, keratinocytes, and endothelial cells.[9][10][11] When synthesized, it is a 66kDa polypeptide chain with N-linked glycans at 6 positions.[12] Then, factor I is cleaved by furin to yield the mature factor I protein, which is a disulfide-linked dimer of heavy chain (residues 19-335, 51 kDalton) and light chain (residues 340-583, 37 kDalton).[13] Only the mature protein is active.
Structure
[edit]Factor I is a glycoprotein heterodimer consisting of a disulfide linked heavy chain and light chain.[14]
The factor I heavy chain has four domains: an FI membrane attack complex (FIMAC) domain, CD5 domain, and low density lipoprotein receptor 1 and 2 (LDLr1 and LDLr2) domains.[15] the heavy chain plays an inhibitory role in maintaining the enzyme inactive until it meets the complex formed by the substrate (either C3b or C4b) and a cofactor protein (Factor H, C4b-binding protein, complement receptor 1, and membrane cofactor protein).[16] Upon binding of the enzyme to the substrate:cofactor complex, the heavy:light chain interface is disrupted, and the enzyme activated by allostery.[16] The LDL-receptor domains contain one Calcium-binding site each.
The factor I light chain contains only the serine protease domain. This domain contains the catalytic triad His-362, Asp-411, and Ser-507, which is responsible for specific cleavage of C3b and C4b.[15] Conventional protease inhibitors do not completely inactivate Factor I[17] but they can do so if the enzyme is pre-incubated with its substrate: this supports the proposed rearrangement of the molecule upon binding to the substrate.
Both heavy and light chains bear Asn-linked glycans, on three distinct glycosylation sites each.
Crystal structure the crystal structure of human Factor I has been deposited as PDB: 2XRC.
Clinical significance
[edit]Dysregulated factor I activity has clinical implications. Loss of function mutations in the Complement Factor I gene lead to low levels of factor I which results in increased complement activity. Factor I deficiency in turn leads to low levels of complement component 3 (C3), factor B, factor H and properdin in blood, due to unregulated activation of C3 convertase, and to low levels of IgG, due to loss of iC3b and C3dg production. In addition to the following diseases, low factor I is associated with recurrent bacterial infections in children.
Age-related macular degeneration
[edit]Research suggests that mutations in the CFI gene contribute to development of age-related macular degeneration.[18] This contribution is thought to be due to the dysregulation of the alternative pathway, leading to increased inflammation in the eye.[19]
Atypical hemolytic uremic syndrome
[edit]Atypical hemolytic uremic syndrome is caused by complement overactivation.[20] Heterozygous mutations in the serine protease domain of the CFI gene account for 5-10% of cases.[20]
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000205403 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000058952 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Nelson RA, Jensen J, Gigli I, Tamura N (March 1966). "Methods for the separation, purification and measurement of nine components of hemolytic complement in guinea-pig serum". Immunochemistry. 3 (2): 111–35. doi:10.1016/0019-2791(66)90292-8. PMID 5960883.
- ^ Lachmann PJ, Müller-Eberhard HJ (April 1968). "The demonstration in human serum of "conglutinogen-activating factor" and its effect on the third component of complement". Journal of Immunology. 100 (4): 691–8. doi:10.4049/jimmunol.100.4.691. PMID 5645214.
- ^ Nilsson SC, Sim RB, Lea SM, Fremeaux-Bacchi V, Blom AM (August 2011). "Complement factor I in health and disease". Molecular Immunology (Submitted manuscript). 48 (14): 1611–20. doi:10.1016/j.molimm.2011.04.004. PMID 21529951. S2CID 37521895.
- ^ Goldberger G, Bruns GA, Rits M, Edge MD, Kwiatkowski DJ (July 1987). "Human complement factor I: analysis of cDNA-derived primary structure and assignment of its gene to chromosome 4". The Journal of Biological Chemistry. 262 (21): 10065–71. doi:10.1016/S0021-9258(18)61076-2. PMID 2956252.
- ^ Vyse TJ, Morley BJ, Bartok I, Theodoridis EL, Davies KA, Webster AD, Walport MJ (February 1996). "The molecular basis of hereditary complement factor I deficiency". The Journal of Clinical Investigation. 97 (4): 925–33. doi:10.1172/JCI118515. PMC 507137. PMID 8613545.
- ^ Julen N, Dauchel H, Lemercier C, Sim RB, Fontaine M, Ripoche J (January 1992). "In vitro biosynthesis of complement factor I by human endothelial cells". European Journal of Immunology. 22 (1): 213–7. doi:10.1002/eji.1830220131. PMID 1530917. S2CID 30130789.
- ^ Whaley K (March 1980). "Biosynthesis of the complement components and the regulatory proteins of the alternative complement pathway by human peripheral blood monocytes". The Journal of Experimental Medicine. 151 (3): 501–16. doi:10.1084/jem.151.3.501. PMC 2185797. PMID 6444659.
