Influenza A virus subtype H5N1
| Influenza A virus | |
|---|---|
| |
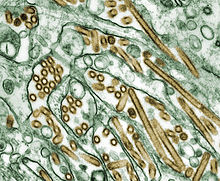
| Colorized transmission electron micrograph of Avian influenza A H5N1 viruses (seen in gold) grown in MDCK cells (seen in green) | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Insthoviricetes |
| Order: | Articulavirales |
| Family: | Orthomyxoviridae |
| Genus: | Alphainfluenzavirus |
| Species: | Influenza A virus
|
| Notable strains | |
Influenza A virus subtype H5N1 (A/H5N1) is a subtype of the influenza A virus, which causes influenza (flu), predominantly in birds. It is enzootic (maintained in the population) in many bird populations, and also panzootic (affecting animals of many species over a wide area).[1] A/H5N1 virus can also infect mammals (including humans) that have been exposed to infected birds; in these cases, symptoms are frequently severe or fatal.[2]
A/H5N1 virus is shed in the saliva, mucus, and feces of infected birds; other infected animals may shed bird flu viruses in respiratory secretions and other body fluids (such as milk).[3] The virus can spread rapidly through poultry flocks and among wild birds.[3] An estimated half a billion farmed birds have been slaughtered in efforts to contain the virus.[2]
Symptoms of A/H5N1 influenza vary according to both the strain of virus underlying the infection and on the species of bird or mammal affected.[4][5] Classification as either Low Pathogenic Avian Influenza (LPAI) or High Pathogenic Avian Influenza (HPAI) is based on the severity of symptoms in domestic chickens and does not predict the severity of symptoms in other species.[6] Chickens infected with LPAI A/H5N1 virus display mild symptoms or are asymptomatic, whereas HPAI A/H5N1 causes serious breathing difficulties, a significant drop in egg production, and sudden death.[7]
In mammals, including humans, A/H5N1 influenza (whether LPAI or HPAI) is rare. Symptoms of infection vary from mild to severe, including fever, diarrhoea, and cough.[5] Human infections with A/H5N1 virus have been reported in 23 countries since 1997, resulting in severe pneumonia and death in about 50% of cases.[8] Between 2003 and October 2024, the World Health Organization has recorded 921 cases of confirmed H5N1 influenza, leading to 464 deaths.[9] The true fatality rate may be lower because some cases with mild symptoms may not have been identified as H5N1.[10]
A/H5N1 influenza virus was first identified in farmed birds in southern China in 1996.[11] Between 1996 and 2018, A/H5N1 coexisted in bird populations with other subtypes of the virus, but since then, the highly pathogenic subtype HPAI A(H5N1) has become the dominant strain in bird populations worldwide.[12] Some strains of A/H5N1 which are highly pathogenic to chickens have adapted to cause mild symptoms in ducks and geese,[13][6] and are able to spread rapidly through bird migration.[14] Mammal species in addition to humans that have been recorded with H5N1 infection include cows, seals, goats, and skunks.[15]
Due to the high lethality and virulence of HPAI A(H5N1), its worldwide presence, its increasingly diverse host reservoir, and its significant ongoing mutations, the H5N1 virus is regarded as the world's largest pandemic threat.[16] Domestic poultry may potentially be protected from specific strains of the virus by vaccination.[17] In the event of a serious outbreak of H5N1 flu among humans, health agencies have prepared "candidate" vaccines that may be used to prevent infection and control the outbreak; however, it could take several months to ramp up mass production.[3][18][19]
Signs and symptoms
[edit]Humans
[edit]Avian flu viruses, both HPAI and LPAI, can infect humans who are in close, unprotected contact with infected poultry. Incidents of cross-species transmission are rare, with symptoms ranging in severity from no symptoms or mild illness, to severe disease that resulted in death.[22][23] As of February, 2024 there have been very few instances of human-to-human transmission, and each outbreak has been limited to a few people.[24] All subtypes of avian Influenza A have potential to cross the species barrier, with H5N1 and H7N9 considered the biggest threats.[25][26]
In order to avoid infection, the general public are advised to avoid contact with sick birds or potentially contaminated material such as carcasses or feces. People working with birds, such as conservationists or poultry workers, are advised to wear appropriate personal protection equipment.[27]
The avian influenza hemagglutinin prefers to bind to alpha-2,3 sialic acid receptors, while the human influenza hemagglutinin prefers to bind to alpha-2,6 sialic acid receptors.[28][29] This means that when the H5N1 strain infects humans, it will replicate in the lower respiratory tract (where alpha-2,3 sialic acid receptors are more plentiful in humans) and consequently cause viral pneumonia.[30][31]
Between 2003 and October 2024, the World Health Organization has recorded 921 cases of confirmed H5N1 influenza, leading to 464 deaths.[32] The true fatality rate may be lower because some cases with mild symptoms may not have been identified as H5N1.[10]
Virology
[edit]Influenza virus nomenclature
[edit]
To unambiguously describe a specific isolate of virus, researchers use the internationally accepted Influenza virus nomenclature,[33] which describes, among other things, the species of animal from which the virus was isolated, and the place and year of collection. For example, A/chicken/Nakorn-Patom/Thailand/CU-K2/04(H5N1):
- A stands for the genus of influenza (A, B or C).
- chicken is the animal species the isolate was found in (note: human isolates lack this component term and are thus identified as human isolates by default)
- Nakorn-Patom/Thailand is the place this specific virus was isolated
- CU-K2 is the laboratory reference number that identifies it from other influenza viruses isolated at the same place and year
- 04 represents the year of isolation 2004
- H5 stands for the fifth of several known types of the protein hemagglutinin.
- N1 stands for the first of several known types of the protein neuraminidase.
