Deoxyribonuclease gamma
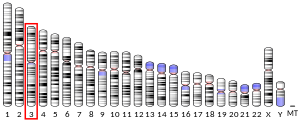
Deoxyribonuclease gamma (also termed DNase γ, deoxyribonuclease 1L3, DNASE1L3, of deoxyribonuclease I like 3) is an enzyme that in humans is encoded by the DNASE1L3 (also termed the deoxyribonuclease 1L3 or deoxyribonuclease 1 like 3) gene. This gene's is located on chromosome 3's "p arm", i.e., short arm, between region 1, band 4, sub-band 3 and region 2, band 1, sub-band 1 (this location's is abbreviation as 3p14.3-p21.1)[5][6]
Function
[edit]DNASE1L3 belongs to the family of deoxyribonuclease enzymes that are responsible for degrading DNA. Specifically, DNASE1L3 plays a key role in the breakdown of extracellular DNA, particularly DNA released from dying cells due to apoptosis or necrosis. This function is important for maintaining cellular homeostasis and preventing the accumulation of DNA debris, which could otherwise trigger widespread inflammatory autoimmune responses.[7]
Clinical significance
[edit]Role in autoimmune response
[edit]Humans with inactivating mutations in both of their DNASE1L3 genes have a greatly recuced ability fail to remove the extracellular DNA released by dead cell and therefore to eliminate these dead cells. This failure leads to the accumulation of DNA deposits and dead cells, which triggers autoimmune inflammation responses throughout the body.[8][9][10] These inflammatory responses cause the following types of inflammatory disorders.
Systemic lupus erythematosus (SLE)
[edit]Systemic lupus erythematosus (SLE) is a disorder in which an individua's immune system loses its tolerance for and therefore mounts inflammatory attacks on certain self-antigens in various tissues.[11] SLE most often develops in adults but in 10% to 20% of cases occurs in individuals less than 19 years old.[12][13] This childhood form of SLE, termed childhood-onset SLE, juvenile-onset SLE, juvenile SLE, or pediatric SLE,[14][15] is a more severe disorder than adult onset SLE in part because it more often involves lupus nephritis, kidney failure, and inflammation in the central nervous system.[16] A small percentage of pediatric SLE cases are caused by defects in both of an individual's DNASE1L3 genes.[9][10][16][17][18] These rare cases of pediatric SLE due to defective DNASE1L3 genes are classified as being one of the inborn error of immunity disorders.[8][14]
Other associated disorders
[edit]In extremely rare cases, inactivating mutations in the DNASE1L3 genes have also been associated with the development of pediatric rheumatoid arthritis[19][20][21][22] or the hypocomplementemic urticarial vasculitis syndrome (also known as McDuffie syndrome). Among 13 patients with this syndrome, four also had rheumatoid arthritis.[9][16][23] Individuals with DNASE1L3-deficient rheumatoid arthritis or hypocomplementemic urticarial vasculitis syndrome may concurrently present with additional inflammation-induced conditions such as alveolar hemorrhages, inflammatory bowel disease, uveitis, scleritis, inflammation of the gallbladder, or arthritis/arthralgia in multiple joints.[9][16]
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000163687 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000025279 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Rodriguez AM, Rodin D, Nomura H, Morton CC, Weremowicz S, Schneider MC (June 1997). "Identification, localization, and expression of two novel human genes similar to deoxyribonuclease I". Genomics. 42 (3): 507–513. doi:10.1006/geno.1997.4748. PMID 9205125.
- ^ "Entrez Gene: DNASE1L3 deoxyribonuclease I-like 3".
- ^ Han DS, Lo YM (August 2021). "The Nexus of cfDNA and Nuclease Biology". Trends in Genetics. 37 (8): 758–770. doi:10.1016/j.tig.2021.04.005. PMID 34006390.
- ^ a b Yu JE (February 2024). "New primary immunodeficiencies 2023 update". Current Opinion in Pediatrics. 36 (1): 112–123. doi:10.1097/MOP.0000000000001315. PMID 38001560.
- ^ a b c d Tusseau M, Khaldi-Plassart S, Cognard J, Viel S, Khoryati L, Benezech S, et al. (April 2024). "Mendelian Causes of Autoimmunity: the Lupus Phenotype". Journal of Clinical Immunology. 44 (4): 99. doi:10.1007/s10875-024-01696-8. PMID 38619739.
- ^ a b Tangye SG, Al-Herz W, Bousfiha A, Chatila T, Cunningham-Rundles C, Etzioni A, et al. (January 2020). "Human Inborn Errors of Immunity: 2019 Update on the Classification from the International Union of Immunological Societies Expert Committee". Journal of Clinical Immunology. 40 (1): 24–64. doi:10.1007/s10875-019-00737-x. PMC 7082301. PMID 31953710.
