User:DocElisa/Lower limbs venous ultrasonography
| DocElisa/Lower limbs venous ultrasonography | |
|---|---|
 Ultrasonography equipment | |
| ICD-10-PCS | B53 |
| ICD-9-CM | 88.77 |
Ultrasonography of leg veins is a non-invasive procedure that gives information about the anatomy, physiology and pathology of both the superficial and the deep venous systems.[1]
As with heart ultrasound studies, venous ultrasonography requires an understanding of hemodynamics, in order to give useful examination reports, of quality.[2] Specialized training in venous ultrasonography is not undertaken in some countries, which undermines best practice.[3]
Since lower limbs venous ultrasonography does not involve the use of ionizing radiation, the procedure is harmless and can be safely used on anybody, of any age. Preparation by the individual is not normally required. Sometimes though a complementary study of the abdominal veins is requested, in which case, the person is asked to fast for 12 hours beforehand. The sensitivity and specificity measurements are approximately 90%. Although the equipment itself is very expensive, the actual examinations are not. This technique is the first choice to confirm venous pathology diagnoses.[4][5]
In chronic venous insufficiency, this examination is of most benefit in confirming varicose disease, allowing a proper assessment of the hemodynamics, and in enabling the charting of disease progression and response to treatment. The detection of competent perforator veins may be as important as the detection of incompetent ones. Mapping[nb 1] of the venous system is essential in the understanding of the condition in any individual. This map enables vascular surgeons to plan interventions, in a stage known as virtual dissection.[nb 2][6]
Equipment
[edit]
The ultrasound equipment must be of sufficiently high quality in order to give a correct image treatment which can then provide invaluable information, mainly at the superficial level. It must be able to deliver both doppler and color. The choice of a probe will depend on the depth needed to be studied. For example, the superficial venous system (SVS) can be very well examined using a high frequency probe of 12 MHz. For patients who have thick adipose tissue a probe of 7.5 MHz will be required. Deep veins require probes of around 6 MHz whilst the abdominal vessels are better studied with probes of between 4 and 6 MHz.[7] In summary, three probes are needed together with a top level scanner which makes it a very expensive piece of equipment. Also, the proper use of the scanner calls for a high level of expertise, so that the examiner must be well qualified and experienced in order to give effective results. In contrast to arterial ultrasonography the wall of the vein is not relevant and importance is given to the hemodynamic conclusions that the examiner can obtain in order to provide a valuable report. It follows that the examiner knowledge of venous hemodynamics is crucial, which is a real barrier to a radiologist untrained in this field, who might wish to carry out these examinations.[8][9]
Indications
[edit]The purpose of this examination is focused mainly on the study of two different pathologies; venous insufficiency, and venous thrombosis.[10][11] It allows the examiner to evaluate properly:
- Superficial and deep venous network anatomy, mainly topographic anatomy.
- Blood flow direction - extremely important in vein pathology.
- The presence of a retrograde blood flow (the inverse of the physiological direction, also called anterograde blood flow).[nb 3]
- The existence of a reflux situation.[12][13][nb 4]
Where venous thrombosis is suspected, this examination gives the diagnosis and evaluates the extension and the degree of severity.[14][15]
There are no contraindications for this examination.
