Guanidinoacetate methyltransferase deficiency
| Guanidinoacetate methyltransferase deficiency | |
|---|---|
| Other names | GAMT deficiency |
 | |
| Specialty | Medical genetics |
| Causes | Deficiency of guanidinoacetate methyltransferase enzyme |
| Diagnostic method | Genetic testing, magnetic resonance spectroscopy, blood and urine testing |
| Treatment | Dietary adjustment and creatine supplementation |
Guanidinoacetate methyltransferase deficiency (GAMT deficiency) is an autosomal recessive[1] cerebral creatine deficiency that primarily affects the nervous system and muscles. It is the first described disorder of creatine metabolism,[2] and results from deficient activity of guanidinoacetate methyltransferase, an enzyme involved in the synthesis of creatine.[3] Clinically, affected individuals most commonly present with developmental delay, behavior disorder, and seizures.[4] Diagnosis can be suspected on clinical findings, and confirmed by specific biochemical tests, brain magnetic resonance spectroscopy, or genetic testing.[5] Biallelic pathogenic variants in the GAMT gene are the underlying cause of the disorder. After GAMT deficiency is diagnosed, it can be treated by dietary adjustments, including supplementation with creatine.[6][7] Treatment is highly effective if started early in life.[8] If treatment is started late, it cannot reverse brain damage which has already taken place.[8] The prevalence of GAMT deficiency is estimated to be 1:250,000.[9]
Signs and symptoms
[edit]Individuals with GAMT deficiency appear normal at birth. Shortly after birth, infants may start to show signs, as the consequences of decreased creatine levels in their body become more apparent.[4] Symptoms generally begin during early infancy (3–6 months) to age two years.[4] These clinical findings are relatively non-specific and do not immediately suggest a disorder of creatine metabolism. The most consistent clinical manifestation is developmental delay or intellectual disability, which is observed in all affected individuals, and can range from mild to severe.[4] Most individuals have severe developmental delay or intellectual disability (50-75%).[4] The next most consistent symptom is a behavior disorder, such as hyperactivity, autism, or self-injurious behavior, reported in 75% of GAMT deficient individuals.[4] The third most consistent symptom is seizures, reported in more than 70% of affected individuals.[4] Additional symptoms include movement disorders, such as chorea, athetosis, dystonia or ataxia, observed in about 30% of GAMT patients.[4]

Genetics
[edit]
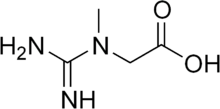
Biallelic pathogenic variants in GAMT are associated with guanidinoacetate methyltransferase deficiency. Over 70 variants have been reported in the GAMT gene.[10] This gene codes for the enzyme guanidinoacetate methyltransferase (GAMT), which participates in the two-step synthesis of the compound creatine from amino acids glycine, arginine and methionine. Specifically, GAMT controls the second step of the sequence, in which creatine is produced from another compound called guanidinoacetate.[11] GAA is toxic,[12] and because GAMT patients lack the enzyme used to convert GAA to creatine, a build-up of GAA occurs in the brain and other tissues. This accumulation of GAA is thought to cause the more severe symptoms of GATM deficiency.[8] The effects of GAMT deficiency are most severe in organs and tissues that require large amounts of energy, such as the brain and muscles.[8]
This disorder is inherited in an autosomal recessive manner, which means the causative gene is located on an autosome, and two defective copies of the gene – one from each parent – are required to inherit the disorder. The parents both carry one pathogenic variant; however, they are not affected by the disorder. As carriers, the residual activity of approximately 50% is enough to avoid clinical complications.[13] Any siblings of an GAMT deficient individual have a 25% chance of also being GAMT deficient, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier.[4]
Diagnosis
