PSMB8
Proteasome subunit beta type-8 as known as 20S proteasome subunit beta-5i is a protein that in humans is encoded by the PSMB8 gene.[4][5][6] This protein is one of the 17 essential subunits (alpha subunits 1–7, constitutive beta subunits 1–7, and inducible subunits including beta1i, beta2i, beta5i) that contributes to the complete assembly of 20S proteasome complex. In particular, proteasome subunit beta type-5, along with other beta subunits, assemble into two heptameric rings and subsequently a proteolytic chamber for substrate degradation. This protein contains "Chymotrypsin-like" activity and is capable of cleaving after large hydrophobic residues of peptide.[7] The eukaryotic proteasome recognized degradable proteins, including damaged proteins for protein quality control purpose or key regulatory protein components for dynamic biological processes. The constitutive subunit beta1, beta2, and beta 5 (systematic nomenclature) can be replaced by their inducible counterparts beta1i, 2i, and 5i when cells are under the treatment of interferon-γ. The resulting proteasome complex becomes the so-called immunoproteasome. An essential function of the modified proteasome complex, the immunoproteasome, is the processing of numerous MHC class-I restricted T cell epitopes.[8]
Structure
[edit]Gene
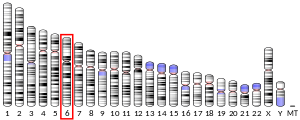
[edit]This gene encodes a member of the proteasome B-type family, also known as the T1B family, that is a 20S core beta subunit. This gene is located in the class II region of the MHC (major histocompatibility complex). Expression of this gene is induced by gamma interferon and this gene product replaces catalytic subunit 3 (proteasome beta 5 subunit) in the immunoproteasome. Proteolytic processing is required to generate a mature subunit. Two alternative transcripts encoding two isoforms have been identified; both isoforms are processed to yield the same mature subunit.[6] The human PSMB8 gene has 7 exons and locates at chromosome band 6p21.3.
Protein structure
[edit]The human protein proteasome subunit beta type-8 is 23 kDa in size and composed of 204 amino acids. The calculated theoretical pI of this protein is 7.59.
Complex assembly
[edit]The proteasome is a multicatalytic proteinase complex with a highly ordered 20S core structure. This barrel-shaped core structure is composed of 4 axially stacked rings of 28 non-identical subunits: the two end rings are each formed by 7 alpha subunits, and the two central rings are each formed by 7 beta subunits. Three beta subunits (beta1, beta2, beta5) each contains a proteolytic active site and has distinct substrate preferences. Proteasomes are distributed throughout eukaryotic cells at a high concentration and cleave peptides in an ATP/ubiquitin-dependent process in a non-lysosomal pathway.[9][10]
Function
[edit]Protein functions are supported by its tertiary structure and its interaction with associating partners. As one of 28 subunits of 20S proteasome, protein proteasome subunit beta type-2 contributes to form a proteolytic environment for substrate degradation. Evidences of the crystal structures of isolated 20S proteasome complex demonstrate that the two rings of beta subunits form a proteolytic chamber and maintain all their active sites of proteolysis within the chamber.[10] Concomitantly, the rings of alpha subunits form the entrance for substrates entering the proteolytic chamber. In an inactivated 20S proteasome complex, the gate into the internal proteolytic chamber are guarded by the N-terminal tails of specific alpha-subunit. This unique structure design prevents random encounter between proteolytic active sites and protein substrate, which makes protein degradation a well-regulated process.[11][12] 20S proteasome complex, by itself, is usually functionally inactive. The proteolytic capacity of 20S core particle (CP) can be activated when CP associates with one or two regulatory particles (RP) on one or both side of alpha rings. These regulatory particles include 19S proteasome complexes, 11S proteasome complex, etc. Following the CP-RP association, the confirmation of certain alpha subunits will change and consequently cause the opening of substrate entrance gate. Besides RPs, the 20S proteasomes can also be effectively activated by other mild chemical treatments, such as exposure to low levels of sodium dodecylsulfate (SDS) or NP-14.[12][13]
The 20S proteasome subunit beta-5i (systematic nomenclature) is originally expressed as a precursor with 276 amino acids. The fragment of 72 amino acids at peptide N-terminal is essential for proper protein folding and subsequent complex assembly. At the end-stage of complex assembly, the N-terminal fragment of beta5i subunit is cleaved, forming the mature beta5i subunit of 20S complex.[14] During the basal assembly, and proteolytic processing is required to generate a mature subunit. The subunit beta5i only presents in the immunoproteasome and is replaced by subunit beta5(proteasome beta 5 subunit) in constitutive 20S proteasome complex.