Mechanism
[edit]
Ultrasonography is based on the knowledge that sound can pass through human body tissues and can reflect itself on the tissue interfaces[nb 5] in the same way that light can reflect back on itself, from a mirror. Tissue in the body will offer varying degrees of resistance, known as acoustic impedance, to the path of the ultrasound beam. So that, any tissue will still reflect the ultrasound beam to some degree. When there is a high impedance difference between two tissues, the interface between them will strongly reflect the sound. When the ultrasound beam meets air, or solid tissue such as bone, their impedance difference is so great that most of the acoustic energy is reflected making it impossible to see any underlying structures. The examiner will see just a shadow, instead of the image, he or she might have expected. Air will impede sound waves which is why a gel is used. The gel prevents air bubbles from forming between the transducer, or probe, and the patient's skin and so helps the conduction of the sound waves from the transducer into the body. The watery medium also helps to conduct the sound waves. Liquids, including blood have a low impedance, which means that little energy will be reflected and no visualization possible. One of the important exceptions is that when the blood flow is very slow it can in fact be seen, and this is termed "spontaneous contrast".[16][17]
The probe is an ultrasonic sensor also called a transceiver, but more generally known as a transducer, which functions to send and receive acoustic energy. The emission is generated on piezoelectric crystals by the piezoelectric effect. The reflected ultrasound is received by the probe, transformed into an electric impulse as voltage and sent to the engine for signal processing and conversion to an image on the screen. The depth reached by the ultrasound beam is dependent on the frequency of the probe used. The higher the frequency the lesser the depth reached.[18]
Preparation
[edit]No preparation is normally necessary for this examination, but if a complementary study of abdominal veins is also required, the patient will be asked to fast for 12 hours beforehand. The sensitivity and specificity measurements are around 90%.[5]
Procedure
[edit]Where either superficial or deep thrombosis is suspected, this examination can be performed with the patient lying down. For an evaluation of varicose veins, the patient will need to be in an upright position to enable a proper study of blood flow direction[19]
Deep vein thrombosis
[edit]
Unlike the arterial ultrasound study, the venous ultrasonography is carried out with the probe in a transversal position, (perpendicular to the vein great axis).[20] Vessels will appear on the screen as round, and black inside. All collateral veins are better detected this way, including perforator veins, but of most importance is the detection of venous thrombosis. The most reliable sign of thrombosis (even when a good image and color is present) is the absence of compressibility.[nb 6][21] However, if the probe is parallel to the vein axis, when the examiner compresses it, the probe can slide to the right or to the left giving a false negative for thrombosis as the probe has moved away and the vein will not then be evident. Nevertheless when the examiner needs to show the head thrombus in a printout he will present the probe parallel to the vein great axis.[20]
The inability to compress the vein is one of the more reliable indications of venous thrombosis, since a very recently formed thrombus being not very solid, will have a low echogenicity, and will be seen as a black area in the gray-scale image and will be hardly visible. When the examiner uses color, the imaging is not much improved.[22] The fact that the examiner doesn't see a thrombus doesn't mean that it doesn't exist and a vein lumen with echoes doesn't mean that a thrombus does exist. The location of the thrombus and its detail will inform of the seriousness of the condition. In a deep vein thrombosis (DVT), or in a superficial thrombosis where the thrombus is floating, especially if it is located near to the sapheno-femoral junction will indicate an emergency situation since their will be a high risk of a pulmonary embolism occurring. [4][23]
There is a simplified technique called "compression ultrasonography" which can be used for quick deep vein thrombosis diagnosis, limited though to the common femoral vein and the popliteal vein. It is invaluable in an emergency situation and is performed just by vein compression using transducer pressure.[24]
Compression ultrasonography has both high sensitivity and specificity for detecting proximal deep vein thrombosis, but only in symptomatic patients. Results are not reliable when the patient is symptomless and must be checked carefully. For example, in high risk post-operative patients, mainly after orthopedic surgery where there is already lower limb pain and edema following surgery, thrombi can be localized in the calf veins and are often not completely occlusive.[25][26][27]
Venous insufficiency
[edit]The request procedure, asking for an investigation into the hemodynamic changes in a patient with chronic venous disease, is quite different from an examination request made for suspected deep vein thrombosis. The request for this investigation needs to be made by a physician who has firstly undertaken a clinical examination and can provide valid reasons for the investigation. He or she also needs to give guidance as to what to look for and, if the patient's physician is a surgeon, how he or she intends to treat the patient. For example, an investigation performed with the intention of treating the patient by vein stripping or laser therapy is very different from the examination performed with the intention of executing a CHIVA. [nb 7]
Unlike the arterial ultrasound study, when the sonographer studies venous insufficiency, the vein wall itself has no relevance and attention will be focused on the direction of blood flow. The objective of the examination is to see how the veins drain. In this way, venous ultrasonography has at times become a hemodynamic examination which is reserved for experienced sonographers who have completed hemodynamic studies and training and have acquired a deep knowledge of this subject.[8]
Also, unlike the arterial ultrasound examination, blood velocity in veins has no diagnostic meaning. Veins are a draining system similar to a low pressure hydraulic system, with a laminar flow and a low velocity. This low velocity is responsible for the fact that we can only detect it spontaneously with the doppler effect on the proximal and larger veins (femoral and iliac veins). Here the flow is either modulated by the respiratory rhythm or is continuous in cases where the flow is high. The thinner veins do not have a spontaneous flow. However, in some circumstances the blood flow is so slow that we can see some echogenic material moving within the vein, in "spontaneous contrast".[nb 8] This material can easily be mistaken for a thrombus, but can also easily be discounted by testing the vein's compressibility.[28]

To evidence the blood flow velocity there are some techniques that the examiner can use to accelerate blood flow and show valvular function:
Manual squeezing and releasing - the examiner can compress the vein below the probe which will push the blood in its normal anterograde direction. On releasing the pressure if the valves are insufficient the flow will appear as a retrograde flow or reflux, greater than 0.5 sec.[12]
Valsalva maneuver - when the patient performs this maneuver, he increases intra-abdominal venous pressure. If the great saphenous valve at the sapheno-femoral junction is insufficient, a reflux will appear.