Other examples include: A/duck/Hong Kong/308/78(H5N3), and A/shoveler/Egypt/03(H5N2).[34]
Genetic structure
[edit]
H5N1 is a subtype of Influenza A virus. Like all subtypes it is an enveloped negative-sense RNA virus, with a segmented genome.[35] Subtypes of IAV are defined by the combination of the antigenic hemagglutinin and neuraminidase proteins in the viral envelope. "H5N1" designates an IAV subtype that has a type 5 hemagglutinin (H) protein and a type-1 neuraminidase (N) protein.[36] Further variations exist within the subtypes and can lead to very significant differences in the virus's ability to infect and cause disease, as well as to the severity of symptoms.[37][38]
Influenza viruses have a relatively high mutation rate that is characteristic of RNA viruses.[39] The segmentation of its genome facilitates genetic recombination by segment reassortment in hosts infected with two different strains of influenza viruses at the same time.[40][41] Through a combination of mutation and genetic reassortment the virus can evolve to acquire new characteristics, enabling it to evade host immunity and occasionally to jump from one species of host to another.[42][43]
Prevention and treatment
[edit]Vaccine
[edit]Humans - Several "candidate" (unproved) vaccines are available in case an avian virus acquires the ability to infect and transmit among humans; as of July 2024 these include Aflunov, Celldemic and Seqirus/Audenz.[44][45] Some governments have prepared strategic stockpiles of vaccines against the H5N1 subtype which is considered the biggest risk.[46][47][45] However, because the influenza virus is highly variable any vaccine needs to be specifically targeted against the particular strain of virus which is causing concern. Existing influenza vaccine technologies can be adapted to a H5N1 strain causing the pandemic; in the event of an outbreak, the candidate vaccine would be rapidly tested for safety as well as efficacy against the zoonotic strain, and then authorised and distributed to vaccine manufacturers.[48][44]
Poultry - it is possible to vaccinate poultry against specific strains of HPAI influenza. Vaccination should be combined with other control measures such as infection monitoring, early detection and biosecurity.[49][50] In many countries, it is routine to vaccinate poultry against H5N1.[51] In China, the world's biggest poultry producer, there has been is a mandatory vaccination requirement since 2017; the vaccine is bivalent or trivalent, targeting the H5 and H7 subtypes of influenza A virus. It is manufactured using recombinant influenza virus.[52]
Treatment
[edit]In the event of an outbreak of human H5N1, the main antiviral drugs recommended are neuraminidase inhibitors, such as zanamivir (Relenza) and oseltamivir (Tamiflu). These drugs can reduce the severity of symptoms if taken soon after infection and can also be taken as prophylaxis to decrease the risk of infection.[53][54][55][56]
Epidemiology
[edit]History
[edit]Influenza A/H5N1 was first detected in 1959 after an outbreak of highly pathogenic avian influenza in Scotland, which infected two flocks of chickens.[57] [58]The next detection, and the earliest infection of humans by H5N1, was an epizootic (an epidemic in nonhumans) of H5N1 influenza in Hong Kong's poultry population in 1997. This outbreak was stopped by the killing of the entire domestic poultry population within the territory. Human infection was confirmed in 18 individuals who had been in close contact with poultry, 6 of whom died.[59][60]
Since then, avian A/H5N1 bird flu has become widespread in wild birds worldwide, with numerous outbreaks among both domestic and wild birds. An estimated half a billion farmed birds have been slaughtered in efforts to contain the virus.[61][62]
Pandemic potential
[edit]Influenza viruses have a relatively high mutation rate that is characteristic of RNA viruses.[63] The segmentation of the influenza A virus genome facilitates genetic recombination by segment reassortment in hosts who become infected with two different strains of influenza viruses at the same time.[64][65] With reassortment between strains, an avian strain which does not affect humans may acquire characteristics from a different strain which enable it to infect and pass between humans - a zoonotic event.[66]
As of June 2024, there is concern about two subtypes of avian influenza which are circulating in wild bird populations worldwide, A/H5N1 and A/H7N9. Both of these have potential to devastate poultry stocks, and both have jumped to humans with relatively high case fatality rates.[67] A/H5N1 in particular has infected a wide range of mammals and may be adapting to mammalian hosts.[68]
Surveillance
[edit]The Global Influenza Surveillance and Response System (GISRS) is a global network of laboratories that monitor the spread of influenza with the aim to provide the World Health Organization with influenza control information and to inform vaccine development.[69] Several millions of specimens are tested by the GISRS network annually through a network of laboratories in 127 countries. GISRS monitors avian, swine, and other potentially zoonotic influenza viruses as well as human viruses.[70]
Transmission and prevention
[edit]
Birds - Influenza A viruses of various subtypes have a large reservoir in wild waterfowl, which can infect the respiratory and gastrointestinal tract without affecting the health of the host. They can then be carried by the bird over large distances especially during annual migration. Infected birds can shed avian influenza A viruses in their saliva, nasal secretions, and feces; susceptible birds become infected when they have contact with the virus as it is shed by infected birds.[72] The virus can survive for long periods in water and at low temperatures, and can be spread from one farm to another on farm equipment.[73] Domesticated birds (chickens, turkeys, ducks, etc.) may become infected with avian influenza A viruses through direct contact with infected waterfowl or other infected poultry, or through contact with contaminated feces or surfaces.
Avian influenza outbreaks in domesticated birds are of concern for several reasons. There is potential for low pathogenic avian influenza viruses (LPAI) to evolve into strains which are high pathogenic to poultry (HPAI), and subsequent potential for significant illness and death among poultry during outbreaks. Because of this, international regulations state that any detection of H5 or H7 subtypes (regardless of their pathogenicity) must be notified to the appropriate authority.[74][75] It is also possible that avian influenza viruses could be transmitted to humans and other animals which have been exposed to infected birds, causing infection with unpredictable but sometimes fatal consequences.
When an HPAI infection is detected in poultry, it is normal to cull infected animals and those nearby in an effort to rapidly contain, control and eradicate the disease. This is done together with movement restrictions, improved hygiene and biosecurity, and enhanced surveillance. [73]
Humans - Avian flu viruses, both HPAI and LPAI, can infect humans who are in close, unprotected contact with infected poultry. Incidents of cross-species transmission are rare, with symptoms ranging in severity from no symptoms or mild illness, to severe disease that resulted in death.[76][75] As of February, 2024 there have been very few instances of human-to-human transmission, and each outbreak has been limited to a few people.[77] All subtypes of avian Influenza A have potential to cross the species barrier, with H5N1 and H7N9 considered the biggest threats.[78][79]
In order to avoid infection, the general public are advised to avoid contact with sick birds or potentially contaminated material such as carcasses or feces. People working with birds, such as conservationists or poultry workers, are advised to wear appropriate personal protection equipment.[80]
Other animals - a wide range of other animals have been affected by avian flu, generally due to eating birds which had been infected.[81] There have been instances where transmission of the disease between mammals, including seals and cows, may have occurred.[82][83]
Mortality
[edit]| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | Total | ||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
cases |
deaths |
CFR
|
