Hypouricemia
| Hypouricemia | |
|---|---|
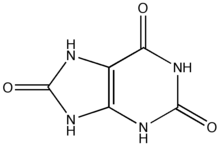 | |
| Uric acid | |
| Specialty | Endocrinology |
Hypouricemia or hypouricaemia is a level of uric acid in blood serum that is below normal. In humans, the normal range of this blood component has a lower threshold set variously in the range of 2 mg/dL to 4 mg/dL, while the upper threshold is 530 μmol/L (6 mg/dL) for women and 619 μmol/L (7 mg/dL) for men.[1] Hypouricemia usually is benign and sometimes is a sign of a medical condition.
Presentation
[edit]Complications
[edit]Although normally benign, idiopathic renal hypouricemia may increase the risk of exercise-induced acute kidney failure.[2][3][4] There is also evidence that hypouricemia can worsen conditions such as rheumatoid arthritis, especially when combined with low Vitamin C uptake, due to free radical damage.[5]
Causes
[edit]Hypouricemia is often benign and not a medical condition, but it is a useful medical sign. It is known occasionally to result in a decreased ability to concentrate urine due to decreased hypertonicity of the renal medulla, and may contribute to hypotension when other risk factors are present. Hypotonicity of the renal medulla is considered normal in the fetus and in infants due to hypouricemia caused by low protein intake. [6] Hypouricemia is usually due to drugs and toxic agents, sometimes to diet or genetics, and, rarely, suggests an underlying medical condition.[citation needed]
Medication
[edit]The majority of drugs that contribute to hypouricemia are uricosuric drugs that increase the excretion of uric acid from the blood into the urine.[7] Others include drugs that reduce the production of uric acid: xanthine oxidase inhibitors, urate oxidase (rasburicase), and sevelamer.[8]
Diet
[edit]Hypouricemia is common in vegetarians and vegans due to the low purine content of most vegetarian diets.[9] Vegetarian diet has been found to result in mean serum uric acid values as low as 239 μmol/L (2.7 mg/dL).[10] While a vegetarian diet is typically seen as beneficial with respect to conditions such as gout,[10] it may be associated with some other health conditions.[citation needed]
Transient hypouricemia sometimes is produced by total parenteral nutrition.[11] Paradoxically, total parenteral nutrition may produce hypouricemia followed shortly by acute gout, a condition normally associated with hyperuricemia.[12][13] The reasons for this are unclear.
Genetics
[edit]Two kinds of genetic mutations are known to cause hypouricemia: mutations causing xanthine oxidase deficiency, which reduces the production of uric acid; and mutations causing abnormal kidney function that increases the excretion of uric acid. Collectively known as familial renal hypouricemia, the latter mutations are of two types, involving defects of presecretory and postsecretory reabsorption.[citation needed]
A genetic mutation in Dalmatian dogs causes hypouricemia due to a kidney defect that interferes with reabsorption of uric acid. A similar mutation has been reported in a human brother and sister.[14]
In humans, loss-of-function mutations in the gene URAT1 are associated with presecretory reabsorption defects.[15][16][17]
Medical conditions
[edit]Medical conditions that can cause hypouricemia include:
- Fanconi syndrome
- Hyperthyroidism
- Multiple sclerosis[18]
- Myeloma
- Nephritis
- Wilson's disease
- Purine nucleoside phosphorylase (PNP) deficiency[19]
Diagnosis
[edit]Uric acid clearance should also be performed, increase in clearance points to proximal tubular defects in the kidney, normal or reduced clearance points to a defect in xanthine oxidase.[citation needed]
Treatment
[edit]Idiopathic hypouricemia usually requires no treatment. In some cases, hypouricemia is a medical sign of an underlying condition that does require treatment. For example, if hypouricemia reflects high excretion of uric acid into the urine (hyperuricosuria) with its risk of uric acid nephrolithiasis, the hyperuricosuria may require treatment.[20]
Drugs and dietary supplements that may be helpful
[edit]Prevalence
[edit]In one study, hypouricemia was found in 4.8% of hospitalized women and 6.5% of hospitalized men. (The definition was less than 0.14 mmol/L for women and less than 0.20 mmol/L in men.) [21]
See also
[edit]References
[edit]- ^ Chizyński K, Rózycka M (November 2005). "[Hyperuricemia]". Pol. Merkur. Lekarski (in Polish). 19 (113): 693–6. PMID 16498814.
- ^ Ito O, Hasegawa Y, Sato K, Mitsui H, Yuda F, Sato H, Ito S, Kudo K (June 2003). "A case of exercise-induced acute renal failure in a patient with idiopathic renal hypouricemia developed during antihypertensive therapy with losartan and trichlormethiazide". Hypertens. Res. 26 (6): 509–13. doi:10.1291/hypres.26.509. PMID 12862209.
- ^ Ohta T, Sakano T, Igarashi T, Itami N, Ogawa T (June 2004). "Exercise-induced acute renal failure associated with renal hypouricaemia: results of a questionnaire-based survey in Japan". Nephrol. Dial. Transplant. 19 (6): 1447–53. doi:10.1093/ndt/gfh094. PMID 15150354.
- ^ Mima A, Ichida K, Matsubara T, Kanamori H, Inui E, Tanaka M, Manabe Y, Iehara N, Tanaka Y, Yanagita M, Yoshioka A, Arai H, Kawamura M, Usami K, Hosoya T, Kita T, Fukatsu A (December 2008). "Acute Renal Failure After Exercise in a Japanese Sumo Wrestler With Renal Hypouricemia". Am. J. Med. Sci. 336 (6): 512–514. doi:10.1097/MAJ.0b013e318164717f. PMID 19092327.