Paraná maneuver,[nb 9] uses a proprioceptive reflex to test venous muscle pump induced flow. A slight push to the waist, triggers a muscle contraction in the leg, in order to maintain posture. This maneuver is very useful to study deep vein flow and to detect valvular insufficiency, mainly at the popliteal level, and is used when there are painful or very edematous legs. [29]
Toe flexion, active foot dorsi-flexion, and hyper-extension on tip toes, can all be very useful to detect perforator vein insufficiency. These maneuvers unleash a muscle contraction which compresses deep veins. If a perforator valve is insufficient then a reflux flow from the deep to the superficial through the perforator vein will be registered.[30]
All of these trained techniques need time to be mastered properly.
Normal blood flow is anterograde (going to the heart), and from superficial to deep veins via perforator veins. However there are two exceptions: firstly, the great saphenous vein (GSV) collaterals which drain the abdominal wall have a flow from top to bottom so that when an examiner tests the sapheno-femoral junction, a false positive diagnosis might be made; secondly, in the flow from the sole of the foot venous network around 10% drains to the dorsal venous arch of the foot, going therefore from deep to superficial veins.[31]
Attention will be focused on the direction of the blood flow in deep veins and in the superficial veins the GSV, and the small saphenous vein (SSV), their collaterals, mainly the anterior accessory saphenous vein, the Giacomini vein, and the perforator veins, as well as being focused on shunt detection.[nb 10][32]
As a further complication to the examination, where venous insufficiency is evidenced, the examination needs to be done with the probe in the transversal position but the mapping must be done showing the veins in their longitudinal aspect. This demands a rapid extrapolation by the physician from the transversal images seen to the longitudinal drawing needed.[33][6]
 |
 |
 |
 |
Technical pitfalls
[edit]Out of all of the medical complementary examinations, lower limbs venous ultrasonography is the one where the examiner's expertise and training are all important in deciding the quality of the results .[34][35] The actual execution of the examination is demanding and the interpretation of the results themselves is subjective and proportional to the examiner's knowledge in venous hemodynamics. (A mapping does help the reproducibility and the inter-observer agreement of this examination).[6]}[36] The examination is made even more difficult because there can be dilated veins without insufficiency, (by hyper-debit), and non dilated but insufficient veins. Moreover, veins can have a discrete insufficiency in summer but then can be normal in winter. Also, by definition of insufficiency, blood may be seen to flow freely in both directions, anterograde and retrograde between two valves.[37] Another problem presents itself when dealing with the superficial venous system, and that is the fact that venous anatomy is not constant, there are numerous variations such as veins being where they are found, not where they are looked for, and in the same patient the right lower limb is not identical to the left lower limb. The execution protocol is completely different from the arterial examination and all the dynamic maneuvers need to be very well executed which can be a problem for less experienced examiners. The need of a specialized training is mandatory which is a huge problem for many countries today.[38]
Particular details
[edit]Great saphenous vein
[edit]
The great saphenous vein,(GSV) a superficial vein, has its origin in the dorsal venous arch of the foot, a superficial vein which connects the small saphenous vein with the GSV. It travels up the leg and medial side of the thigh to reach the groin, where it drains in the common femoral vein. It is located between the superficial and the deep fascia, called the saphenous compartment.[39] Along the length of the GSV, it receives numerous collaterals and drains into the deep veins via the perforator veins. When visualized in an ultrasonography examination, this compartment with the GSV inside it, resembles an eye and so it is called the "eye image". [40] Both the Giacomini vein and the anterior accessory saphenous vein (AASV) also present this "eye image", with the AASV only at its proximal third. All veins which are between the skin and the superficial fascia are tributaries and all veins which cross the deep fascia to join the deep venous system are perforator veins.[11]
Three anatomic compartments can be described:
- The deep compartment or N1 (N=Network), containing the deep veins
- The saphenous compartment or N2, between the two fascia, containing the saphenous, the AAS and the Giacomini veins
- The superficial or N3, containing numerous tributary veins; of these one is usually seen at the medial leg, the Leonardo's vein or posterior arch vein and very often is the cause of varicose problems.