[edit]GAMT deficiency can be suspected from clinical findings, although clinical findings are not suggestive of a specific diagnosis. The initial diagnosis is typically established via measurement of creatine, creatinine, and guanidinoacetate in plasma, cerebrospinal fluid, or dried blood spots.[5] These measurements can distinguish among the different cerebral creatine deficiency disorders. In GAMT deficiency, laboratory testing of plasma will show decreased levels of creatine and increased levels of guanidinoacetate.[5] A definitive diagnosis requires DNA sequencing of the GAMT gene and/or GAMT enzymatic activity assays.[5] Brain magnetic resonance spectroscopy can also be used in diagnosis, and will show decreased levels of creatine in affected individuals.[5] However, as this finding is seen in all three cerebral creatine deficiencies, further testing is needed to identify the specific defect.[5]
Treatment is most effective for GAMT deficiency with early diagnosis; however, the non-specific clinical findings mean a diagnosis is often delayed. Due to the efficacy of early treatment and the lengthy typical diagnostic journey, GAMT deficiency has been recommended for newborn screening by the United States Advisory Committee on Heritable Disorders in Newborns and Children.[5] Newborn screening assays measure the amount of guanidinoacetate in a dried blood spot using tandem mass spectrometry. Abnormal results from a newborn screening test still need to be confirmed by testing in plasma or urine.[14]
In the United States, Utah started screening for GAMT deficiency in all newborns in 2015. New York started screening newborns in late 2018.[15] In 2020, a GAMT-positive infant was identified via newborn screening in Utah,[16] thus providing evidence that a case could be identified from newborn screening. A second infant was identified in New York in 2021.[16] In 2022, a federal advisory committee voted to include GAMT in the Recommended Universal Screening Panel starting in January 2023.[17] In addition to New York and Utah, California,[18] Pennsylvania,[19] Connecticut,[20] Delaware,[20] and Michigan[20] all currently screen for GAMT.
Around the world, the state of Victoria, Australia began screening for GAMT in 2004,[17] leading to the diagnosis of a newborn at birth in 2022.[21] In Canada, the provinces of Ontario[22] and British Columbia[23] screen for GAMT.
Treatment
[edit]Treatment of GAMT deficiency focuses on restoration of depleted brain creatine with oral creatine supplementation in pharmacologic doses, and removal of toxic intermediate GAA via ornithine supplementation and arginine- or protein-restricted diet.[24][8] Sodium benzoate supplementation is also sometimes used to decrease GAA levels.[7] All patients are reported to benefit from creatine supplementation, with possible improvements or stabilization in symptoms.[6] Seizures appear to reduce more with dietary arginine restriction and ornithine supplementation.[7] Despite treatment, none of the patients have been reported to return to completely normal developmental level, if significant damage had taken place before treatment.[8] Prior to the addition of GAMT deficiency to newborn screening panels, younger siblings of affected individuals may have been tested at birth and treated early.[24] This early treatment can result in outcomes that are very close to normal.[25]
References
[edit]- ^ Schulze, Andreas (2003). "Creatine deficiency syndromes". Molecular and Cellular Biochemistry. 244 (1/2): 143–150. doi:10.1023/A:1022443503883. ISSN 0300-8177. PMID 12701824. S2CID 25056424.
- ^ Stöckler, S.; Holzbach, U.; Hanefeld, F.; Marquardt, I.; Helms, G.; Requart, M.; Hänicke, W.; Frahm, J. (1994). "Creatine deficiency in the brain: a new, treatable inborn error of metabolism". Pediatric Research. 36 (3): 409–413. doi:10.1203/00006450-199409000-00023. ISSN 0031-3998. PMID 7808840.
- ^ Stöckler, S; Isbrandt, D; Hanefeld, F; Schmidt, B; Von Figura, K (1 May 1996). "Guanidinoacetate methyltransferase deficiency: the first inborn error of creatine metabolism in man" (Free full text). American Journal of Human Genetics. 58 (5): 914–22. ISSN 0002-9297. PMC 1914613. PMID 8651275.
- ^ a b c d e f g h i Mercimek-Andrews, Saadet; Salomons, Gajja S. (2022), Adam, Margaret P.; Feldman, Jerry; Mirzaa, Ghayda M.; Pagon, Roberta A. (eds.), "Creatine Deficiency Disorders", GeneReviews®, Seattle (WA): University of Washington, Seattle, PMID 20301745, retrieved 2024-08-27
- ^ a b c d e f g Sharer, J. Daniel; Bodamer, Olaf; Longo, Nicola; Tortorelli, Silvia; Wamelink, Mirjam M. C.; Young, Sarah (2017). "Laboratory diagnosis of creatine deficiency syndromes: a technical standard and guideline of the American College of Medical Genetics and Genomics". Genetics in Medicine. 19 (2): 256–263. doi:10.1038/gim.2016.203. ISSN 1530-0366. PMID 28055022.