Clinical significance
[edit]The proteasome and its subunits are of clinical significance for at least two reasons: (1) a compromised complex assembly or a dysfunctional proteasome can be associated with the underlying pathophysiology of specific diseases, and (2) they can be exploited as drug targets for therapeutic interventions. More recently, more effort has been made to consider the proteasome for the development of novel diagnostic markers and strategies. An improved and comprehensive understanding of the pathophysiology of the proteasome should lead to clinical applications in the future.
The proteasomes form a pivotal component for the ubiquitin–proteasome system (UPS) [15] and corresponding cellular Protein Quality Control (PQC). Protein ubiquitination and subsequent proteolysis and degradation by the proteasome are important mechanisms in the regulation of the cell cycle, cell growth and differentiation, gene transcription, signal transduction and apoptosis.[16] Subsequently, a compromised proteasome complex assembly and function lead to reduced proteolytic activities and the accumulation of damaged or misfolded protein species. Such protein accumulation may contribute to the pathogenesis and phenotypic characteristics in neurodegenerative diseases,[17][18] cardiovascular diseases,[19][20][21] inflammatory responses and autoimmune diseases,[22] and systemic DNA damage responses leading to malignancies.[23]
Several experimental and clinical studies have indicated that aberrations and deregulations of the UPS contribute to the pathogenesis of several neurodegenerative and myodegenerative disorders, including Alzheimer's disease,[24] Parkinson's disease[25] and Pick's disease,[26] Amyotrophic lateral sclerosis (ALS),[26] Huntington's disease,[25] Creutzfeldt–Jakob disease,[27] and motor neuron diseases, polyglutamine (PolyQ) diseases, Muscular dystrophies[28] and several rare forms of neurodegenerative diseases associated with dementia.[29] As part of the ubiquitin–proteasome system (UPS), the proteasome maintains cardiac protein homeostasis and thus plays a significant role in cardiac ischemic injury,[30] ventricular hypertrophy[31] and heart failure.[32] Additionally, evidence is accumulating that the UPS plays an essential role in malignant transformation. UPS proteolysis plays a major role in responses of cancer cells to stimulatory signals that are critical for the development of cancer. Accordingly, gene expression by degradation of transcription factors, such as p53, c-jun, c-Fos, NF-κB, c-Myc, HIF-1α, MATα2, STAT3, sterol-regulated element-binding proteins and androgen receptors are all controlled by the UPS and thus involved in the development of various malignancies.[33] Moreover, the UPS regulates the degradation of tumor suppressor gene products such as adenomatous polyposis coli (APC) in colorectal cancer, retinoblastoma (Rb). and von Hippel–Lindau tumor suppressor (VHL), as well as a number of proto-oncogenes (Raf, Myc, Myb, Rel, Src, Mos, ABL). The UPS is also involved in the regulation of inflammatory responses. This activity is usually attributed to the role of proteasomes in the activation of NF-κB which further regulates the expression of pro inflammatory cytokines such as TNF-α, IL-β, IL-8, adhesion molecules (ICAM-1, VCAM-1, P-selectin) and prostaglandins and nitric oxide (NO).[22] Additionally, the UPS also plays a role in inflammatory responses as regulators of leukocyte proliferation, mainly through proteolysis of cyclines and the degradation of CDK inhibitors.[34] Lastly, autoimmune disease patients with SLE, Sjögren syndrome and rheumatoid arthritis (RA) predominantly exhibit circulating proteasomes which can be applied as clinical biomarkers.[35]
During the antigen processing for the major histocompatibility complex (MHC) class-I, the proteasome is the major degradation machinery that degrades the antigen and present the resulting peptides to cytotoxic T lymphocytes.[36][37] The immunoproteasome has been considered playing a critical role in improving the quality and quantity of generated class-I ligands.