Some authors describe one more compartment N4, containing collaterals which form a bypass between two distinct points of the same vein.[41]

The compartment differentiation is very useful in ultrasonographic examination because it enables an easier systematization, the mapping execution and, if appropriate, the surgery strategic.
Being protected between two fascias, veins belonging to compartment N2 very rarely become sinuous. So, when doing the patient physical examination the clinician who detects a sinuous vein knows immediately (with a very low possibility of error) that it's not the saphenous vein but a tributary.
The sapheno-femoral junction will be tested by Valsalva maneuver and the use of color and doppler is very useful at this level.[41]
Anterior accessory saphenous vein
[edit]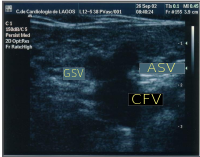
The anterior accessory saphenous vein is an important GSV collateral frequently responsible for varicose veins located on the anterior and lateral aspect of the thigh. It has a more anterior position compared with saphenous vein and is outside the femoral vessels plan. It is the "alignment sign".[11] At the groin it can be seen at the outside of great saphenous vein creating, together with the GSV and the femoral vein, an image, the so-called "Mickey mouse sign". Some authors, inspired on this sign (presented for the first time at CHIVA's meeting 2002 at Berlin), describe a "Mickey mouse view" at the groin, image formed by the common femoral vein, GSV and superficial femoral artery. When insufficient, its flow becomes retrograde and tries to drain in the superior fibular perforator, at the lateral aspect of the knee or sometimes it runs down until the ankle trying to drain in the inferior fibular perforator.[41]
Small saphenous vein
[edit]The Small saphenous vein, runs along the posterior aspect of the leg until the popliteal region where usually it drains in the popliteal vein. Ultrasonography has permitted to show a great number of variations at this level. Is not rare to see it joining the gastrocnemius vein before draining in the popliteal vein. Sometimes it doesn't contact with the popliteal vein but go up to drain in the great saphenous vein at a variable level, or, instead draining in the popliteal vein it can merge with Giacomini vein and drain in the GSV at the superior 1/3 of the thigh. Usually it connects with a perforator vein at its middle 1/3.[20] Rarely it can drain in a thigh muscle vein (semimembranosus in the images below). To check its insufficiency, Paraná maneuver is very useful.[29]
Giacomini vein
[edit]Giacomini vein acts most of the time as a bypass between GSV and SSV territories. Usually its flow is in anterograde direction, from bottom to top. However it can be retrograde without pathology. After a GSV stripping, laser ablation or after its ligation at the sapheno-femoral junction, Giacomini vein will drain into the SSV, with a retrograde flow. When there is GSV thrombosis or insufficiency, Giacomini can deviate blood flow to SSV and from this one to the popliteal vein. Each time the examiner must refer what is the flow direction in this vein, as it has important implications to decide how to treat the patient if the surgeon pretend to do a treatment other than a stripping or laser ablation.[42]
Perforator veins
[edit]
Perforator veins are a very special part of venous system, carrying blood from superficial to deep veins. During the muscular systole their valves close and don't permit the blood flow coming from the deep to the superficial veins. When their valves become insufficient they are responsible for the fast worsening of a previous varicose disease and the development of venous ulcers. Detection of insufficient perforators is important because they need to be ligatured. However, the detection of competent ones is also very important because they are used strategically in new techniques of conservative surgery. When the venous ultrasonography is made, insufficient and continent perforators must be present on venous mapping.[43] To test properly these veins the examiner needs to use some maneuvers like the Paraná maneuver, toe flexion, active foot dorsi-flexion and hyper-extension of tip toes.