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8 | 5 | 62.5% | 8 | 5 | 62.5% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 2 | 0 | 0% | 3 | 0 | 0% | 1 | 1 | 100% | 1 | 0 | 0% | 8 | 1 | 12.5% | |||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 | 4 | 100% | 2 | 2 | 100% | 1 | 1 | 100% | 1 | 0 | 0% | 1 | 0 | 0% | 1 | 1 | 100% | 8 | 8 | 100% | 3 | 3 | 100% | 26 | 14 | 53.8% | 9 | 4 | 44.4% | 6 | 4 | 66.7% | 10 | 2 | 20.0% | 72 | 43 | 59.7% | ||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 8 | 5 | 62.5% | 13 | 8 | 61.5% | 5 | 3 | 60.0% | 4 | 4 | 100% | 7 | 4 | 57.1% | 2 | 1 | 50.0% | 1 | 1 | 100% | 2 | 1 | 50.0% | 2 | 2 | 100% | 2 | 0 | 0% | 6 | 1 | 16.7% | 1 | 1 | 100% | 1 | 0 | 0% | 55 | 32 | 58.2% | ||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 18 | 10 | 55.6% | 25 | 9 | 36.0% | 8 | 4 | 50.0% | 39 | 4 | 10.3% | 29 | 13 | 44.8% | 39 | 15 | 38.5% | 11 | 5 | 45.5% | 4 | 3 | 75.0% | 37 | 14 | 37.8% | 136 | 39 | 28.7% | 10 | 3 | 30.0% | 3 | 1 | 33.3% | 359 | 120 | 33.4% | ||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 20 | 13 | 65.0% | 55 | 45 | 81.8% | 42 | 37 | 88.1% | 24 | 20 | 83.3% | 21 | 19 | 90.5% | 9 | 7 | 77.8% | 12 | 10 | 83.3% | 9 | 9 | 100% | 3 | 3 | 100% | 2 | 2 | 100% | 2 | 2 | 100% | 1 | 1 | 100% | 200 | 168 | 84.0% | ||||||||||||||||||||||||||||||
| 3 | 2 | 66.6% | 3 | 2 | 66.6% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 | 2 | 100% | 1 | 0 | 0% | 3 | 2 | 66.7% | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 1 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 1 | 100% | 1 | 1 | 100% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 | 1 | 33.3% | 3 | 1 | 33.3% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 | 0 | 0% | 2 | 0 | 0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 17 | 12 | 70.6% | 5 | 2 | 40.0% | 3 | 3 | 100% | 25 | 17 | 68.0% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12 | 4 | 33.3% | 12 | 4 | 33.3% | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 4 | 0 | 0% | 5 | 0 | 0% | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 | 0 | 0% | 46 | 0 | 0% | 47 | 0 | 0% | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 | 3 | 100% | 29 | 20 | 69.0% | 61 | 19 | 31.1% | 8 | 5 | 62.5% | 6 | 5 | 83.3% | 5 | 5 | 100% | 7 | 2 | 28.6% | 4 | 2 | 50.0% | 2 | 1 | 50.0% | 2 | 2 | 100% | 1 | 0 | 0% | 1 | 1 | 100% | 129 | 65 | 50.0% | ||||||||||||||||||||||||||||||
| 4 | 4 | 100% | 46 | 32 | 69.6% | 98 | 43 | 43.9% | 115 | 79 | 68.7% | 88 | 59 | 67.0% | 44 | 33 | 75.0% | 73 | 32 | 43.8% | 48 | 24 | 50.0% | 62 | 34 | 54.8% | 32 | 20 | 62.5% | 39 | 25 | 64.1% | 52 | 22 | 42.3% | 145 | 42 | 29.0% | 10 | 3 | 30.0% | 4 | 2 | 50.0% | 0 | 0 | 0% | 1 | 1 | 100% | 1 | 0 | 0% | 2 | 1 | 50.0% | 6 | 1 | 16.7% | 12 | 4 | 33.3% | 58 | 3 | 5.17% | 940 | 464 | 49.4% |
Outbreaks
[edit]1959–1997
[edit]- A highly pathogenic strain of H5N1 caused flu outbreaks in 1959 in Scotland in chickens.[84]
- In 1997, in Hong Kong, 18 humans were infected and 6 died in the first known case of H5N1 infecting humans.[85] Subsequently 1.3 million chickens were culled in the territory of Hong Kong. The government also suspended the import of chickens from mainland China.[86]
2003
[edit]- In 2003 the first cases in humans since 1997 were diagnosed. Three people in one family were infected after visiting Fujian province in mainland China and 2 died.[87][88]
- By midyear of 2003 outbreaks of poultry disease caused by H5N1 occurred in Asia, but were not recognized as such. In December animals in a Thai zoo died after eating infected chicken carcasses. Later that month H5N1 infection was detected in 3 flocks in the Republic of Korea.[89]
2004
[edit]- In January 2004 a major new outbreak of H5N1 surfaced in Vietnam and Thailand's poultry industry, and within weeks spread to ten countries and regions in Asia, including Indonesia, South Korea, Japan and China.[citation needed]
- Variants have been found in a number of domestic cats, leopards, and tigers in Thailand, with high lethality.[90] "The Thailand Zoo tiger outbreak killed more than 140 tigers, causing health officials to make the decision to cull all the sick tigers in an effort to stop the zoo from becoming a reservoir for H5N1 influenza.[91]
2005
[edit]- In January 2005 an outbreak of avian influenza affected thirty three out of sixty four cities and provinces in Vietnam, leading to the forced killing of nearly 1.2 million poultry.[citation needed]
- In April 2005 there begins an unprecedented die-off of over 6,000 migratory birds at Qinghai Lake in central China over three months. Later in the year H5N1 was detected in Kazakhstan, Mongolia and Russia, Turkey, Romania, Croatia and Kuwait.[citation needed]
- H5N1 was found to be infecting pigs in Indonesia, but without causing symptoms.[92]
2006
[edit]- In the first two months of 2006 H5N1 spread to India, north Africa, and Europe in wild bird populations.[citation needed]
2007
[edit]- Significant outbreaks recorded in Japan, Hungary, Russia, United Kingdom, Pakistan, Turkey, Afghanistan, Myanmar, Bangladesh, Saudi Arabia, Ghana, Malaysia, Germany, Czech Republic, Togo, France and India.[citation needed]
2008 to 2019
[edit]Many more outbreaks are recorded, in almost every country in the world, affecting both wild birds and poultry, with occasional spillover events infecting humans.[13][58][59]
2020–2024
[edit]Since 2020, outbreaks of avian influenza subtype H5N1 have been occurring, with cases reported from every continent except Australia as of November 2024.[94][95][96][97] Some species of wild aquatic birds act as natural asymptomatic carriers of a large variety of influenza A viruses, which can infect poultry, other bird species, mammals and humans if they come into close contact with infected feces or contaminated material, or by eating infected birds.[98] In late 2023, H5N1 was discovered in the Antarctic for the first time, raising fears of imminent spread throughout the region, potentially leading to a "catastrophic breeding failure" among animals that had not previously been exposed to avian influenza viruses.[99] The main virus involved in the global outbreak is classified as H5N1 clade 2.3.4.4b, however genetic diversification with other clades such as 2.3.2.1c has seen the virus evolve in ability to cause significant outbreaks in a broader range of species including mammals.[100][101][102]
H5N6 and H5N8 viruses with the H5-2.3.4.4b hemagglutinin (HA) gene became prominent globally in 2018–2020.[101][103] In 2020, reassortment (genetic "swapping") between these H5-2.3.4.4b viruses and other strains of avian influenza led to the emergence of a H5N1 strain with a H5-2.3.4.4b gene.[101] The virus then spread across Europe, detected there in autumn, before spreading to Africa and Asia.[94] It continues to swap genes with local flu viruses as it travels the globe.[104]: (fig.1)Mammalian infections
[edit]In October 2022 an outbreak of H5N1 on a Spanish mink farm showed evidence of being the first recorded case of mammal-to-mammal transmission, with 4 percent of the farm's mink population dying from H5N1-related haemorrhagic pneumonia. This coincided with H5N1 detections in the area among gulls and other seabirds, which are the presumed source of the outbreak.[105][106]
A mass Caspian seal die-off in December 2022, with 700 infected seals found dead along the Caspian Sea coastline of Russia's Dagestan republic, worried researchers regarding the possibility that wild mammal-to-mammal spread had begun.[107] A similar mass die-off of 95% of southern elephant seal pups in 2023 also raised concerns of mammal-to-mammal spread, as nursing pups would have had less exposure to birds.[108] Between January and October 2023, at least 24,000 South American sea lions died from H5N1 flu, with the outbreak starting on the Pacific coast of Peru, moving down the coast to Chile and then up the Atlantic coast of Argentina.[109]
In April 2024, spread of H5N1 amongst dairy cow herds in nine states of the USA strongly indicated the presence of cow-to-cow transmission possibly occurring while the animals were being milked.[110][111] Although mortality in bovines infected with H5N1 is rare, viable virus can be shed in the milk.[110] Around 50% of cats that lived on the affected dairy farms and were fed unpasteurised milk from symptomatic cows died within a few days from severe systemic influenza infection, raising significant concerns of cross-species mammal-to-mammal transmission.[112]
Research
[edit]H5N1 transmission studies in ferrets (2011)
[edit]Novel, contagious strains of H5N1 were created by Ron Fouchier of the Erasmus Medical Center in Rotterdam, the Netherlands, who first presented his work to the public at an influenza conference in Malta in September 2011. Three mutations were introduced into the H5N1 virus genome, and the virus was then passed from the noses of infected ferrets to the noses of uninfected ones, which was repeated 10 times.[113] After these 10 passages the H5N1 virus had acquired the ability of transmission between ferrets via aerosols or respiratory droplets.