The PSMB8 protein has a significant clinical role in autoimmune diseases and inflammatory reactions. For instance, patients with a homozygous missense mutation (G197V) in the immunoproteasome subunit, β type 8 (PSMB8) suffered from autoinflammatory responses that included recurrent fever and nodular erythema together with lipodystrophy. This mutation increased assembly intermediates of immunoproteasomes, resulting in decreased proteasome function and ubiquitin-coupled protein accumulation in the patient's tissues. In the patient's skin and B cells, IL-6 was also highly expressed, and there was a reduced expression of PSMB8. Furthermore, downregulation of PSMB8 also inhibited the differentiation of murine and human adipocytes in vitro, while an injection of siRNA against Psmb8 in mouse skin could reduce adipocyte tissue volume. Thus, PSMB8 may be an essential component and regulator not only for inflammation, but also in the differentiation of adipocytes, hereby indicating that immunoproteasomes may have pleiotropic functions to maintain the homeostasis of a variety of cell types.[38] Subsequently, in addition to autoimmune diseases the PSMB8 protein also has been linked in the diagnosis of lipodystrophy syndrome.[39] Glycosylation disorders are sometimes involved. Some genetically determined forms have recently been found to be due to autoinflammatory syndromes linked to a proteasome anomaly through PSMB8. They result in a lipodystrophy syndrome that occurs secondarily with fever, dermatosis and panniculitis,[39][40] and Nakajo-Nishimura syndrome,[41] a distinct inherited inflammatory and wasting disease that is originated from Japan. Patients with Nakajo-Nishimura syndrome, develop periodic high fever and nodular erythema-like eruptions, and gradually progress lipomuscular atrophy in the upper body, mainly the face and the upper extremities, to show the characteristic thin facial appearance and long clubbed fingers with joint contractures.[42]
References
[edit]- ^ a b c ENSG00000206298, ENSG00000230034, ENSG00000235715, ENSG00000231631, ENSG00000204264, ENSG00000226201, ENSG00000236443 GRCh38: Ensembl release 89: ENSG00000230669, ENSG00000206298, ENSG00000230034, ENSG00000235715, ENSG00000231631, ENSG00000204264, ENSG00000226201, ENSG00000236443 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Bodmer JG, Marsh SG, Albert ED, Bodmer WF, Dupont B, Erlich HA, Mach B, Mayr WR, Parham P, Sasazuki T (Apr 1992). "Nomenclature for factors of the HLA system, 1991. WHO Nomenclature Committee for factors of the HLA system". Tissue Antigens. 39 (4): 161–73. doi:10.1111/j.1399-0039.1992.tb01932.x. PMID 1529427.
- ^ Schmidt M, Zantopf D, Kraft R, Kostka S, Preissner R, Kloetzel PM (Apr 1999). "Sequence information within proteasomal prosequences mediates efficient integration of beta-subunits into the 20 S proteasome complex". Journal of Molecular Biology. 288 (1): 117–28. doi:10.1006/jmbi.1999.2660. PMID 10329130.
- ^ a b "Entrez Gene: PSMB8 proteasome (prosome, macropain) subunit, beta type, 8 (large multifunctional peptidase 7)".
- ^ Coux O, Tanaka K, Goldberg AL (November 1996). "Structure and functions of the 20S and 26S proteasomes". Annual Review of Biochemistry. 65: 801–47. doi:10.1146/annurev.bi.65.070196.004101. PMID 8811196.
- ^ Basler M, Kirk CJ, Groettrup M (Feb 2013). "The immunoproteasome in antigen processing and other immunological functions". Current Opinion in Immunology (Submitted manuscript). 25 (1): 74–80. doi:10.1016/j.coi.2012.11.004. PMID 23219269.
- ^ Coux O, Tanaka K, Goldberg AL (1996). "Structure and functions of the 20S and 26S proteasomes". Annual Review of Biochemistry. 65: 801–47. doi:10.1146/annurev.bi.65.070196.004101. PMID 8811196.
- ^ a b Tomko RJ, Hochstrasser M (2013). "Molecular architecture and assembly of the eukaryotic proteasome". Annual Review of Biochemistry. 82: 415–45. doi:10.1146/annurev-biochem-060410-150257. PMC 3827779. PMID 23495936.