- ^ Kiriakidou M, Ching CL (June 2020). "Systemic Lupus Erythematosus". Annals of Internal Medicine. 172 (11): ITC81 – ITC96. doi:10.7326/AITC202006020. PMID 32479157.
- ^ Massias JS, Smith EM, Al-Abadi E, Armon K, Bailey K, Ciurtin C, et al. (April 2020). "Clinical and laboratory characteristics in juvenile-onset systemic lupus erythematosus across age groups". Lupus. 29 (5): 474–481. doi:10.1177/0961203320909156. PMC 7528537. PMID 32233733.
- ^ Lythgoe H, Lj M, Hedrich CM, Aringer M (January 2022). "Classification of systemic lupus erythematosus in children and adults". Clinical Immunology. 234: 108898. doi:10.1016/j.clim.2021.108898. PMID 34856381.
- ^ a b Bousfiha A, Moundir A, Tangye SG, Picard C, Jeddane L, Al-Herz W, et al. (October 2022). "The 2022 Update of IUIS Phenotypical Classification for Human Inborn Errors of Immunity". Journal of Clinical Immunology. 42 (7): 1508–1520. doi:10.1007/s10875-022-01352-z. PMID 36198931.
- ^ Omarjee O, Picard C, Frachette C, Moreews M, Rieux-Laucat F, Soulas-Sprauel P, et al. (October 2019). "Monogenic lupus: Dissecting heterogeneity". Autoimmunity Reviews. 18 (10): 102361. doi:10.1016/j.autrev.2019.102361. PMID 31401343.
- ^ a b c d Tusseau M, Lovšin E, Samaille C, Pescarmona R, Mathieu AL, Maggio MC, et al. (August 2022). "DNASE1L3 deficiency, new phenotypes, and evidence for a transient type I IFN signaling". Journal of Clinical Immunology. 42 (6): 1310–1320. doi:10.1007/s10875-022-01287-5. PMID 35670985.
- ^ Gray PE, David C (June 2023). "Inborn Errors of Immunity and Autoimmune Disease". The Journal of Allergy and Clinical Immunology. In Practice. 11 (6): 1602–1622. doi:10.1016/j.jaip.2023.04.018. PMID 37119983.
- ^ Belot A, Rice GI, Omarjee SO, Rouchon Q, Smith EM, Moreews M, et al. (February 2020). "Contribution of rare and predicted pathogenic gene variants to childhood-onset lupus: a large, genetic panel analysis of British and French cohorts". The Lancet. Rheumatology. 2 (2): e99 – e109. doi:10.1016/S2665-9913(19)30142-0. hdl:20.500.11820/9168e506-f4b1-44b2-8ce8-4d0ddb201c13. PMID 38263665.
- ^ Tsilifis C, Slatter MA, Gennery AR (2023). "Too much of a good thing: a review of primary immune regulatory disorders". Frontiers in Immunology. 14: 1279201. doi:10.3389/fimmu.2023.1279201. PMC 10645063. PMID 38022498.
- ^ Lee WF, Fan WL, Tseng MH, Yang HY, Huang JL, Wu CY (August 2022). "Characteristics and genetic analysis of patients suspected with early-onset systemic lupus erythematosus". Pediatric Rheumatology Online Journal. 20 (1): 68. doi:10.1186/s12969-022-00722-6. PMC 9375402. PMID 35964089.
- ^ Westra HJ, Martínez-Bonet M, Onengut-Gumuscu S, Lee A, Luo Y, Teslovich N, et al. (October 2018). "Fine-mapping and functional studies highlight potential causal variants for rheumatoid arthritis and type 1 diabetes". Nature Genetics. 50 (10): 1366–1374. doi:10.1038/s41588-018-0216-7. PMC 6364548. PMID 30224649.
- ^ Padyukov L (January 2022). "Genetics of rheumatoid arthritis". Seminars in Immunopathology. 44 (1): 47–62. doi:10.1007/s00281-022-00912-0. PMC 8837504. PMID 35088123.
- ^ Marzano AV, Maronese CA, Genovese G, Ferrucci S, Moltrasio C, Asero R, et al. (April 2022). "Urticarial vasculitis: Clinical and laboratory findings with a particular emphasis on differential diagnosis". The Journal of Allergy and Clinical Immunology. 149 (4): 1137–1149. doi:10.1016/j.jaci.2022.02.007. PMID 35396080.