After Fouchier offered an article describing this work to the leading academic journal Science, the US National Science Advisory Board for Biosecurity (NSABB) recommended against publication of the full details of the study, and the one submitted to Nature by Yoshihiro Kawaoka of the University of Wisconsin describing related work. However, after additional consultations at the World Health Organization and by the NSABB, the NSABB reversed its position and recommended publication of revised versions of the two papers.[114] However, then the Dutch government declared that this type of manuscripts required Fouchier to apply for an export permit in the light of EU directive 428/2009 on dual use goods.[note 1] After much controversy surrounding the publishing of his research, Fouchier complied (under formal protest) with Dutch government demands to obtain a special permit[115] for submitting his manuscript, and his research appeared in a special issue of the journal Science devoted to H5N1.[116][117][118] The papers by Fouchier and Kawaoka conclude that it is entirely possible that a natural chain of mutations could lead to an H5N1 virus acquiring the capability of airborne transmission between mammals, and that a H5N1 influenza pandemic would not be impossible.[119]
In May 2013, it was reported that scientists at the Harbin Veterinary Research Institute in Harbin, China, had created H5N1 strains which passed between guinea pigs.[120]
In response to Fouchier and Kawaoka's work, a number of scientists expressed concerns with the risks of creating novel potential pandemic pathogens, culminating in the formation of the Cambridge Working Group, a consensus statement calling for an assessment of the risks and benefits of such research.[121][122]
See also
[edit]- Antigenic shift
- Avian influenza virus
- Favipiravir
- Fujian flu
- H5N1 clinical trials
- H7N9
- Influenzavirus A
- International Conference on Emerging Infectious Diseases
- National Influenza Centers
- Swine influenza
- Zoonosis
Notes
[edit]- ^ The World Intellectual Property Organization (WIPO) lists strategic goods with prohibited goods or goods that require a special permit for import and export without which the carrier faces pecuniary punishment or up to 5 years' imprisonment.
References
[edit]Citations
[edit]- ^ "Influenza (Avian and other zoonotic)". who.int. World Health Organization. 3 October 2023. Retrieved 2024-05-06.
- ^ a b Bourk, India (26 April 2024). "'Unprecedented': How bird flu became an animal pandemic". bbc.com. BBC. Retrieved 2024-05-08.
- ^ a b c "Prevention and Antiviral Treatment of Bird Flu Viruses in People | Avian Influenza (Flu)". cdc.gov. US: Centers for Disease Control. 2024-04-19. Retrieved 2024-05-08.
- ^ "Bird flu (avian influenza)". betterhealth.vic.gov.au. Victoria, Australia: Department of Health & Human Services. Retrieved 2024-05-09.
- ^ a b "Avian influenza: guidance, data and analysis". gov.uk. 2021-11-18. Retrieved 2024-05-09.
- ^ a b "Avian Influenza in Birds". cdc.gov. US: Centers for Disease Control and Prevention. 2022-06-14. Retrieved 2024-05-06.
- ^ "Bird flu (avian influenza): how to spot and report it in poultry or other captive birds". gov.uk. UK: Department for Environment, Food & Rural Affairs and Animal and Plant Health Agency. 2022-12-13. Retrieved 2024-05-06.
- ^ "Influenza Type A Viruses". cdc.gov. US: Centers for Disease Control and Prevention. 2024-02-01. Retrieved 2024-05-03.
- ^ "Avian influenza A(H5N1) virus". www.who.int. Retrieved 2024-05-28.
- ^ a b Li FC, Choi BC, Sly T, Pak AW (June 2008). "Finding the real case-fatality rate of H5N1 avian influenza". J Epidemiol Community Health. 62 (6): 555–9. doi:10.1136/jech.2007.064030. PMID 18477756. S2CID 34200426.
- ^ "Emergence and Evolution of H5N1 Bird Flu | Avian Influenza (Flu)". cdc.gov. US: Centers for Disease Control and Prevention. 2023-06-06. Retrieved 2024-05-03.
- ^ Huang, Pan; Sun, Lujia; Li, Jinhao; et al. (2023-06-16). "Potential cross-species transmission of highly pathogenic avian influenza H5 subtype (HPAI H5) viruses to humans calls for the development of H5-specific and universal influenza vaccines". Cell Discovery. 9 (1): 58. doi:10.1038/s41421-023-00571-x. ISSN 2056-5968. PMC 10275984. PMID 37328456.
- ^ a b "Highlights in the History of Avian Influenza (Bird Flu) Timeline – 2020-2024 | Avian Influenza (Flu)". cdc.gov. US: Centers for Disease Control and Prevention. 2024-04-22. Retrieved 2024-05-08.
- ^ Caliendo, V.; Lewis, N. S.; Pohlmann, A.; et al. (2022-07-11). "Transatlantic spread of highly pathogenic avian influenza H5N1 by wild birds from Europe to North America in 2021". Scientific Reports. 12 (1): 11729. Bibcode:2022NatSR..1211729C. doi:10.1038/s41598-022-13447-z. ISSN 2045-2322. PMC 9276711. PMID 35821511.
- ^ "Bird flu is bad for poultry and cattle. Why it's not a dire threat for most of us — yet". NBC News. 2024-05-02. Retrieved 2024-05-09.
- ^ McKie, Robin (2024-04-20). "Next pandemic likely to be caused by flu virus, scientists warn". The Observer. ISSN 0029-7712. Retrieved 2024-05-09.
- ^ "Vaccination of poultry against highly pathogenic avian influenza – Available vaccines and vaccination strategies". efsa.europa.eu. 2023-10-10. Retrieved 2024-05-09.