- ^ Groll M, Ditzel L, Löwe J, Stock D, Bochtler M, Bartunik HD, Huber R (Apr 1997). "Structure of 20S proteasome from yeast at 2.4 A resolution". Nature. 386 (6624): 463–71. Bibcode:1997Natur.386..463G. doi:10.1038/386463a0. PMID 9087403. S2CID 4261663.
- ^ a b Groll M, Bajorek M, Köhler A, Moroder L, Rubin DM, Huber R, Glickman MH, Finley D (Nov 2000). "A gated channel into the proteasome core particle". Nature Structural Biology. 7 (11): 1062–7. doi:10.1038/80992. PMID 11062564. S2CID 27481109.
- ^ Zong C, Gomes AV, Drews O, Li X, Young GW, Berhane B, Qiao X, French SW, Bardag-Gorce F, Ping P (Aug 2006). "Regulation of murine cardiac 20S proteasomes: role of associating partners". Circulation Research. 99 (4): 372–80. doi:10.1161/01.RES.0000237389.40000.02. PMID 16857963.
- ^ Yang Y, Früh K, Ahn K, Peterson PA (Nov 1995). "In vivo assembly of the proteasomal complexes, implications for antigen processing". The Journal of Biological Chemistry. 270 (46): 27687–94. doi:10.1074/jbc.270.46.27687. PMID 7499235.
- ^ Kleiger G, Mayor T (Jun 2014). "Perilous journey: a tour of the ubiquitin-proteasome system". Trends in Cell Biology. 24 (6): 352–9. doi:10.1016/j.tcb.2013.12.003. PMC 4037451. PMID 24457024.
- ^ Goldberg AL, Stein R, Adams J (Aug 1995). "New insights into proteasome function: from archaebacteria to drug development". Chemistry & Biology. 2 (8): 503–8. doi:10.1016/1074-5521(95)90182-5. PMID 9383453.
- ^ Sulistio YA, Heese K (Jan 2015). "The Ubiquitin–Proteasome System and Molecular Chaperone Deregulation in Alzheimer's Disease". Molecular Neurobiology. 53 (2): 905–31. doi:10.1007/s12035-014-9063-4. PMID 25561438. S2CID 14103185.
- ^ Ortega Z, Lucas JJ (2014). "Ubiquitin–proteasome system involvement in Huntington's disease". Frontiers in Molecular Neuroscience. 7: 77. doi:10.3389/fnmol.2014.00077. PMC 4179678. PMID 25324717.
- ^ Sandri M, Robbins J (Jun 2014). "Proteotoxicity: an underappreciated pathology in cardiac disease". Journal of Molecular and Cellular Cardiology. 71: 3–10. doi:10.1016/j.yjmcc.2013.12.015. PMC 4011959. PMID 24380730.
- ^ Drews O, Taegtmeyer H (Dec 2014). "Targeting the ubiquitin–proteasome system in heart disease: the basis for new therapeutic strategies". Antioxidants & Redox Signaling. 21 (17): 2322–43. doi:10.1089/ars.2013.5823. PMC 4241867. PMID 25133688.
- ^ Wang ZV, Hill JA (Feb 2015). "Protein quality control and metabolism: bidirectional control in the heart". Cell Metabolism. 21 (2): 215–26. doi:10.1016/j.cmet.2015.01.016. PMC 4317573. PMID 25651176.
- ^ a b Karin M, Delhase M (Feb 2000). "The I kappa B kinase (IKK) and NF-kappa B: key elements of proinflammatory signalling". Seminars in Immunology. 12 (1): 85–98. doi:10.1006/smim.2000.0210. PMID 10723801.
- ^ Ermolaeva MA, Dakhovnik A, Schumacher B (Jan 2015). "Quality control mechanisms in cellular and systemic DNA damage responses". Ageing Research Reviews. 23 (Pt A): 3–11. doi:10.1016/j.arr.2014.12.009. PMC 4886828. PMID 25560147.
- ^ Checler F, da Costa CA, Ancolio K, Chevallier N, Lopez-Perez E, Marambaud P (Jul 2000). "Role of the proteasome in Alzheimer's disease". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1502 (1): 133–8. doi:10.1016/s0925-4439(00)00039-9. PMID 10899438.