Examination report
[edit]
After performing this examination, the physician needs to write a report in which some points are crucial:
How is the DVS, its permeability, compressibility, continent or insufficient;
Permeability, compressibility of the SVS, presence or absence superficial insufficiency, in which veins or vein segments ;
Which perforator veins are continent or insufficient;
Presence or absence of shunts;
Mapping the insufficient veins, flux direction, shunts, perforators.[6]
History
[edit]After the introduction of ultrasound in 1956, it was very quickly adopted for use in medicine due to its rapid, accurate diagnostic capabilities which offered the possibility of prompt treatment. A few years later, acoustic Doppler velocimetry and the color doppler were devised, which have had a significant impact on many specialties, including radiology, obstetrics, gynecology, angiology and cardiology. Their use requires appropriate training in order to prevent false positive or false negative diagnoses. [44][4]
Doppler effect has been described for the first time by Christian Doppler in 1843. Around forty years after the piezoelectric effect was discovered and confirmed in 1880 by Pierre & Jacques Curie, but only in the late 1940s it has been applied to the human body for medical purposes by Dr. George Ludwig, University of Pennsylvania.[45][46]
In France, 1963, Pourcelot L. begins his these, which is presented in 1964, and used pulsed doppler for blood flow calculation [47] followed by Peronneau in 1969. Dr. Gene Strandness and the bio-engineering group at the University of Washington who conducted research on Doppler ultrasound as a diagnostic tool for vascular disease, published their first work in 1967, the first medical application of ultrasound.[48] [49] The first report published about the venous system appeared around 1967-1968.[50]
Since 1970, real-time scanners and pulsed doppler, have permitted its use to study the venous system function. The first demonstration of color Doppler was achieved by Geoff Stevenson.[51][52]
Rapid technical advancements in echotomography and the possibility to see properly the superficial tissues made possible the very good specificity and sensitivity of this technique.[53] Great attention to hemodynamic study begins mainly with Franceschi, C., in France, when he described for the first time the conservative treatment for venous insufficiency in 1985.[54]
Footnotes
[edit]- ^ Mapping is a schematic depiction of the venous anatomic-functional configuration in an individual
- ^ Virtual dissection is a schema based on veinous mapping where the surgeon projects what he will do to treat his patient. Drawn on paper, after the ultrasound examination, it will be drawn over the patient's skin before surgery.
- ^ The anterograde blood flow or physiological blood flow in veins is from periphery to the heart
- ^ Reflux means the presence of a bi-directional flow. An isolated retrograde flow is not a reflux, but it only becomes a reflux in presence of a previously anterograde flow
- ^ Interface is the plane between two tissues with a different density, for instance skin-fat-aponevrosis-muscle
- ^ A vein cannot be compressed when the blood is in a solid state, as with a thrombus, in the same way that a rubber pipe cannot be compressed if the water inside is frozen
- ^ CHIVA means "Venous Insufficiency Conservative, Hemodynamic and Ambulatory treatment" the order of words coming from French because is a procedure invented by the French researcher Claude Franceschi
- ^ Echogenic is the tissue which reflects the ultrasound beam and can be visualized on the screen
- ^ Paraná maneuver has been described for the first time by Claude Franceschi at the Chiva congress 1998 at Paraná Town, Argentina
- ^ In venous circulation, shunt is the situation where blood circulates from one vein (leak point) to another and from this one to the former (re-entry point) creating a pathway in a vicious circle between two veins one with a physiologic flow and the other with a retrograde flow
Bibliography
[edit]- Belem, Luciano Herman Juaçaba; Nogueira, Antonio Carlos Santos; Schettino, Claudio Domenico; Barros, Marcio Vinicius Lins; de Alcantara, Monica Luiza; Studart, Paulo Cesar de Carvalho; de Araújo, Paula Pimentel; do Amaral, Salomon Israel; Barretto, Simone (2004). "Normatização dos equipamentos e das técnicas para a realização de exames de ultra-sonografia vascular" [Standardization of equipment and techniques for performing vascular ultrasound examinations]. Arquivos Brasileiros de Cardiologia. 82: 1–14. doi:10.1590/S0066-782X2004001200001. PMID 15264051.