- ^ "Two possible bird flu vaccines could be available within weeks, if needed". NBC News. 2024-05-01. Retrieved 2024-05-09.
- ^ "Avian influenza (bird flu) | European Medicines Agency". ema.europa.eu. Retrieved 2024-05-09.
- ^ "Bird flu (avian influenza): how to spot and report it in poultry or other captive birds". Department for Environment, Food & Rural Affairs and Animal and Plant Health Agency. 2022-12-13. Retrieved 2024-05-06.
- ^ "Avian flu". The Royal Society for the Protection of Birds (RSPB). Retrieved 2024-06-25.
- ^ CDC (2024-05-30). "Avian Influenza A Virus Infections in Humans". Centers for Disease Control and Prevention. Retrieved 2024-06-11.
- ^ "Questions and Answers on Avian Influenza". An official website of the European Commission. 11 June 2024. Retrieved 2024-06-11.
- ^ "Reported Human Infections with Avian Influenza A Viruses | Avian Influenza (Flu)". Centers for Disease Control and Prevention. 2024-02-01. Retrieved 2024-06-11.
- ^ "Zoonotic influenza". Wordl Health Organization. Retrieved 2024-06-16.
- ^ "The next pandemic: H5N1 and H7N9 influenza?". Gavi, the Vaccine Alliance. Retrieved 2024-06-16.
- ^ "Highly Pathogenic Avian Influenza A(H5N1) Virus in Animals: Interim Recommendations for Prevention, Monitoring, and Public Health Investigations". Centers for Disease Control. 2024-06-05. Retrieved 2024-06-13.
- ^ Bertram S, Glowacka I, Steffen I, et al. (September 2010). "Novel insights into proteolytic cleavage of influenza virus hemagglutinin". Reviews in Medical Virology. 20 (5): 298–310. doi:10.1002/rmv.657. PMC 7169116. PMID 20629046.
The influenza virus HA binds to alpha 2–3 linked (avian viruses) or alpha 2–6 linked (human viruses) sialic acids presented by proteins or lipids on the host cell surface.
- ^ Shinya K, Ebina M, Yamada S, et al. (March 2006). "Avian flu: influenza virus receptors in the human airway". Nature. 440 (7083): 435–436. Bibcode:2006Natur.440..435S. doi:10.1038/440435a. PMID 16554799. S2CID 9472264.
- ^ van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, Kuiken T (2006). "H5N1 Virus Attachment to Lower Respiratory Tract". Science. 312 (5772): 399. doi:10.1126/science.1125548. PMID 16556800. S2CID 33294327.
- ^ Bennett, Nicholas John (13 October 2021). "Avian Influenza (Bird Flu): Background, Pathophysiology, Epidemiology". Medscape Reference. Retrieved 28 April 2024.
Avian influenza is still primarily a respiratory infection but involves more of the lower airways than human influenza typically does. This is likely due to differences in the hemagglutinin protein and the types of sialic acid residues to which the protein binds. Avian viruses tend to prefer sialic acid alpha(2-3) galactose, which, in humans, is found in the terminal bronchi and alveoli. Conversely, human viruses prefer sialic acid alpha(2-6) galactose, which is found on epithelial cells in the upper respiratory tract.
- ^ "Avian influenza A(H5N1) virus". www.who.int. Retrieved 2024-05-28.
- ^ "A revision of the system of nomenclature for influenza viruses: a WHO Memorandum". Bull World Health Organ. 58 (4): 585–591. 1980. PMC 2395936. PMID 6969132.
This Memorandum was drafted by the signatories listed on page 590 on the occasion of a meeting held in Geneva in February 1980.
- ^ Payungporn S, Chutinimitkul S, Chaisingh A, Damrongwantanapokin S, Nuansrichay B, Pinyochon W, Amonsin A, Donis RO, Theamboonlers A, Poovorawan T (2006). "Discrimination between Highly Pathogenic and Low Pathogenic H5 Avian Influenza A Viruses". Emerging Infectious Diseases. 12 (4): 700–701. doi:10.3201/eid1204.051427. PMC 3294708. PMID 16715581.
- ^ "Influenza A Subtypes and the Species Affected | Seasonal Influenza (Flu) | CDC". Centers for Disease Control and Prevention. 2024-05-13. Retrieved 2024-06-17.
- ^ CDC (2024-02-01). "Influenza Type A Viruses". Centers for Disease Control and Prevention. Retrieved 2024-05-03.
- ^ CDC (2023-03-30). "Types of Influenza Viruses". Centers for Disease Control and Prevention. Retrieved 2024-06-17.
- ^ CDC (2024-06-11). "Avian Influenza Type A Viruses". Avian Influenza (Bird Flu). Retrieved 2024-06-17.
- ^ Márquez Domínguez L, Márquez Matla K, Reyes Leyva J, Vallejo Ruíz V, Santos López G (December 2023). "Antiviral resistance in influenza viruses". Cellular and Molecular Biology (Noisy-le-Grand, France). 69 (13): 16–23. doi:10.14715/cmb/2023.69.13.3. PMID 38158694.
- ^ Kou Z, Lei FM, Yu J, Fan ZJ, Yin ZH, Jia CX, Xiong KJ, Sun YH, Zhang XW, Wu XM, Gao XB, Li TX (2005). "New Genotype of Avian Influenza H5N1 Viruses Isolated from Tree Sparrows in China". J. Virol. 79 (24): 15460–15466. doi:10.1128/JVI.79.24.15460-15466.2005. PMC 1316012. PMID 16306617.
- ^ The World Health Organization Global Influenza Program Surveillance Network. (2005). "Evolution of H5N1 avian influenza viruses in Asia". Emerging Infectious Diseases. 11 (10): 1515–1521. doi:10.3201/eid1110.050644. PMC 3366754. PMID 16318689.
Figure 1 shows a diagramatic representation of the genetic relatedness of Asian H5N1 hemagglutinin genes from various isolates of the virus - ^ Shao, Wenhan; Li, Xinxin; Goraya, Mohsan Ullah; Wang, Song; Chen, Ji-Long (2017-08-07). "Evolution of Influenza A Virus by Mutation and Re-Assortment". International Journal of Molecular Sciences. 18 (8): 1650. doi:10.3390/ijms18081650. ISSN 1422-0067. PMC 5578040. PMID 28783091.
- ^ Eisfeld AJ, Neumann G, Kawaoka Y (January 2015). "At the centre: influenza A virus ribonucleoproteins". Nature Reviews. Microbiology. 13 (1): 28–41. doi:10.1038/nrmicro3367. PMC 5619696. PMID 25417656.
- ^ a b "Vaccines for pandemic influenza". European Medicines Agency. Retrieved 30 July 2024.
- ^ a b "Audenz". U.S. Food and Drug Administration (FDA). January 31, 2020. STN: 125692. Archived from the original on August 6, 2020. Retrieved February 5, 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Vaccines for pandemic influenza". European Medicines Agency. Retrieved 2024-06-15.
- ^ Keown A (February 4, 2020). "FDA Approves Seqirus' Audenz as Vaccine Against Potential Flu Pandemic". BioSpace. Archived from the original on February 5, 2020. Retrieved February 5, 2020.