- ^ a b Chung KK, Dawson VL, Dawson TM (Nov 2001). "The role of the ubiquitin-proteasomal pathway in Parkinson's disease and other neurodegenerative disorders". Trends in Neurosciences. 24 (11 Suppl): S7–14. doi:10.1016/s0166-2236(00)01998-6. PMID 11881748. S2CID 2211658.
- ^ a b Ikeda K, Akiyama H, Arai T, Ueno H, Tsuchiya K, Kosaka K (Jul 2002). "Morphometrical reappraisal of motor neuron system of Pick's disease and amyotrophic lateral sclerosis with dementia". Acta Neuropathologica. 104 (1): 21–8. doi:10.1007/s00401-001-0513-5. PMID 12070660. S2CID 22396490.
- ^ Manaka H, Kato T, Kurita K, Katagiri T, Shikama Y, Kujirai K, Kawanami T, Suzuki Y, Nihei K, Sasaki H (May 1992). "Marked increase in cerebrospinal fluid ubiquitin in Creutzfeldt–Jakob disease". Neuroscience Letters. 139 (1): 47–9. doi:10.1016/0304-3940(92)90854-z. PMID 1328965. S2CID 28190967.
- ^ Mathews KD, Moore SA (Jan 2003). "Limb-girdle muscular dystrophy". Current Neurology and Neuroscience Reports. 3 (1): 78–85. doi:10.1007/s11910-003-0042-9. PMID 12507416. S2CID 5780576.
- ^ Mayer RJ (Mar 2003). "From neurodegeneration to neurohomeostasis: the role of ubiquitin". Drug News & Perspectives. 16 (2): 103–8. doi:10.1358/dnp.2003.16.2.829327. PMID 12792671.
- ^ Calise J, Powell SR (Feb 2013). "The ubiquitin proteasome system and myocardial ischemia". American Journal of Physiology. Heart and Circulatory Physiology. 304 (3): H337–49. doi:10.1152/ajpheart.00604.2012. PMC 3774499. PMID 23220331.
- ^ Predmore JM, Wang P, Davis F, Bartolone S, Westfall MV, Dyke DB, Pagani F, Powell SR, Day SM (Mar 2010). "Ubiquitin proteasome dysfunction in human hypertrophic and dilated cardiomyopathies". Circulation. 121 (8): 997–1004. doi:10.1161/CIRCULATIONAHA.109.904557. PMC 2857348. PMID 20159828.
- ^ Powell SR (Jul 2006). "The ubiquitin-proteasome system in cardiac physiology and pathology". American Journal of Physiology. Heart and Circulatory Physiology. 291 (1): H1–H19. doi:10.1152/ajpheart.00062.2006. PMID 16501026. S2CID 7073263.
- ^ Adams J (Apr 2003). "Potential for proteasome inhibition in the treatment of cancer". Drug Discovery Today. 8 (7): 307–15. doi:10.1016/s1359-6446(03)02647-3. PMID 12654543.
- ^ Ben-Neriah Y (Jan 2002). "Regulatory functions of ubiquitination in the immune system". Nature Immunology. 3 (1): 20–6. doi:10.1038/ni0102-20. PMID 11753406. S2CID 26973319.
- ^ Egerer K, Kuckelkorn U, Rudolph PE, Rückert JC, Dörner T, Burmester GR, Kloetzel PM, Feist E (Oct 2002). "Circulating proteasomes are markers of cell damage and immunologic activity in autoimmune diseases". The Journal of Rheumatology. 29 (10): 2045–52. PMID 12375310.
- ^ Basler M, Lauer C, Beck U, Groettrup M (Nov 2009). "The proteasome inhibitor bortezomib enhances the susceptibility to viral infection". Journal of Immunology. 183 (10): 6145–50. doi:10.4049/jimmunol.0901596. PMID 19841190.
- ^ Rock KL, Gramm C, Rothstein L, Clark K, Stein R, Dick L, Hwang D, Goldberg AL (Sep 1994). "Inhibitors of the proteasome block the degradation of most cell proteins and the generation of peptides presented on MHC class I molecules". Cell. 78 (5): 761–71. doi:10.1016/s0092-8674(94)90462-6. PMID 8087844. S2CID 22262916.