- ^ Tsiftsoglou SA, Arnold JN, Roversi P, Crispin MD, Radcliffe C, Lea SM, Dwek RA, Rudd PM, Sim RB (November 2006). "Human complement factor I glycosylation: structural and functional characterisation of the N-linked oligosaccharides". Biochimica et Biophysica Acta (BBA) - Proteins and Proteomics. 1764 (11): 1757–66. CiteSeerX 10.1.1.712.1764. doi:10.1016/j.bbapap.2006.09.007. PMID 17055788.
- ^ "FURIN furin, paired basic amino acid cleaving enzyme [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2018-03-30.
- ^ "CFI complement factor I [Homo sapiens (human)] - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2018-03-27.
- ^ a b Sanchez-Gallego JI, Groeneveld TW, Krentz S, Nilsson SC, Villoutreix BO, Blom AM (April 2012). "Analysis of binding sites on complement factor I using artificial N-linked glycosylation". The Journal of Biological Chemistry. 287 (17): 13572–83. doi:10.1074/jbc.M111.326298. PMC 3340171. PMID 22393059.
- ^ a b Roversi P, Johnson S, Caesar JJ, McLean F, Leath KJ, Tsiftsoglou SA, Morgan BP, Harris CL, Sim RB, Lea SM (August 2011). "Structural basis for complement factor I control and its disease-associated sequence polymorphisms". Proceedings of the National Academy of Sciences of the United States of America. 108 (31): 12839–44. Bibcode:2011PNAS..10812839R. doi:10.1073/pnas.1102167108. PMC 3150940. PMID 21768352.
- ^ Ekdahl KN, Nilsson UR, Nilsson B (June 1990). "Inhibition of factor I by diisopropylfluorophosphate. Evidence of conformational changes in factor I induced by C3b and additional studies on the specificity of factor I". Journal of Immunology. 144 (11): 4269–74. doi:10.4049/jimmunol.144.11.4269. PMID 2140392.
- ^ Wang Q, Zhao HS, Li L (2016-02-18). "Association between complement factor I gene polymorphisms and the risk of age-related macular degeneration: a Meta-analysis of literature". International Journal of Ophthalmology. 9 (2): 298–305. doi:10.18240/ijo.2016.02.23. PMC 4761747. PMID 26949655.
- ^ Tan PL, Garrett ME, Willer JR, Campochiaro PA, Campochiaro B, Zack DJ, Ashley-Koch AE, Katsanis N (March 2017). "Systematic Functional Testing of Rare Variants: Contributions of CFI to Age-Related Macular Degeneration". Investigative Ophthalmology & Visual Science. 58 (3): 1570–1576. doi:10.1167/iovs.16-20867. PMC 6022411. PMID 28282489.
- ^ a b Kavanagh D, Goodship TH, Richards A (November 2013). "Atypical hemolytic uremic syndrome". Seminars in Nephrology. 33 (6): 508–30. doi:10.1016/j.semnephrol.2013.08.003. PMC 3863953. PMID 24161037.
Further reading
[edit]- Bradley DT, Zipfel PF, Hughes AE (June 2011). "Complement in age-related macular degeneration: a focus on function". Eye. 25 (6): 683–93. doi:10.1038/eye.2011.37. PMC 3178140. PMID 21394116.
- Chan MR, Thomas CP, Torrealba JR, Djamali A, Fernandez LA, Nishimura CJ, Smith RJ, Samaniego MD (February 2009). "Recurrent atypical hemolytic uremic syndrome associated with factor I mutation in a living related renal transplant recipient". American Journal of Kidney Diseases. 53 (2): 321–6. doi:10.1053/j.ajkd.2008.06.027. PMC 2879708. PMID 18805611.
- Kalsi G, Kuo PH, Aliev F, Alexander J, McMichael O, Patterson DG, Walsh D, Zhao Z, Schuckit M, Nurnberger J, Edenberg H, Kramer J, Hesselbrock V, Tischfield JA, Vladimirov V, Prescott CA, Dick DM, Kendler KS, Riley BP (June 2010). "A systematic gene-based screen of chr4q22-q32 identifies association of a novel susceptibility gene, DKK2, with the quantitative trait of alcohol dependence symptom counts". Human Molecular Genetics. 19 (12): 2497–506. doi:10.1093/hmg/ddq112. PMC 2876884. PMID 20332099.
- Nilsson SC, Kalchishkova N, Trouw LA, Fremeaux-Bacchi V, Villoutreix BO, Blom AM (January 2010). "Mutations in complement factor I as found in atypical hemolytic uremic syndrome lead to either altered secretion or altered function of factor I". European Journal of Immunology. 40 (1): 172–85. doi:10.1002/eji.200939280. PMID 19877009.
- Rose JE, Behm FM, Drgon T, Johnson C, Uhl GR (2010). "Personalized smoking cessation: interactions between nicotine dose, dependence and quit-success genotype score". Molecular Medicine. 16 (7–8): 247–53. doi:10.2119/molmed.2009.00159. PMC 2896464. PMID 20379614.
- Sullivan M, Erlic Z, Hoffmann MM, Arbeiter K, Patzer L, Budde K, Hoppe B, Zeier M, Lhotta K, Rybicki LA, Bock A, Berisha G, Neumann HP (January 2010). "Epidemiological approach to identifying genetic predispositions for atypical hemolytic uremic syndrome" (PDF). Annals of Human Genetics. 74 (1): 17–26. doi:10.1111/j.1469-1809.2009.00554.x. PMID 20059470. S2CID 24304765.