- ^ "Making a Candidate Vaccine Virus (CVV) for a HPAI (Bird Flu) Virus". U.S. Centers for Disease Control and Prevention (CDC). 2024-06-03. Retrieved 2024-06-22.
- ^ "Vaccination of poultry against highly pathogenic avian influenza – Available vaccines and vaccination strategies". efsa.europa.eu. 2023-10-10. Retrieved 2024-05-09.
- ^ "Making a Candidate Vaccine Virus (CVV) for a HPAI (Bird Flu) Virus". U.S. Centers for Disease Control and Prevention (CDC). 2024-06-03. Retrieved 2024-06-15.
- ^ "Bird flu vaccination policies by country". Reuters. 17 February 2023. Retrieved 30 July 2024.
- ^ Wu, Jie; Ke, Changwen; Lau, Eric H.Y.; Song, Yingchao; Cheng, Kit Ling; Zou, Lirong; Kang, Min; Song, Tie; Peiris, Malik; Yen, Hui-Ling (January 2019). "Influenza H5/H7 Virus Vaccination in Poultry and Reduction of Zoonotic Infections, Guangdong Province, China, 2017–18". Emerging Infectious Diseases. 25 (1): 116–118. doi:10.3201/eid2501.181259. ISSN 1080-6040. PMC 6302570. PMID 30355435.
- ^ Peteranderl C, Herold S, Schmoldt C (August 2016). "Human Influenza Virus Infections". Seminars in Respiratory and Critical Care Medicine. 37 (4): 487–500. doi:10.1055/s-0036-1584801. PMC 7174870. PMID 27486731.
- ^ "Bird flu". National Health Service (NHS) UK. 2017-10-19. Retrieved 2024-07-30.
- ^ CDC (2024-07-29). "Avian Influenza (Bird Flu) - Emergency Use Instructions (EUI) for Oseltamivir". Centers for Disease Control and Prevention. Retrieved 2024-07-30.
- ^ Stiver, Grant (2003). "The treatment of influenza with antiviral drugs". Canadian Medical Association Journal. 168 (1): 49–57. PMC 139319. PMID 12515786 – via Pub Med.
- ^ Charostad, Javad; Rezaei Zadeh Rukerd, Mohammad; Mahmoudvand, Shahab; Bashash, Davood; Hashemi, Seyed Mohammad Ali; Nakhaie, Mohsen; Zandi, Keivan (September 2023). "A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep". Travel Medicine and Infectious Disease. 55: 102638. doi:10.1016/j.tmaid.2023.102638. ISSN 1477-8939. PMID 37652253.
- ^ a b CDC (2024-06-10). "1880-1959 Highlights in the History of Avian Influenza (Bird Flu) Timeline". Avian Influenza (Bird Flu). Retrieved 2024-07-08.
- ^ a b CDC (2024-06-10). "1960-1999 Highlights in the History of Avian Influenza (Bird Flu) Timeline". Avian Influenza (Bird Flu). Retrieved 2024-07-08.
- ^ Chan, Paul K. S. (2002-05-01). "Outbreak of Avian Influenza A(H5N1) Virus Infection in Hong Kong in 1997". Clinical Infectious Diseases. 34 (Supplement_2): S58–S64. doi:10.1086/338820. ISSN 1537-6591. PMID 11938498.
- ^ Bourk, India (26 April 2024). "'Unprecedented': How bird flu became an animal pandemic". www.bbc.com. Retrieved 2024-05-08.
- ^ CDC (2024-07-05). "H5N1 Bird Flu: Current Situation". Avian Influenza (Bird Flu). Retrieved 2024-07-08.
- ^ Sanjuán R, Nebot MR, Chirico N, Mansky LM, Belshaw R (October 2010). "Viral mutation rates". Journal of Virology. 84 (19): 9733–48. doi:10.1128/JVI.00694-10. PMC 2937809. PMID 20660197.
- ^ Kou Z, Lei FM, Yu J, Fan ZJ, Yin ZH, Jia CX, Xiong KJ, Sun YH, Zhang XW, Wu XM, Gao XB, Li TX (2005). "New Genotype of Avian Influenza H5N1 Viruses Isolated from Tree Sparrows in China". J. Virol. 79 (24): 15460–15466. doi:10.1128/JVI.79.24.15460-15466.2005. PMC 1316012. PMID 16306617.
- ^ The World Health Organization Global Influenza Program Surveillance Network. (2005). "Evolution of H5N1 avian influenza viruses in Asia". Emerging Infectious Diseases. 11 (10): 1515–1521. doi:10.3201/eid1110.050644. PMC 3366754. PMID 16318689. Figure 1 shows a diagramatic representation of the genetic relatedness of Asian H5N1 hemagglutinin genes from various isolates of the virus
- ^ CDC (2024-05-15). "Transmission of Bird Flu Viruses Between Animals and People". Centers for Disease Control and Prevention. Retrieved 2024-06-10.
- ^ "Global AIV with Zoonotic Potential". The Food and Agriculture Organization (FAO) of the United Nations. 29 July 2020. Retrieved 2024-06-24.
- ^ Plaza, Pablo I.; Gamarra-Toledo, Víctor; Euguí, Juan Rodríguez; Lambertucci, Sergio A. (2024). "Recent Changes in Patterns of Mammal Infection with Highly Pathogenic Avian Influenza A(H5N1) Virus Worldwide". Emerging Infectious Diseases. 30 (3): 444–452. doi:10.3201/eid3003.231098. PMC 10902543. PMID 38407173.
- ^ Lee, Kelley; Fang, Jennifer (2013). Historical Dictionary of the World Health Organization. Rowman & Littlefield. ISBN 9780810878587.
- ^ "70 years of GISRS – the Global Influenza Surveillance & Response System". World Health Organization. 19 September 2022. Retrieved 2024-06-13.
- ^ Thompson, Des; Byrkjedal, Ingvar (2001). Shorebirds. Colin Baxter Photography Ltd. ISBN 978-1841070759.
- ^ "Transmission of Bird Flu Viruses Between Animals and People". U.S. Centers for Disease Control and Prevention (CDC). 2024-05-15. Retrieved 2024-06-10.
- ^ a b "Avian Influenza". WOAH - World Organisation for Animal Health. Retrieved 2024-06-10.
- ^ "Prevention and Control of H5 and H7 Avian Influenza in the Live Bird Marketing System". United States Department of Agriculture. August 2020. Retrieved 15 June 2024.
- ^ a b "Questions and Answers on Avian Influenza". An official website of the European Commission. 11 June 2024. Retrieved 2024-06-11.
- ^ "Avian Influenza A Virus Infections in Humans". U.S. Centers for Disease Control and Prevention (CDC). 2024-05-30. Retrieved 2024-06-11.
- ^ "Reported Human Infections with Avian Influenza A Viruses". Centers for Disease Control and Prevention. 2024-02-01. Retrieved 2024-06-11.
- ^ "Zoonotic influenza". Wordl Health Organization. Retrieved 2024-06-16.