- ^ a b Stockler-Ipsiroglu, Sylvia; van Karnebeek, Clara; Longo, Nicola; Korenke, G. Christoph; Mercimek-Mahmutoglu, Saadet; Marquart, Iris; Barshop, Bruce; Grolik, Christiane; Schlune, Andrea; Angle, Brad; Araújo, Helena Caldeira; Coskun, Turgay; Diogo, Luisa; Geraghty, Michael; Haliloglu, Goknur (2014-01-01). "Guanidinoacetate methyltransferase (GAMT) deficiency: Outcomes in 48 individuals and recommendations for diagnosis, treatment and monitoring". Molecular Genetics and Metabolism. 111 (1): 16–25. doi:10.1016/j.ymgme.2013.10.018. ISSN 1096-7192. PMID 24268530.
- ^ a b c Khaikin, Yannay; Sidky, Sarah; Abdenur, Jose; Anastasi, Arnaud; Ballhausen, Diana; Buoni, Sabrina; Chan, Alicia; Cheillan, David; Dorison, Nathalie; Goldenberg, Alice; Goldstein, Jennifer; Hofstede, Floris C.; Jacquemont, Marie-Line; Koeberl, Dwight D.; Lion-Francois, Laurence (16 Feb 2018). "Treatment outcome of twenty-two patients with guanidinoacetate methyltransferase deficiency: An international retrospective cohort study". European Journal of Paediatric Neurology. 22 (3): 369–379. doi:10.1016/j.ejpn.2018.02.007. ISSN 1532-2130. PMID 29506905.
- ^ a b c d e f Hanna-El-Daher, Layane; Braissant, Olivier (2016-08-01). "Creatine synthesis and exchanges between brain cells: What can be learned from human creatine deficiencies and various experimental models?". Amino Acids. 48 (8): 1877–1895. doi:10.1007/s00726-016-2189-0. ISSN 1438-2199. PMID 26861125.
- ^ Mercimek-Mahmutoglu, S.; Pop, A.; Kanhai, W.; Fernandez Ojeda, M.; Holwerda, U.; Smith, D.; Loeber, J. G.; Schielen, P. C. J. I.; Salomons, G. S. (2016-01-01). "A pilot study to estimate incidence of guanidinoacetate methyltransferase deficiency in newborns by direct sequencing of the GAMT gene". Gene. 575 (1): 127–131. doi:10.1016/j.gene.2015.08.045. ISSN 1879-0038. PMID 26319512.
- ^ Goldstein, Jennifer; Thomas-Wilson, Amanda; Groopman, Emily; Aggarwal, Vimla; Bianconi, Simona; Fernandez, Raquel; Hart, Kim; Longo, Nicola; Liang, Nicole; Reich, Daniel; Wallis, Heidi; Weaver, Meredith; Young, Sarah; Mercimek-Andrews, Saadet (May 2024). "ClinGen variant curation expert panel recommendations for classification of variants in GAMT, GATM and SLC6A8 for cerebral creatine deficiency syndromes". Molecular Genetics and Metabolism. 142 (1): 108362. doi:10.1016/j.ymgme.2024.108362. ISSN 1096-7206. PMID 38452609.
- ^ Clark, Joseph F.; Cecil, Kim M. (2014). "Diagnostic methods and recommendations for the cerebral creatine deficiency syndromes". Pediatric Research. 77 (3): 398–405. doi:10.1038/pr.2014.203. ISSN 0031-3998. PMID 25521922. S2CID 6720075.
- ^ Meera, Pratap; Uusi-Oukari, Mikko; Wallner, Martin; Lipshutz, Gerald S. (28 Jan 2023). "Guanidinoacetate ( GAA ) is a potent GABA A receptor GABA mimetic: Implications for neurological disease pathology". Journal of Neurochemistry. 165 (3): 445–454. doi:10.1111/jnc.15774. ISSN 0022-3042. PMID 36726215.