- ^ Kitamura A, Maekawa Y, Uehara H, Izumi K, Kawachi I, Nishizawa M, Toyoshima Y, Takahashi H, Standley DM, Tanaka K, Hamazaki J, Murata S, Obara K, Toyoshima I, Yasutomo K (Oct 2011). "A mutation in the immunoproteasome subunit PSMB8 causes autoinflammation and lipodystrophy in humans". The Journal of Clinical Investigation. 121 (10): 4150–60. doi:10.1172/JCI58414. PMC 3195477. PMID 21881205.
- ^ a b Vantyghem MC, Balavoine AS, Douillard C, Defrance F, Dieudonne L, Mouton F, Lemaire C, Bertrand-Escouflaire N, Bourdelle-Hego MF, Devemy F, Evrard A, Gheerbrand D, Girardot C, Gumuche S, Hober C, Topolinski H, Lamblin B, Mycinski B, Ryndak A, Karrouz W, Duvivier E, Merlen E, Cortet C, Weill J, Lacroix D, Wémeau JL (Jun 2012). "How to diagnose a lipodystrophy syndrome". Annales d'Endocrinologie. 73 (3): 170–89. doi:10.1016/j.ando.2012.04.010. PMID 22748602.
- ^ Garg A (Nov 2011). "Clinical review#: Lipodystrophies: genetic and acquired body fat disorders". The Journal of Clinical Endocrinology and Metabolism. 96 (11): 3313–25. doi:10.1210/jc.2011-1159. PMC 7673254. PMID 21865368.
- ^ Kanazawa N (2012). "Nakajo-Nishimura syndrome: An autoinflammatory disorder showing pernio-like rashes and progressive partial lipodystrophy". Allergology International. 61 (2): 197–206. doi:10.2332/allergolint.11-RAI-0416. PMID 22441638.
- ^ Kanazawa N, Arima K, Ida H, Yoshiura K, Furukawa F (2011). "[Nakajo-Nishimura syndrome]". Nihon Rinsho Men'eki Gakkai Kaishi = Japanese Journal of Clinical Immunology. 34 (5): 388–400. doi:10.2177/jsci.34.388. PMID 22041427.
Further reading
[edit]- Coux O, Tanaka K, Goldberg AL (1996). "Structure and functions of the 20S and 26S proteasomes". Annual Review of Biochemistry. 65: 801–47. doi:10.1146/annurev.bi.65.070196.004101. PMID 8811196.
- Goff SP (Aug 2003). "Death by deamination: a novel host restriction system for HIV-1". Cell. 114 (3): 281–3. doi:10.1016/S0092-8674(03)00602-0. PMID 12914693. S2CID 16340355.
- Früh K, Yang Y, Arnold D, Chambers J, Wu L, Waters JB, Spies T, Peterson PA (Nov 1992). "Alternative exon usage and processing of the major histocompatibility complex-encoded proteasome subunits". The Journal of Biological Chemistry. 267 (31): 22131–40. doi:10.1016/S0021-9258(18)41645-6. PMID 1429565.
- Beck S, Kelly A, Radley E, Khurshid F, Alderton RP, Trowsdale J (Nov 1992). "DNA sequence analysis of 66 kb of the human MHC class II region encoding a cluster of genes for antigen processing". Journal of Molecular Biology. 228 (2): 433–41. doi:10.1016/0022-2836(92)90832-5. PMID 1453454.
- Glynne R, Powis SH, Beck S, Kelly A, Kerr LA, Trowsdale J (Sep 1991). "A proteasome-related gene between the two ABC transporter loci in the class II region of the human MHC". Nature. 353 (6342): 357–60. Bibcode:1991Natur.353..357G. doi:10.1038/353357a0. PMID 1922342. S2CID 4369131.
- Ustrell V, Realini C, Pratt G, Rechsteiner M (Dec 1995). "Human lymphoblast and erythrocyte multicatalytic proteases: differential peptidase activities and responses to the 11S regulator". FEBS Letters. 376 (3): 155–8. doi:10.1016/0014-5793(95)01257-9. PMID 7498531. S2CID 8558045.