- ^ "The next pandemic: H5N1 and H7N9 influenza?". Gavi, the Vaccine Alliance. Retrieved 2024-06-16.
- ^ "Highly Pathogenic Avian Influenza A(H5N1) Virus in Animals: Interim Recommendations for Prevention, Monitoring, and Public Health Investigations". U.S. Centers for Disease Control and Prevention. 2024-06-05. Retrieved 2024-06-13.
- ^ "Bird flu 'spills over' to otters and foxes in UK". BBC News. 2023-02-02. Retrieved 2024-06-11.
- ^ "Study of H5N1 avian flu seal deaths reveals multiple lineages". Center for Infectious Disease Research and Policy. 2023-03-15. Retrieved 2024-06-13.
- ^ Kozlov M (June 2024). "Huge amounts of bird-flu virus found in raw milk of infected cows". Nature. doi:10.1038/d41586-024-01624-1. PMID 38840011.
- ^ Charostad, Javad; Rezaei Zadeh Rukerd, Mohammad; Mahmoudvand, Shahab; Bashash, Davood; Hashemi, Seyed Mohammad Ali; Nakhaie, Mohsen; Zandi, Keivan (2023-09-01). "A comprehensive review of highly pathogenic avian influenza (HPAI) H5N1: An imminent threat at doorstep". Travel Medicine and Infectious Disease. 55: 102638. doi:10.1016/j.tmaid.2023.102638. ISSN 1477-8939.
- ^ WHO (October 28, 2005). "H5N1 avian influenza: timeline" (PDF). Archived from the original (PDF) on November 29, 2005.
- ^ "香港禽流感大事记". Archived from the original on October 7, 2008. Retrieved June 12, 2008.
- ^ J.S. Peiris; W.C Yu; C.W. Leung; C.Y. Cheung; W.F. Ng; J.M. Nicholls; T.K. Ng; K.H. Chan; S.T. Lai; W.L. Lim; K.Y. Yuen; Y. Guan (February 21, 2004). "Re-emergence of fatal human influenza A subtype H5N1 disease". Lancet. 363 (9409): 617–9. doi:10.1016/S0140-6736(04)15595-5. PMC 7112424. PMID 14987888.
- ^ "Emergence and Evolution of H5N1 Bird Flu | Avian Influenza (Flu)". Centers for Disease Control and Prevention. 6 June 2023. Archived from the original on 7 March 2024. Retrieved 10 March 2024.
- ^ WHO. "Confirmed Human Cases of Avian Influenza A(H5N1)". Archived from the original on April 23, 2006.
- ^ T. Tiensin; P. Chaitaweesub; T. Songserm; A. Chaisingh; W. Hoonsuwan; C. Buranathai; T. Parakamawongsa; S. Premashthira; A. Amonsin; M. Gilbert; M. Nielen; A. Stegeman (November 2005). "Highly pathogenic avian influenza H5N1, Thailand, 2004". Emerg Infect Dis. 11 (11): 1664–72. doi:10.3201/eid1111.050608. PMC 3367332. PMID 16318716.
- ^ Henry L Niman (October 22, 2004). "Thailand: Up to 100 Tigers in Sri Racha Zoo Now Affected by Avian Influenza". Archived from the original on April 22, 2009. Retrieved February 19, 2008.
- ^ CIDRAP article Indonesian pigs have avian flu virus; bird cases double in China published May 27, 2005
- ^ "German cat gets deadly bird flu". BBC News. February 28, 2006. Retrieved October 8, 2006.
- ^ a b "Highlights in the History of Avian Influenza (Bird Flu) Timeline – 2020-2023 | Avian Influenza (Flu)". www.cdc.gov. 2023-02-24. Archived from the original on 2023-02-25. Retrieved 2023-02-24.
- ^ "A global bird flu outbreak is now so bad, many countries are considering vaccination". ABC News. 2023-02-16. Archived from the original on 2023-02-23. Retrieved 2023-02-24.
- ^ Worden-Sapper, Emma; Sawyer, Sara; Wu, Sharon (16 March 2023). "As bird flu continues to spread in the US and worldwide, what's the risk that it could start a human pandemic? 4 questions answered". The Conversation. Archived from the original on 2023-03-30. Retrieved 2023-03-30.
- ^ Docter-Loeb, Hannah. "Vaccine Makers Are Preparing for Bird Flu". Scientific American. Archived from the original on 2023-03-30. Retrieved 2023-03-30.
- ^ "Bird flu (avian influenza): how to spot and report it in poultry or other captive birds". Department for Environment, Food & Rural Affairs and Animal and Plant Health Agency. 2022-12-13. Retrieved 2024-05-06.
- ^ Weston, Phoebe (24 October 2023). "'Catastrophic': bird flu reaches Antarctic for the first time". The Guardian. Archived from the original on 29 October 2023. Retrieved 30 October 2023.
- ^ Kerlin, Katherine E. (28 February 2024). "Avian Influenza Virus Is Adapting to Spread to Marine Mammals". UC Davis. Archived from the original on 10 March 2024. Retrieved 10 March 2024.
- ^ a b c "Emergence and Evolution of H5N1 Bird Flu | Avian Influenza (Flu)". www.cdc.gov. 6 June 2023. Archived from the original on 7 March 2024. Retrieved 10 March 2024.
- ^ Schnirring, Lisa (27 April 2024). "H5N1 avian flu infects Colorado dairy cows as global experts weigh in on virus changes". University of Minnesota. CIDRAP. Archived from the original on 28 April 2024. Retrieved 28 April 2024.
- ^ Tian, Jingman; Bai, Xiaoli; Li, Minghui; Zeng, Xianying; Xu, Jia; Li, Peng; Wang, Miao; Song, Xingdong; Zhao, Zhiguo; Tian, Guobin; Liu, Liling; Guan, Yuntao; Li, Yanbing; Chen, Hualan (July 2023). "Highly Pathogenic Avian Influenza Virus (H5N1) Clade 2.3.4.4b Introduced by Wild Birds, China, 2021". Emerging Infectious Diseases. 29 (7): 1367–1375. doi:10.3201/eid2907.221149. ISSN 1080-6040. PMC 10310395. PMID 37347504.
- ^ Tian, Jingman; Bai, Xiaoli; Li, Minghui; Zeng, Xianying; Xu, Jia; Li, Peng; Wang, Miao; Song, Xingdong; Zhao, Zhiguo; Tian, Guobin; Liu, Liling; Guan, Yuntao; Li, Yanbing; Chen, Hualan (July 2023). "Highly Pathogenic Avian Influenza Virus (H5N1) Clade 2.3.4.4b Introduced by Wild Birds, China, 2021". Emerging Infectious Diseases. 29 (7): 1367–75. doi:10.3201/eid2907.221149. PMC 10310395. PMID 37347504.
- ^ Nuki, Paul (2 February 2023). "How worried should we be about avian flu?". The Telegraph. Archived from the original on 2 February 2023. Retrieved 5 February 2023.