- Caggiati, A.; Ricci, S. (Dec 1997). "The long saphenous vein compartment". Phlebology. 12 (3): 107–11. doi:10.1177/026835559701200307. S2CID 70465177.
{{cite journal}}: CS1 maint: date and year (link)
- Cavezzi, A.; Labropoulos, N.; Partsch, H.; Ricci, S.; Caggiati, A.; Myers, K.; Nicolaides, A.; Smith, P.C. (2006). "Duplex Ultrasound Investigation of the Veins in Chronic Venous Disease of the Lower Limbs—UIP Consensus Document. Part II. Anatomy". European Journal of Vascular and Endovascular Surgery. 31 (3): 288–99. doi:10.1016/j.ejvs.2005.07.020. PMID 16230038.
- Cina, Alessandro; Pedicelli, Alessandro; Di Stasi, Carmine; Porcelli, Alessandra; Fiorentino, Alessandro; Cina, Gregorio; Rulli, Francesco; Bonomo, Lorenzo (2005). "Color-Doppler sonography in chronic venous insufficiency: What the radiologist should know". Current Problems in Diagnostic Radiology. 34 (2): 51–62. doi:10.1067/j.cpradiol.2004.12.001. PMID 15753879.
- Cobbold, Richard SC (2007). Foundations of Biomedical Ultrasound. New York: Oxford University Press. pp. 422–3. ISBN 978-0-19-516831-0. Retrieved February 5, 2013.
- Coleridge-Smith, P.; Labropoulos, N.; Partsch, H.; Myers, K.; Nicolaides, A.; Cavezzi, A. (2006). "Duplex Ultrasound Investigation of the Veins in Chronic Venous Disease of the Lower Limbs—UIP Consensus Document. Part I. Basic Principles". European Journal of Vascular and Endovascular Surgery. 31 (1): 83–92. doi:10.1016/j.ejvs.2005.07.019. PMID 16226898.
- Dauzat, Michel (1991). Ultrasonographie vasculaire diagnostique: Théorie et pratique [Vascular diagnostic ultrasound: Theory and practice] (in French). Paris: Vigot. pp. 386–437. ISBN 978-2-7114-1104-7.
- Elias, Antoine; Mallard, Luc; Elias, Marie; Alquier, Catherine; Guidolin, François; Gauthier, Bruno; Viard, Alain; Mahouin, Pierre; Vinel, Anne (2011). "A single complete ultrasound investigation of the venous network for the diagnostic management of patients with a clinically suspected first episode of deep venous thrombosis of the lower limbs". Thrombosis and Haemostasis. 89 (2): 221–7. doi:10.1267/THRO03020221 (inactive 2022-06-26). PMID 12574799.
{{cite journal}}: CS1 maint: DOI inactive as of June 2022 (link)
- Escribano, J.M.; Juan, J.; Bofill, R.; Rodríguez-Mori, A.; Maeso, J.; Fuentes, J.M.; Matas, M. (2005). "Haemodynamic Strategy for Treatment of Diastolic Anterograde Giacomini Varicose Veins". European Journal of Vascular and Endovascular Surgery. 30 (1): 96–101. doi:10.1016/j.ejvs.2005.03.001. PMID 15933990.
- Franceschi, Claude (1988). Théorie et Pratique de la Cure Conservatrice et Hémodynamique de l'Insuffisance Veineuse en Ambulatoire [Theory and Practice of Cure Curator and Venous hemodynamics in the outpatient clinic] (in French) (1st ed.). Précy-sous-Thil: Armançon. ISBN 2-906594-06-7.