- Westra D, Volokhina E, van der Heijden E, Vos A, Huigen M, Jansen J, van Kaauwen E, van der Velden T, van de Kar N, van den Heuvel L (July 2010). "Genetic disorders in complement (regulating) genes in patients with atypical haemolytic uraemic syndrome (aHUS)". Nephrology, Dialysis, Transplantation. 25 (7): 2195–202. doi:10.1093/ndt/gfq010. PMID 20106822.
- Bienaime F, Dragon-Durey MA, Regnier CH, Nilsson SC, Kwan WH, Blouin J, Jablonski M, Renault N, Rameix-Welti MA, Loirat C, Sautés-Fridman C, Villoutreix BO, Blom AM, Fremeaux-Bacchi V (February 2010). "Mutations in components of complement influence the outcome of Factor I-associated atypical hemolytic uremic syndrome". Kidney International. 77 (4): 339–49. doi:10.1038/ki.2009.472. PMID 20016463.
- Kondo N, Bessho H, Honda S, Negi A (June 2010). "Additional evidence to support the role of a common variant near the complement factor I gene in susceptibility to age-related macular degeneration". European Journal of Human Genetics. 18 (6): 634–5. doi:10.1038/ejhg.2009.243. PMC 2987347. PMID 20087399.
- Maga TK, Nishimura CJ, Weaver AE, Frees KL, Smith RJ (June 2010). "Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome". Human Mutation. 31 (6): E1445–60. doi:10.1002/humu.21256. PMID 20513133. S2CID 205919773.
- Reynolds R, Hartnett ME, Atkinson JP, Giclas PC, Rosner B, Seddon JM (December 2009). "Plasma complement components and activation fragments: associations with age-related macular degeneration genotypes and phenotypes". Investigative Ophthalmology & Visual Science. 50 (12): 5818–27. doi:10.1167/iovs.09-3928. PMC 2826794. PMID 19661236.
- Shin DH, Webb BM, Nakao M, Smith SL (July 2009). "Characterization of shark complement factor I gene(s): genomic analysis of a novel shark-specific sequence". Molecular Immunology. 46 (11–12): 2299–308. doi:10.1016/j.molimm.2009.04.002. PMC 2699631. PMID 19423168.
- Nilsson SC, Trouw LA, Renault N, Miteva MA, Genel F, Zelazko M, Marquart H, Muller K, Sjöholm AG, Truedsson L, Villoutreix BO, Blom AM (January 2009). "Genetic, molecular and functional analyses of complement factor I deficiency". European Journal of Immunology. 39 (1): 310–23. doi:10.1002/eji.200838702. PMID 19065647. S2CID 8445601.
- Fagerness JA, Maller JB, Neale BM, Reynolds RC, Daly MJ, Seddon JM (January 2009). "Variation near complement factor I is associated with risk of advanced AMD". European Journal of Human Genetics. 17 (1): 100–4. doi:10.1038/ejhg.2008.140. PMC 2985963. PMID 18685559.
- Yuasa I, Irizawa Y, Nishimukai H, Fukumori Y, Umetsu K, Nakayashiki N, Saitou N, Henke L, Henke J (January 2011). "A hypervariable STR polymorphism in the complement factor I (CFI) gene: Asian-specific alleles". International Journal of Legal Medicine. 125 (1): 121–5. doi:10.1007/s00414-009-0369-0. PMID 19693526. S2CID 37565572.
- Moore I, Strain L, Pappworth I, Kavanagh D, Barlow PN, Herbert AP, Schmidt CQ, Staniforth SJ, Holmes LV, Ward R, Morgan L, Goodship TH, Marchbank KJ (January 2010). "Association of factor H autoantibodies with deletions of CFHR1, CFHR3, CFHR4, and with mutations in CFH, CFI, CD46, and C3 in patients with atypical hemolytic uremic syndrome". Blood. 115 (2): 379–87. doi:10.1182/blood-2009-05-221549. PMC 2829859. PMID 19861685.
- Li MZ, Yu DM, Yu P, Liu DM, Wang K, Tang XZ (April 2008). "Mitochondrial gene mutations and type 2 diabetes in Chinese families". Chinese Medical Journal. 121 (8): 682–6. doi:10.1097/00029330-200804020-00004. PMID 18701018.
- Nilsson SC, Nita I, Månsson L, Groeneveld TW, Trouw LA, Villoutreix BO, Blom AM (February 2010). "Analysis of binding sites on complement factor I that are required for its activity". The Journal of Biological Chemistry. 285 (9): 6235–45. doi:10.1074/jbc.M109.097212. PMC 2825419. PMID 20044478.
External links
[edit]- GeneReviews/NCBI/NIH/UW entry on Atypical Hemolytic-Uremic Syndrome
- OMIM entries on Atypical Hemolytic-Uremic Syndrome
- The MEROPS online database for peptidases and their inhibitors: S01.199[permanent dead link]