- ^ Pelley, Lauren (2 February 2023). "Bird flu keeps spreading beyond birds. Scientists worry it signals a growing threat to humans, too". CBC News. Archived from the original on 2 February 2023. Retrieved 5 February 2023.
- ^ Merrick, Jane (1 February 2023). "Mass death of seals raises fears bird flu is jumping between mammals, threatening new pandemic". The i newspaper. Archived from the original on 3 February 2023. Retrieved 15 February 2023.
- ^ Kwan, Jacklin (22 January 2024). "Bird flu wipes out over 95% of southern elephant seal pups in 'catastrophic' mass death". livescience.com. Retrieved 23 January 2024.
- ^ Plaza, Pablo I.; Gamarra-Toledo, Víctor; Rodríguez Euguí, Juan; Rosciano, Natalia; Lambertucci, Sergio A. (2024-05-01). "Pacific and Atlantic sea lion mortality caused by highly pathogenic Avian Influenza A(H5N1) in South America". Travel Medicine and Infectious Disease. 59: 102712. doi:10.1016/j.tmaid.2024.102712. ISSN 1477-8939.
- ^ a b Kozlov, Max (2024-06-05). "Huge amounts of bird-flu virus found in raw milk of infected cows". Nature. doi:10.1038/d41586-024-01624-1. ISSN 0028-0836. PMID 38840011.
- ^ Mallapaty, Smriti (2024-04-27). "Bird flu virus has been spreading in US cows for months, RNA reveals". Nature. doi:10.1038/d41586-024-01256-5. PMID 38678111.
- ^ Burrough, Eric; Magstadt, Drew; Main, Rodger (29 April 2024). "Highly Pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b Virus Infection in Domestic Dairy Cattle and Cats, United States, 2024". Emerging Infectious Diseases. 30 (7): 1335–1343. doi:10.3201/eid3007.240508. PMC 11210653. PMID 38683888. Retrieved 30 April 2024.
- ^ Harmon, Katherine (2011-09-19). "What Will the Next Influenza Pandemic Look Like?". Scientific American. Archived from the original on 2012-03-02. Retrieved 2012-01-23.
- ^ David Malakoff (March 30, 2012). "Breaking News: NSABB Reverses Position on Flu Papers". Science Insider. Archived from the original on June 30, 2012. Retrieved June 23, 2012.
- ^ Nell Greenfieldboyce (April 24, 2012). "Bird Flu Scientist has Applied for Permit to Export Research". NPR. Archived from the original on June 22, 2012. Retrieved June 23, 2012.
- ^ Nell Greenfieldboyce (June 21, 2012). "Journal Publishes Details on Contagious Bird Flu Created in Lab". National Public Radio (NPR). Archived from the original on June 22, 2012. Retrieved June 23, 2012.
- ^ "H5N1" (Special Issue). Science. June 21, 2012. Archived from the original on June 25, 2012. Retrieved June 23, 2012.
- ^ Herfst, S.; Schrauwen, E. J. A.; Linster, M.; Chutinimitkul, S.; De Wit, E.; Munster, V. J.; Sorrell, E. M.; Bestebroer, T. M.; Burke, D. F.; Smith, D. J.; Rimmelzwaan, G. F.; Osterhaus, A. D. M. E.; Fouchier, R. A. M. (2012). "Airborne Transmission of Influenza A/H5N1 Virus Between Ferrets". Science. 336 (6088): 1534–1541. Bibcode:2012Sci...336.1534H. doi:10.1126/science.1213362. PMC 4810786. PMID 22723413.
- ^ Brown, Eryn (June 21, 2012). "Scientists create bird flu that spreads easily among mammals". Los Angeles Times. Archived from the original on June 23, 2012. Retrieved June 23, 2012.
- ^ Keim, Brandon (2013-05-02). "Chinese Scientists Create New Mutant Bird-Flu Virus". Wired. ISSN 1059-1028. Retrieved 2023-02-07.
- ^ "Scientists Resume Efforts to Create Deadly Flu Virus, with US Government's Blessing". Forbes.
- ^ "From anthrax to bird flu – the dangers of lax security in disease-control labs". TheGuardian.com. 18 July 2014.
Sources
[edit]- Analysis of the efficacy of an adjuvant-based inactivated pandemic H5N1 influenza virus vaccine. https://link.springer.com/article/10.1007%2Fs00705-019-04147-7 Ainur NurpeisovaEmail authorMarkhabat KassenovNurkuisa RametovKaissar TabynovGourapura J. RenukaradhyaYevgeniy VolginAltynay SagymbayAmanzhol MakbuzAbylay SansyzbayBerik Khairullin
Research Institute for Biological Safety Problems (RIBSP), Zhambyl Region, Republic of Kazakhstan
External links
[edit]- Influenza Research Database – Database of influenza genomic sequences and related information.
- WHO World Health Organization
- WHO's Avian Flu Facts Sheet for 2006
- Epidemic and Pandemic Alert and Response Guide to WHO's H5N1 pages
- Avian Influenza Resources (updated) – tracks human cases and deaths
- National Influenza Pandemic Plans
- WHO Collaborating Centres and Reference Laboratories Centers, names, locations, and phone numbers
- FAO Avian Influenza portal Archived 2012-01-26 at the Wayback Machine Information resources, animations, videos, photos
- FAO Food and Agriculture Organisation – Bi-weekly Avian Influenza Maps – tracks animal cases and deaths
- FAO Bird Flu disease card
- FAO Socio-Economic impact of AI Projects, Information resources
- OIE World Organisation for Animal Health – tracks animal cases and deaths
- Official outbreak reports by country Archived 2012-12-13 at the Wayback Machine
- Official outbreak reports by week
- Chart of outbreaks by country Archived 2012-04-19 at the Wayback Machine
- Health-EU Portal EU response to Avian Influenza.
- Avian influenza – Q & A's factsheet from European Centre for Disease Prevention and Control
- United Kingdom
- Exotic Animal Disease Generic Contingency Plan – DEFRA generic contingency plan for controlling and eradicating an outbreak of an exotic animal disease. PDF hosted by BBC.
- UK Influenza Pandemic Contingency Plan by the National Health Service – a government entity. PDF hosted by BBC
- UK Department of Health Archived 2009-07-09 at the Wayback Machine
- United States
- Center for Infectious Disease Research and Policy Archived 2013-06-17 at the Wayback Machine Avian Influenza (Bird Flu): Implications for Human Disease – An overview of Avian Influenza
- PandemicFlu.Gov U.S. Government's avian flu information site
- USAID U.S. Agency for International Development – Avian Influenza Response
- CDC, Centers for Disease Control and Prevention – responsible agency for avian influenza in humans in US – Facts About Avian Influenza (Bird Flu) and Avian Influenza A (H5N1) Virus
- USGS – NWHC National Wildlife Health Center – responsible agency for avian influenza in animals in US
- Wildlife Disease Information Node A part of the National Biological Information Infrastructure and partner of the NWHC, this agency collects and distributes news and information about wildlife diseases such as avian influenza and coordinates collaborative information sharing efforts.
- HHS U.S. Department of Health & Human Services's Pandemic Influenza Plan