- Franceschi, Claude; Zamboni, Paolo (2009). Principles of Venous Hemodynamics. New York: Nova Science Publishers. ISBN 978-1-60692-485-3.
- Galeandro, Aldo Innocente; Quistelli, Giovanni; Scicchitano, Pietro; Gesualdo, Michele; Zito, Annapaola; Caputo, Paola; Carbonara, Rosa; Galgano, Giuseppe; Ciciarello, Francesco (2012). "Doppler ultrasound venous mapping of the lower limbs". Vascular Health and Risk Management. 8: 59–64. doi:10.2147/VHRM.S27552. PMC 3282606. PMID 22371652.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
- Goldman, M.E., Rastegar, R. (2003). "Spontaneous echo contrast videodensity isflow-related and is dependent on the relative concentrations of fibrinogen and red blood cells". JACC. 41 (4). Retrieved 2003-02-20.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)</ref>
- Labropoulos, Nicos; Tiongson, Jay; Pryor, Landon; Tassiopoulos, Apostolos K; Kang, Steven S; Ashraf Mansour, M; Baker, William H (2003). "Definition of venous reflux in lower-extremity veins". Journal of Vascular Surgery. 38 (4): 793–8. doi:10.1016/S0741-5214(03)00424-5. PMID 14560232. S2CID 38397552.
- Lam, S., Raghavendra, B.N. (1986). "Deep venous thrombosis detection by probe compression of veins". J.Ultrasound Med. 5 (2): 89–95. doi:10.7863/jum.1986.5.2.89. PMID 3514943. S2CID 25293123.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- "Lower Extremity Venous Duplex Evaluation" (PDF). Society for Vascular Ultrasound. 2011.
- Markowitz, J. (1981). "Probe Selection, Machine Controls, and Equipment" (PDF). Retrieved 2013-02-24.
- Pierik, E.G.J.M.; Toonder, I.M.; van Urk, H.; Wittens, C.H.A. (1997). "Validation of duplex ultrasonography in detecting competent and incompetent perforating veins in patients with venous ulceration of the lower leg". Journal of Vascular Surgery. 26 (1): 49–52. doi:10.1016/S0741-5214(97)70146-0. PMID 9240321.
- Saliba, Orlando Adas; Giannini, Mariangela; Rollo, Hamilton Almeida (2007). "Métodos de diagnóstico não-invasivos para avaliação da insuficiência venosa dos membros inferiores" [Noninvasive diagnostic methods to evaluate venous insufficiency of the lower limbs]. Jornal Vascular Brasileiro (in Portuguese). 6 (3): 266–75. doi:10.1590/S1677-54492007000300010.
- Training in Diagnostic Ultrasound: Essentials, Principles and Standards: Report of a Who Study Group (PDF). Vol. 875. World Health Organization. 1998. pp. i-46, back cover. ISBN 978-92-4-120875-8. PMID 9659004. Retrieved 2013-02-05.
{{cite book}}:|journal=ignored (help)
- Wong, J.K.F; Duncan, J.L; Nichols, D.M (2003). "Whole-leg Duplex Mapping for Varicose Veins: Observations on Patterns of Reflux in Recurrent and Primary Legs, with Clinical Correlation". European Journal of Vascular and Endovascular Surgery. 25 (3): 267–75. doi:10.1053/ejvs.2002.1830. PMID 12623340.
References
[edit]- ^ SVU 2011.
- ^ Franceschi & Zamboni 2009, pp. 19–28.
- ^ WHO 1998, pp. 7–8.
- ^ a b c WHO 1998, pp. 1–2.
- ^ a b Belem et al. 2004.
- ^ a b c d Galeandro et al. 2012.
- ^ Markowitz 1981.
- ^ a b Cina et al. 2005.
- ^ Franceschi & Zamboni 2009, pp. 21–8.
- ^ WHO 1998, pp. 51–2.
- ^ a b c Cavezzi et al. 2006.
- ^ a b Labropoulos et al. 2003.
- ^ Franceschi & Zamboni 2009, p. 25.
- ^ WHO 1998, p. 26.
