Inactivated vaccine
| Inactivated vaccine | |
|---|---|
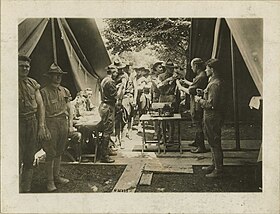 Typhoid prophylaxis for soldiers in World War I. | |
| Other names | Killed vaccine Non-replicating vaccines |
| Specialty | Public health, immunology, family medicine, general practice |
| Uses | prevention of infectious diseases |
| Frequency | birth to adulthood |
| Outcomes | development of active immunity in individuals; contribution to herd immunity |
An inactivated vaccine (or killed vaccine) is a type of vaccine that contains pathogens (such as virus or bacteria) that have been killed or rendered inactive, so they cannot replicate or cause disease. In contrast, live vaccines use pathogens that are still alive (but are almost always attenuated, that is, weakened). Pathogens for inactivated vaccines are grown under controlled conditions and are killed as a means to reduce infectivity and thus prevent infection from the vaccine.[1]
Inactivated vaccines were first developed in the late 1800s and early 1900s for cholera, plague, and typhoid.[2] In 1897, Japanese scientists developed an inactivated vaccine for the bubonic plague. In the 1950's, Jonas Salk created an inactivated vaccine for the poliovirus, creating the first vaccine that was both safe and effective against polio. Today, inactivated vaccines exist for many pathogens, including influenza, polio (IPV), rabies, hepatitis A, CoronaVac, Covaxin and pertussis.[3][4]
Because inactivated pathogens tend to produce a weaker response by the immune system than live pathogens, immunologic adjuvants and multiple "booster" injections may be required in some vaccines to provide an effective immune response against the pathogen.[1][5][6] Attenuated vaccines are often preferable for generally healthy people because a single dose is often safe and very effective. However, some people cannot take attenuated vaccines because the pathogen poses too much risk for them (for example, elderly people or people with immunodeficiency). For those patients, an inactivated vaccine can provide protection.[citation needed]
Mechanism
[edit]The pathogen particles are destroyed and cannot divide, but the pathogens maintain some of their integrity to be recognized by the immune system and evoke an adaptive immune response.[7][8] When manufactured correctly, the vaccine is not infectious, but improper inactivation can result in intact and infectious particles.[citation needed]
When a vaccine is administered, the antigen will be taken up by an antigen-presenting cell (APC) and transported to a draining lymph node in vaccinated people. The APC will place a piece of the antigen, an epitope, on its surface along with a major histocompatibility complex (MHC) molecule. It can now interact with and activate T cells. The resulting helper T cells will then stimulate an antibody-mediated or cell-mediated immune response and develop an antigen-specific adaptive response.[9][10] This process creates an immunological memory against the specific pathogen and allows the immune system to respond more effectively and rapidly after subsequent encounters with that pathogen.[7][9][10]
Inactivated vaccines tend to produce an immune response that is primarily antibody-mediated.[3][11] However, deliberate adjuvant selection allows inactivated vaccines to stimulate a more robust cell-mediated immune response.[1][8]
Social Consequences
[edit]The use of inactivated vaccines helped reduce morbidity and mortality from diseases like tetanus, diphtheria, and pertussis, creating a healthier, more stable society. Community health improved as a result, particularly in developed nations, where high vaccination rates led to herd immunity.[12]
Reducing diseases like polio, hepatitis A, and influenza meant fewer people suffering from debilitating illness, which in turn led to increased social productivity. Families no longer had to care for loved ones with debilitating diseases, and children could go to school without the constant fear of contraction. Inactivated vaccines increased public trust in public health systems, normalizing vaccinations to the point where yearly flu shots and childhood immunization are seen as routine parts of life, especially in developed countries.[12]
Types
[edit]Inactivated vaccines can be divided by the method used for killing the pathogen.[5][1]
- Whole pathogen inactivated vaccines are produced when an entire pathogen is 'killed' using heat, chemicals, or radiation,[6] although only formaldehyde and beta-Propiolactone exposure are widely used in human vaccines.[13][14]
- Split virus vaccines are produced by using a detergent to disrupt the viral envelope.[5][15] This technique is used in the development of many influenza vaccines.[16]
A minority of sources use the term inactivated vaccines to broadly refer to non-live vaccines. Under this definition, inactivated vaccines also include subunit vaccines and toxoid vaccines.[3][9]
Examples
[edit]Types include:[17]
- Viral:
- Bacterial:
- Injected typhoid vaccine
- Cholera vaccine
- Plague vaccine
- Whole-cell Pertussis vaccine
Advantages and disadvantages
[edit]Advantages
[edit]- Inactivated pathogens are more stable than live pathogens. Increased stability facilitates the storage and transport of inactivated vaccines.[9][18][19]
- Unlike live attenuated vaccines, inactivated vaccines cannot revert to a virulent form and cause disease.[7][11] For example, there have been rare instances of the live attenuated form of poliovirus present in the oral polio vaccine (OPV) becoming virulent, leading to the inactivated polio vaccine (IPV) replacing OPV in many countries with controlled wild-type polio transmission.[7][10]
- Unlike live attenuated vaccines, inactivated vaccines do not replicate and are not contraindicated for immunocompromised individuals.[7][8][9]
Disadvantages
[edit]- Inactivated vaccines have a reduced ability to produce a robust immune response for long-lasting immunity when compared to live attenuated vaccines.[3] Adjuvants and boosters are often required to produce and maintain protective immunity.[11][18]
- Pathogens must be cultured and inactivated for the creation of killed whole-organism vaccines.[7][10] This process slows down vaccine production when compared to genetic vaccines.[9]
- Inactivated vaccines tend to produce less durable immunity, often requiring multiple doses, which can pose a public health challenge. For example, the flu vaccine requires annual updates and re-administration, and hepatitis A vaccines often require two doses spaced six months apart.