- ^ Mahajan M, Kaur S, Mahajan S, Kant R (April 2009). "Uric acid a better scavenger of free radicals than vitamin C in rheumatoid arthritis". Indian Journal of Clinical Biochemistry. 24 (2): 205–207. doi:10.1007/s12291-009-0038-6. PMC 3453227. PMID 23105835.
- ^ Chevalier, Robert. "Fetal and Neonatal Physiology (Fourth Edition), 2011". Science Direct. Retrieved 7 December 2023.
- ^ Ramsdell CM, Kelley WN (February 1973). "The clinical significance of hypouricemia". Annals of Internal Medicine. 78 (2): 239–42. doi:10.7326/0003-4819-78-2-239. PMID 4683752.
- ^ Garg JP, Chasan-Taber S, Blair A, et al. (January 2005). "Effects of sevelamer and calcium-based phosphate binders on uric acid concentrations in patients undergoing hemodialysis: a randomized clinical trial". Arthritis and Rheumatism. 52 (1): 290–5. doi:10.1002/art.20781. PMID 15641045.
- ^ Siener R, Hesse A (2003). "The effect of a vegetarian and different omnivorous diets on urinary risk factors for uric acid stone formation". Eur J Nutr. 42 (6): 332–7. doi:10.1007/s00394-003-0428-0. PMID 14673606. S2CID 25531908.
- ^ a b Szeto YT, Kwok TC, Benzie IF (October 2004). "Effects of a long-term vegetarian diet on biomarkers of antioxidant status and cardiovascular disease risk". Nutrition. 20 (10): 863–6. doi:10.1016/j.nut.2004.06.006. PMID 15474873.
- ^ Koretz RL (November 1981). "Hypouricemia--a transient biochemical phenomenon of total parenteral nutrition". Am. J. Clin. Nutr. 34 (11): 2493–8. doi:10.1093/ajcn/34.11.2493. PMID 6795918.
- ^ Moyer RA, John DS (April 2003). "Acute gout precipitated by total parenteral nutrition". J. Rheumatol. 30 (4): 849–50. PMID 12672211.
- ^ Derus CL, Levinson DJ, Bowman B, Bengoa JM, Sitrin MD (October 1987). "Altered fractional excretion of uric acid during total parenteral nutrition". J. Rheumatol. 14 (5): 978–81. PMID 3123676.
- ^ Greene ML, Marcus R, Aurbach GD, Kazam ES, Seegmiller JE (September 1972). "Hypouricemia due to isolated renal tubular defect. Dalmatian dog mutation in man". Am. J. Med. 53 (3): 361–7. doi:10.1016/0002-9343(72)90181-7. PMID 5054729.
- ^ Ichida K, Hosoyamada M, Kamatani N, Kamitsuji S, Hisatome I, Shibasaki T, Hosoya T (September 2008). "Age and origin of the G774A mutation in SLC22A12 causing renal hypouricemia in Japanese". Clin. Genet. 74 (3): 243–51. doi:10.1111/j.1399-0004.2008.01021.x. PMID 18492088. S2CID 205406749.
- ^ Takahashi T, Tsuchida S, Oyamada T, Ohno T, Miyashita M, Saito S, Komatsu K, Takashina K, Takada G (May 2005). "Recurrent URAT1 gene mutations and prevalence of renal hypouricemia in Japanese". Pediatr. Nephrol. 20 (5): 576–8. doi:10.1007/s00467-005-1830-z. PMID 15772829. S2CID 12711324.
- ^ Wakida N, Tuyen DG, Adachi M, Miyoshi T, Nonoguchi H, Oka T, Ueda O, Tazawa M, Kurihara S, Yoneta Y, Shimada H, Oda T, Kikuchi Y, Matsuo H, Hosoyamada M, Endou H, Otagiri M, Tomita K, Kitamura K (April 2005). "Mutations in human urate transporter 1 gene in presecretory reabsorption defect type of familial renal hypouricemia". J. Clin. Endocrinol. Metab. 90 (4): 2169–74. doi:10.1210/jc.2004-1111. PMID 15634722.
- ^ Toncev G, Milicic B, Toncev S, Samardzic G (May 2002). "Serum uric acid levels in multiple sclerosis patients correlate with activity of disease and blood–brain barrier dysfunction". Eur. J. Neurol. 9 (3): 221–6. doi:10.1046/j.1468-1331.2002.00384.x. PMID 11985629. S2CID 7832500.
- ^ Wilcox, W. D. (June 1996). "Abnormal serum uric acid levels in children". The Journal of Pediatrics. 128 (6): 731–741. doi:10.1016/S0022-3476(96)70322-0. ISSN 0022-3476. PMID 8648529.
- ^ Martín Hernández E, Aparicio López C, Alvarez Calatayud G, García Herrera MA (September 2001). "[Vesical uric acid lithiasis in a child with renal hypouricemia]". An. Esp. Pediatr. (in Spanish). 55 (3): 273–6. PMID 11676906. Archived from the original on 2009-03-27. Retrieved 2008-12-25.
- ^ Crook M (December 1993). "Hypouricaemia in a hospital population". Scand. J. Clin. Lab. Invest. 53 (8): 883–5. doi:10.3109/00365519309086502. PMID 8140400.