- Kristensen P, Johnsen AH, Uerkvitz W, Tanaka K, Hendil KB (Dec 1994). "Human proteasome subunits from 2-dimensional gels identified by partial sequencing". Biochemical and Biophysical Research Communications. 205 (3): 1785–9. doi:10.1006/bbrc.1994.2876. PMID 7811265.
- Meinhardt T, Gräf U, Hämmerling GJ (1993). "Different genomic structure of mouse and human Lmp7 genes: characterization of MHC-encoded proteasome genes". Immunogenetics. 38 (5): 373–9. doi:10.1007/BF00210482. PMID 8344725. S2CID 39693212.
- Glynne R, Kerr LA, Mockridge I, Beck S, Kelly A, Trowsdale J (Apr 1993). "The major histocompatibility complex-encoded proteasome component LMP7: alternative first exons and post-translational processing". European Journal of Immunology. 23 (4): 860–6. doi:10.1002/eji.1830230414. PMID 8458375. S2CID 44733094.
- Roby KF, Yang Y, Gershon D, Hunt JS (Nov 1995). "Cellular distribution of proteasome subunit Lmp7 mRNA and protein in human placentas". Immunology. 86 (3): 469–74. PMC 1383953. PMID 8550087.
- Beck S, Abdulla S, Alderton RP, Glynne RJ, Gut IG, Hosking LK, Jackson A, Kelly A, Newell WR, Sanseau P, Radley E, Thorpe KL, Trowsdale J (Jan 1996). "Evolutionary dynamics of non-coding sequences within the class II region of the human MHC". Journal of Molecular Biology. 255 (1): 1–13. doi:10.1006/jmbi.1996.0001. PMID 8568858.
- Hisamatsu H, Shimbara N, Saito Y, Kristensen P, Hendil KB, Fujiwara T, Takahashi E, Tanahashi N, Tamura T, Ichihara A, Tanaka K (Apr 1996). "Newly identified pair of proteasomal subunits regulated reciprocally by interferon gamma". The Journal of Experimental Medicine. 183 (4): 1807–16. doi:10.1084/jem.183.4.1807. PMC 2192534. PMID 8666937.
- Seeger M, Ferrell K, Frank R, Dubiel W (Mar 1997). "HIV-1 tat inhibits the 20 S proteasome and its 11 S regulator-mediated activation". The Journal of Biological Chemistry. 272 (13): 8145–8. doi:10.1074/jbc.272.13.8145. PMID 9079628.
- Kim TG, Lee YH, Choi HB, Han H (Mar 1996). "Two newly discovered alleles of major histocompatibility complex-encoded LMP7 in Korean populations". Human Immunology. 46 (1): 61–4. doi:10.1016/0198-8859(95)00172-7. PMID 9157092.
- Vives-Pi M, Vargas F, James RF, Trowsdale J, Costa M, Sospedra M, Somoza N, Obiols G, Tampé R, Pujol-Borrell R (Aug 1997). "Proteasome subunits, low-molecular-mass polypeptides 2 and 7 are hyperexpressed by target cells in autoimmune thyroid disease but not in insulin-dependent diabetes mellitus: implications for autoimmunity". Tissue Antigens. 50 (2): 153–63. doi:10.1111/j.1399-0039.1997.tb02854.x. PMID 9271825.
- Madani N, Kabat D (Dec 1998). "An endogenous inhibitor of human immunodeficiency virus in human lymphocytes is overcome by the viral Vif protein". Journal of Virology. 72 (12): 10251–5. doi:10.1128/JVI.72.12.10251-10255.1998. PMC 110608. PMID 9811770.
- Simon JH, Gaddis NC, Fouchier RA, Malim MH (Dec 1998). "Evidence for a newly discovered cellular anti-HIV-1 phenotype". Nature Medicine. 4 (12): 1397–400. doi:10.1038/3987. PMID 9846577. S2CID 25235070.
- Sewell AK, Price DA, Teisserenc H, Booth BL, Gileadi U, Flavin FM, Trowsdale J, Phillips RE, Cerundolo V (Jun 1999). "IFN-gamma exposes a cryptic cytotoxic T lymphocyte epitope in HIV-1 reverse transcriptase". Journal of Immunology. 162 (12): 7075–9. doi:10.4049/jimmunol.162.12.7075. PMID 10358150. S2CID 255320218.