- ^ Dauzat 1991, pp. 386–437.
- ^ Goldman 2003.
- ^ Dauzat 1991, pp. 3–7.
- ^ Markowitz, J. "Probe Selection, Machine Controls, and Equipment" (PDF).
- ^ Franceschi 1988, p. 86.
- ^ a b c Coleridge-Smith et al. 2006.
- ^ Raghavendra 1986.
- ^ Dauzat 1991, p. 422.
- ^ Elias et al. 2011.
- ^ Hirsh J., Cogo, A. (1993). "Distribution of Thrombosis in Patients With Symptomatic Deep Vein Thrombosis Implications for simplifying the diagnosis Process with compression ultrasound". JAMA. 153 (24).
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Weir, P., Hollyoak, M. (2001). "Deep venous thrombosis in postoperative vascular surgical patients: A frequent finding without prophylaxis". JVS. 34 (4): 656–660. doi:10.1067/mva.2001.116803. PMID 11668320.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "The Diagnostic Approach to Deep Venous Thrombosis: Diagnostic Tests for Deep Vein Thrombosis". Semin Respir Crit Care Med. 21 (6). 2000.
- ^ Lensing, A.W.A., Jongbloets, L.M.M. (may 1994). "Limitations of compression ultrasound for the detection of symptomless postoperative deep vein thrombosis". The Lancet. 343 (8906): 1142–1144. doi:10.1016/S0140-6736(94)90240-2. PMID 7910237. S2CID 23576444.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: date and year (link) CS1 maint: multiple names: authors list (link) - ^ Franceschi 1988, pp. 84–5.
- ^ a b Franceschi & Zamboni 2009, p. 93.
- ^ Franceschi & Zamboni 2009, pp. 92–4.
- ^ Franceschi & Zamboni 2009, p. 19.
- ^ Franceschi & Zamboni 2009, p. 37.
- ^ Franceschi & Zamboni 2009, p. 81.
- ^ Franceschi & Zamboni 2009, pp. 9–17.
- ^ Saliba, Giannini & Rollo 2007.
- ^ Wong, Duncan & Nichols 2003.
- ^ Zamboni 2009, p. 26.
- ^ WHO 1998, p. 14.
- ^ Caggiati & Ricci 1997.
- ^ Franceschi & Zamboni 2009, p. 14.
- ^ a b c Franceschi & Zamboni 2009, pp. 11–3.
- ^ Escribano et al. 2005.
- ^ Pierik et al. 1997.
- ^ Cobbold 2003, pp. 608–609.
- ^ "History of the AIUM". Archived from the original on 2005-11-03. Retrieved 2013-02-24.
- ^ "The History of Ultrasound: A collection of recollections, articles, interviews and images". www.obgyn.net. Retrieved 2013-02-24.
- ^ descotes J., Pourcelot, L. (1965). "Effet Doppler et mesure du débit sanguin". C.R.Acad.Sc.Paris (261): 253–6.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ R. Eugene Zierler, MD (November 1, 2002). "D. Eugene Strandness, Jr, MD, 1928–2002". Journal of Ultrasound in Medicine.
- ^ Dauzat 1991.
- ^ Feigl P., Sigel B. (1968). "A Doppler Ultrasound method for diagnosing lower extremity venous disease". Surgery, Gynecology & Obstetrics (127): 339–350.
- ^ Baker, D.W., Eyer, M.K. (1981). "Color digital echo-doppler image presentation". Ulrasound in Med. & Bio. 7 (1): 21–31. doi:10.1016/0301-5629(81)90019-3. PMID 6165125. Retrieved 2013-02-24.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Jewell R., Persson A.V. (1989). "Use of triplex scanner in diagnosis of deep venous thrombosis". Arch. Surg. 124 (5): 593–596. doi:10.1001/archsurg.1989.01410050083017. PMID 2653279.
- ^ Dauzat M., Laroche J. P. (1983). "L'echotomographie des veines: proposition d'une méthodologie et illustration des premiers résultats pour le diagnostic des thromboses veineuse profondes". Journal d'Imagerie Médicale. 1: 193–197.
- ^ Franceschi.