References
[edit]- ^ a b c d Petrovsky N, Aguilar JC (October 2004). "Vaccine adjuvants: current state and future trends". Immunology and Cell Biology. 82 (5): 488–496. doi:10.1111/j.0818-9641.2004.01272.x. PMID 15479434. S2CID 154670.
- ^ Plotkin SA, Plotkin SL (October 2011). "The development of vaccines: how the past led to the future". Nature Reviews. Microbiology. 9 (12) (published 2011-10-03): 889–893. doi:10.1038/nrmicro2668. PMID 21963800. S2CID 32506969.
- ^ a b c d Wodi AP, Morelli V (2021). "Chapter 1: Principles of Vaccination" (PDF). In Hall E, Wodi AP, Hamborsky J, Morelli V, Schilllie S (eds.). Epidemiology and Prevention of Vaccine-Preventable Diseases (14th ed.). Washington, D.C.: Public Health Foundation, Centers for Disease Control and Prevention.
- ^ Brown, Jonathan (1997). The History of Medicine: A Scandalously Short Introduction (1st ed.). W.W. Norton & Company. pp. 1–530. ISBN 978-0-393-31611-7.
- ^ a b c WHO Expert Committee on Biological Standardization (19 June 2019). "Influenza". World Health Organization (WHO). Retrieved 22 October 2021.
- ^ a b "Types of Vaccines". Vaccines.gov. U.S. Department of Health and Human Services. 23 July 2013. Archived from the original on 9 June 2013. Retrieved 16 May 2016.
- ^ a b c d e f Vetter V, Denizer G, Friedland LR, Krishnan J, Shapiro M (March 2018). "Understanding modern-day vaccines: what you need to know". Annals of Medicine. 50 (2): 110–120. doi:10.1080/07853890.2017.1407035. PMID 29172780. S2CID 25514266.
- ^ a b c Slifka MK, Amanna I (May 2014). "How advances in immunology provide insight into improving vaccine efficacy". Vaccine. 32 (25): 2948–2957. doi:10.1016/j.vaccine.2014.03.078. PMC 4096845. PMID 24709587.
- ^ a b c d e f Pollard AJ, Bijker EM (February 2021). "A guide to vaccinology: from basic principles to new developments". Nature Reviews. Immunology. 21 (2): 83–100. doi:10.1038/s41577-020-00479-7. PMC 7754704. PMID 33353987.
- ^ a b c d Karch CP, Burkhard P (November 2016). "Vaccine technologies: From whole organisms to rationally designed protein assemblies". Biochemical Pharmacology. 120: 1–14. doi:10.1016/j.bcp.2016.05.001. PMC 5079805. PMID 27157411.
- ^ a b c Pecetta, Simone; Ahmed, S. Sohail; Ellis, Ronald; Rappuoli, Rino (2023). "Technologies for Making New Vaccines". Plotkin's Vaccines. pp. 1350–1373.e9. doi:10.1016/B978-0-323-79058-1.00067-0. ISBN 978-0-323-79058-1.
- ^ a b Oshinsky, David M. (2005). Polio: An American Story. Oxford University Press. ISBN 978-0-19-515294-4.[page needed]
- ^ Sanders B, Koldijk M, Schuitemaker H (2015). "Inactivated Viral Vaccines". Vaccine Analysis: Strategies, Principles, and Control. pp. 45–80. doi:10.1007/978-3-662-45024-6_2. ISBN 978-3-662-45023-9. PMC 7189890. S2CID 81212732.
- ^ Hotez, Peter J.; Bottazzi, Maria Elena (27 January 2022). "Whole Inactivated Virus and Protein-Based COVID-19 Vaccines". Annual Review of Medicine. 73 (1): 55–64. doi:10.1146/annurev-med-042420-113212. ISSN 0066-4219. PMID 34637324. S2CID 238747462.
- ^ Chen J, Wang J, Zhang J, Ly H (2021). "Advances in Development and Application of Influenza Vaccines". Frontiers in Immunology. 12: 711997. doi:10.3389/fimmu.2021.711997. PMC 8313855. PMID 34326849.
- ^ Gemmill I, Young K, et al. (National Advisory Committee on Immunization (NACI)) (May 2018). "Summary of the NACI literature review on the comparative effectiveness and immunogenicity of subunit and split virus inactivated influenza vaccines in older adults". Can Commun Dis Rep (CCDR). 44 (6): 129–133. doi:10.14745/ccdr.v44i06a02.
- ^ Ghaffar A, Haqqi T. "Immunization". Immunology. The Board of Trustees of the University of South Carolina. Archived from the original on 26 February 2014. Retrieved 2009-03-10.
- ^ a b Clem AS (January 2011). "Fundamentals of vaccine immunology". Journal of Global Infectious Diseases. 3 (1): 73–78. doi:10.4103/0974-777X.77299. PMC 3068582. PMID 21572612.
- ^ "Inactivated whole-cell (killed antigen) vaccines - WHO Vaccine Safety Basics". vaccine-safety-training.org. World Health Organization (WHO). Retrieved 2021-11-11.
