Ventricular septal defect: Difference between revisions
| Line 38: | Line 38: | ||
CAUSES: The cause of VSD ( ventricular septal defect) includes the incomplete looping of the heart during days 24-28 of development. Faults with NKX2.5 gene can cause this. |
CAUSES: The cause of VSD ( ventricular septal defect) includes the incomplete looping of the heart during days 24-28 of development. Faults with NKX2.5 gene can cause this. |
||
For more information visit::: http://www.ahqa.webs.com/ --- please note we are NOT doctors and CANNOT answer questions to specific medical issues |
|||
==Treatment== |
==Treatment== |
||
Revision as of 11:36, 25 May 2010
| Ventricular septal defect | |
|---|---|
| Specialty | Medical genetics |
| Frequency | 0.0272% (Europe) |
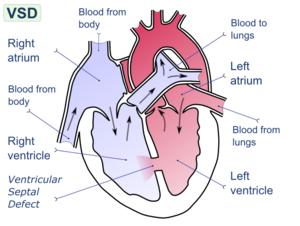
A ventricular septal defect (VSD) is a defect in the ventricular septum, the wall dividing the left and right ventricles of the heart.
The ventricular septum consists of an inferior muscular and superior membranous portion and is extensively innervated with conducting cardiomyocytes. The membranous portion, which is close to the atrioventricular node, is most commonly affected in adults and older children.[1][2]
Congenital VSDs are collectively the most common congenital heart defects.[3]
Diagnosis
A VSD can be detected by cardiac auscultation. Classically, a VSD causes a pathognomonic holo- or pansystolic murmur. Auscultation is generally considered sufficient for detecting a significant VSD. The murmur depends on the abnormal flow of blood from the left ventricle, through the VSD, to the right ventricle. If there is not much difference in pressure between the left and right ventricles, then the flow of blood through the VSD will not be very great and the VSD may be silent. This situation occurs a) in the fetus (when the right and left ventricular pressures are essentially equal), b) for a short time after birth (before the right ventricular pressure has decreased), and c) as a late complication of unrepaired VSD. Confirmation of cardiac auscultation can be obtained by non-invasive cardiac ultrasound (echocardiography). To more accurately measure ventricular pressures, cardiac catheterization, can be performed.
Pathophysiology
During ventricular contraction, or systole, some of the blood from the left ventricle leaks into the right ventricle, passes through the lungs and reenters the left ventricle via the pulmonary veins and left atrium. This has two net effects. First, the circuitous refluxing of blood causes volume overload on the left ventricle. Second, because the left ventricle normally has a much higher systolic pressure (~120 mm Hg) than the right ventricle (~20 mm Hg), the leakage of blood into the right ventricle therefore elevates right ventricular pressure and volume, causing pulmonary hypertension with its associated symptoms. This effect is more noticeable in patients with larger defects, who may present with breathlessness, poor feeding and failure to thrive in infancy. Patients with smaller defects may be asymptomatic.
Signs and symptoms
Ventricular septal defect is usually symptomless at birth. It usually manifests a few weeks after birth.
Symptoms
VSD is an acyanotic congenital heart defect, aka a Left-to-right shunt, so there are no signs of cyanosis.
Signs
- Pansystolic (Holosystolic) murmur (depending upon the size of the defect)
CAUSES: The cause of VSD ( ventricular septal defect) includes the incomplete looping of the heart during days 24-28 of development. Faults with NKX2.5 gene can cause this.
For more information visit::: http://www.ahqa.webs.com/ --- please note we are NOT doctors and CANNOT answer questions to specific medical issues
Treatment

Treatment is either conservative or surgical. Smaller congenital VSDs often close on their own, as the heart grows, and in such cases may be treated conservatively. In cases necessitating surgical intervention, a heart-lung machine is required and a median sternotomy is performed. Percutaneous endovascular procedures are less invasive and can be done on a beating heart, but are only suitable for certain patients. Repair of most VSDs is complicated by the fact that the conducting system of the heart is in the immediate vicinity.
Ventricular septum defect in infants is initially treated medically with cardiac glycosides (e.g., digoxin 10-20mcg/kg per day), loop diuretics (e.g., furosemide 1–3 mg/kg per day) and ACE inhibitors (e.g., captopril 0.5–2 mg/kg per day).
Epidemiology and Etiology
VSDs are the most common congenital cardiac anomalies. They are found in 30-60% of all newborns with a congenital heart defect, or about 2-6 per 10000 births. During heart formation, when the heart begins life as a hollow tube, it begins to partition, forming a septa. If this does not occur properly it can lead to an opening being left within the ventricular septum. It is debatable whether all those defects are true heart defects, or if some of them are normal phenomena, since most of the trabecular VSDs close spontaneously.[4] Prospective studies give a prevalence of 2-5 per 100 births of trabecular VSDs that closes shortly after birth in 80-90% of the cases.[5][6].
Congenital VSDs are frequently associated with other congenital conditions, such as Down syndrome.[7]
A VSD can also form a few days after a myocardial infarction[8] (heart attack) due to mechanical tearing of the septal wall, before scar tissue forms, when macrophages start remodeling the dead heart tissue.
See also
- Atrial septal defect
- Atrioventricular septal defect
- Cardiac output
- Congenital heart disease
- Heart sounds
- Pulmonary hypertension
Additional images
-
Heart anatomic view of right ventricle and right atrium with example ventricular septal defects
References
- ^ Ambumani P, Kuruchi Srinivasan. Ventricular Septal Defect, General Concepts. eMedicine.com. URL: http://www.emedicine.com/ped/topic2402.htm. Accessed on December 5, 2005.
- ^ Eidem BW. Ventricular Septal Defect, Muscular. eMedicine.com. URL: http://www.emedicine.com/ped/topic2543.htm. Accessed on April 13, 2006.
- ^ Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002 Jun 19;39(12):1890-900. PMID 12084585.
- ^ Meberg A, et al.: Increasing incidence of ventricular septal defects caused by improved detection rate. Acta Pædiatrica 1994; 83: 653-657.
- ^ Hiraishi S, Agata Y, Nowatari M, Oguchi K, et al. Incidence and natural course of trabecular ventricular septal defect: Two-dimensional echocardiography and color Doppler flow image study. J Pediatr 1992;120:409-15.
- ^ Roguin N, Du ZD, Barak M, Nasser N, Hershkowitz S, Milgram E. High prevalence of muscular ventricular septal defect in neonates. J Am Coll Cardiol 1995 November 15;26(6):1545-8
- ^ Wells GL, Barker SE, Finley SC, Colvin EV, Finley WH. Congenital heart disease in infants with Down's syndrome. South Med J. 1994 Jul;87(7):724-7. PMID 8023205.
- ^ Bruckheimer E. Ventricular septal defect. Medical Encyclopedia - MedlinePlus.org, URL: http://www.nlm.nih.gov/medlineplus/ency/article/001099.htm. Accessed on December 5, 2005.
External links
- Ventricular septal defect - Children's Hospital Boston
- Pediatric Heart Surgery
- Ventricular septal defect - American Heart Association
- Ventricular septal defect - medlineplus.org
- Ventricular Septal Defect information from Seattle Children's Hospital Heart Center
- Animation of ventricular septal defect from AboutKidsHealth.ca
- Perimembranous VSD - emedicine.com
- Supracristal VSD - emedicine.com
- Down's Heart Group Easy to understand diagram and explanation of VSD.
- C.S. Mott Children's Hospital, Congenital Heart Center: Ventricular Septal Defect at umich.edu
- Ventricular Septal Defect Cove Point Foundation