- ^ "612736 CEREBRAL CREATINE DEFICIENCY SYNDROME 2; CCDS2". Johns Hopkins University. Retrieved 2019-01-05.
- ^ Ombrone D, Giocaliere E, Forni G, Malvagia S, la Marca G (2016). "Expanded newborn screening by mass spectrometry: New tests, future perspectives" (PDF). Mass Spectrom Rev. 35 (1): 71–84. Bibcode:2016MSRv...35...71O. doi:10.1002/mas.21463. hdl:2158/1010572. PMID 25952022. S2CID 21933819. Archived from the original (PDF) on 2022-03-29. Retrieved 2019-09-02.
- ^ "Newborn Screening Program". Association for Creatine Deficiencies. Retrieved 2019-05-05.
- ^ a b Hart, Kim; Rohrwasser, Andreas; Wallis, Heidi; Golsan, Heather; Shao, Jianyin; Anderson, Taylor; Wang, Xiaoli; Szabo-Fresnais, Nicolas; Morrissey, Mark; Kay, Denise M.; Wojcik, Matthew; Galvin-Parton, Patricia A.; Longo, Nicola; Caggana, Michele; Pasquali, Marzia (2021-09-01). "Prospective identification by neonatal screening of patients with guanidinoacetate methyltransferase deficiency". Molecular Genetics and Metabolism. 134 (1): 60–64. doi:10.1016/j.ymgme.2021.07.012. ISSN 1096-7192. PMID 34389248.
- ^ a b Ream, Margie A.; Lam, Wendy K. K.; Grosse, Scott D.; Ojodu, Jelili; Jones, Elizabeth; Prosser, Lisa A.; Rose, Angela M.; Comeau, Anne Marie; Tanksley, Susan; Powell, Cynthia M.; Kemper, Alex R. (2023-08-01). "Evidence and Recommendation for Guanidinoacetate Methyltransferase Deficiency Newborn Screening". Pediatrics. 152 (2): e2023062100. doi:10.1542/peds.2023-062100. ISSN 1098-4275. PMC 10527896. PMID 37465909.
- ^ "NBS Program Disorders Detectable". www.cdph.ca.gov. Retrieved 2024-08-20.
- ^ "Pennsylvania Bulletin". www.pacodeandbulletin.gov. Retrieved 2024-10-17.
- ^ a b c Therrell, Bradford L.; Padilla, Carmencita D.; Borrajo, Gustavo J. C.; Khneisser, Issam; Schielen, Peter C. J. I.; Knight-Madden, Jennifer; Malherbe, Helen L.; Kase, Marika (2024-05-23). "Current Status of Newborn Bloodspot Screening Worldwide 2024: A Comprehensive Review of Recent Activities (2020–2023)". International Journal of Neonatal Screening. 10 (2): 38. doi:10.3390/ijns10020038. ISSN 2409-515X. PMC 11203842. PMID 38920845.
- ^ "First Baby with GAMT Deficiency Identified through Newborn Screening in Australia". EIN Presswire. June 29, 2023.
- ^ "Guanidinoacetate Methyltransferase (GAMT) Deficiency". Newborn Screening Ontario. Retrieved 2024-10-15.
- ^ "Metabolic Disorders". www.perinatalservicesbc.ca. Retrieved 2024-10-15.
- ^ a b Chen, Daphne (2016-11-02). "Utah mom, doctors push to add rare disorder to national newborn screening panel". Deseret News, Utah. Retrieved 2019-02-18.
- ^ Marten, Lara M.; Krätzner, Ralph; Salomons, Gajja S.; Fernandez Ojeda, Matilde; Dechent, Peter; Gärtner, Jutta; Huppke, Peter; Dreha-Kulaczewski, Steffi (2024-03-01). "Long term follow-up in GAMT deficiency – Correlation of therapy regimen, biochemical and in vivo brain proton MR spectroscopy data". Molecular Genetics and Metabolism Reports. 38: 101053. doi:10.1016/j.ymgmr.2024.101053. ISSN 2214-4269. PMC 10926185. PMID 38469086.
Further reading
[edit]- National Library of Medicine. MedlinePlus - Guanidinoacetate methyltransferase deficiency
- GeneReview/NIH/UW entry on Cerebral Creatine Deficiency syndromes
