1826–1837 cholera pandemic
| Second cholera pandemic | |
|---|---|
| Disease | Cholera |
| Bacteria strain | Vibrio cholerae |
| Location | Asia, Europe, the Americas |
| First outbreak | Ganges Delta, British India |
| Dates | 1826–1837 |
| Confirmed cases | Unknown; 250,000 in Russia |
Deaths | Unknown; 100,000 in Russia; 100,000 in France; 6,536 in London |
The second cholera pandemic (1826–1837), also known as the Asiatic cholera pandemic, was a cholera pandemic that reached from India across Western Asia to Europe, Great Britain, and the Americas, as well as east to China and Japan.[1] Cholera caused more deaths than any other epidemic disease in the 19th-century,[2] and as such, researchers consider it a defining epidemic disease of the century.[3][4] The medical community now believes cholera to be exclusively a human disease, spread through many means of travel during the time, and transmitted through warm fecal-contaminated river waters and contaminated foods. During the second pandemic, the scientific community varied in its beliefs about the causes of cholera.
History
[edit]First pandemic
[edit]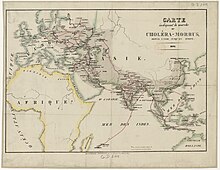
The first cholera pandemic (1817–24) began near Kolkata and spread throughout Southeast Asia to the Middle East, eastern Africa, and the Mediterranean coast. While cholera had spread across India many times previously, this outbreak went farther; it reached as far as China and the Mediterranean Sea before receding. Hundreds of thousands of people died as a result of this pandemic, including many British soldiers, which attracted European attention. This was the first of several cholera pandemics to sweep through Asia and Europe during the 19th and 20th centuries. This first pandemic spread over an unprecedented range of territory, affecting many countries throughout Asia.[5][6]
Origins of the second pandemic
[edit]Historians believe that the first pandemic had lingered in Indonesia and the Philippines in 1830.[7][8]
Although not much is known about the journey of the cholera pandemic in east India, many believe that this pandemic began, like the first, with outbreaks along the Ganges Delta in India. From there, the disease spread along trade routes to cover most of India. By 1828, the disease had traveled to China. Cholera was also reported in China in 1826 and 1835, and in Japan in 1831. In 1829, Iran was apparently infected with cholera from Afghanistan.[9]
Cholera reached the southern tips of the Ural Mountains in 1829. On 26 August 1829, the first cholera case was recorded in Orenburg with reports of outbreaks in Bugulma (7 November), Buguruslan (5 December), Menzelinsk (2 January 1830), and Belebey (6 January). With 3,500 cases including 865 fatal ones in Orenburg province, the epidemic stopped by February 1830.[10]
1830s
[edit]
The second cholera pandemic spread from Russia to the rest of Europe, claiming hundreds of thousands of lives.[11] By 1831, the epidemic had infiltrated Russia's main cities and towns. Russian soldiers brought the disease to Poland in February 1831. There were reported to have been 250,000 cases of cholera and 100,000 deaths in Russia.[7] In 1831, it is estimated that up to 100,000 deaths occurred in Hungary.[12]
The cholera epidemic struck Warsaw during the November Uprising between 16 May and 20 August 1831; 4,734 people fell ill and 2,524 died.[13] The epidemic of cholera brought to Poland and East Prussia by Russian soldiers forced Prussian authorities to close their borders to Russian transports.[14] There were Cholera Riots in the Russian Empire caused by the government's anticholera measures.[15][16]
By early 1831, frequent reports of the spread of the pandemic in Russia prompted the British government to issue quarantine orders for ships sailing from Russia to British ports.[17] By late summer, with the disease appearing more likely to spread to Britain, its board of health, in accordance with the prevailing miasma theory, issued orders recommending as a preventive the burning of "decayed articles, such as rags, cordage, papers, old clothes, hangings...filth of every description removed, clothing and furniture should be submitted to copious effusions of water, and boiled in a strong ley (lye); drains and privies thoroughly cleansed by streams of water and chloride of lime...free and continued admission of fresh air to all parts of the house and furniture should be enjoined for at least a week".[18]
Based on the reports of two English doctors who had observed the epidemic in Saint Petersburg, the board of health published a detailed description of the disease's symptoms and onset:
Giddiness, sick stomach, nervous agitation, intermittent, slow, or small pulse, cramps beginning at the tops of the fingers and toes, and rapidly approaching the trunk, give the first warning. Vomiting or purging, or both these evacuations of a liquid like rice-water or whey, or barley-water, come on; the features become sharp and contracted, the eye sinks, the look is expressive of terror and wildness; the lips, face, neck, hands, and feet, and soon after the thighs, arms, and whole surface assume a leaden, blue, purple, black, or deep brown tint according to the complexion of the individual, varying in shade with the intensity of the attack. The fingers and toes are reduced in size, the skin and soft parts covering them are wrinkled, shrivelled and folded. The nails put on a bluish pearly white; the larger superficial veins are marked by flat lines of a deeper black; the pulse becomes either small as a thread, and scarcely vibrating, or else totally extinct. The skin is deadly cold and often damp, the tongue always moist, often white and loaded, but flabby and chilled like a piece of dead flesh. The voice is nearly gone; the respiration quick, irregular, and imperfectly performed. The patient speaks in a whisper. He struggles for breath, and often lays his hand on his heart to point out the seat of his distress. Sometimes there are rigid spasms of the legs, thighs, and loins. The secretion of urine is totally suspended; vomiting and purgings, which are far from being the most important or dangerous symptoms, and which in a very great number of cases of the disease, have not been profuse, or have been arrested by medicine early in the attack, succeed. It is evident that the most urgent and peculiar symptom of this disease is the sudden depression of the vital powers: proved by the diminished action of the heart, the coldness of the surface and extremities, and the stagnant state of the whole circulation.[19]
From September 1831 to January 1832, a catastrophic cholera epidemic ravaged the lower Euphrates and Tigris regions of what is now Iraq and Iran. In Shushtar, Iran, about half of the city's inhabitants died from cholera. The Mandaean community was hit particularly hard, and all of their priests died in the plague. Yahya Bihram told Julius Heinrich Petermann that there were only 1,500 Mandaean survivors after the plague.[20]

The epidemic reached Great Britain in October 1831,[21] appearing in Sunderland, where it was carried by passengers on a ship from the Baltic. It also appeared in Gateshead and Newcastle. In London, the disease claimed 6,536 victims; in Paris, 20,000 died (out of a population of 650,000), with about 100,000 deaths in all of France.[22] In 1832, the epidemic reached Quebec, Ontario, and Nova Scotia in Canada and Detroit and New York City in the United States.[a] It reached the Pacific coast of North America between 1832 and 1834.[1] The pandemic prompted the passage of the landmark Public Health Act 1848 (11 & 12 Vict. c. 63) and the Nuisances Removal and Diseases Prevention Acts, 1848 and 1849, in England.[7]
In mid-1832, 57 Irish immigrants died who had been laying a stretch of railroad called Duffy's Cut, 30 miles west of Philadelphia. They had all contracted cholera.[23]
Causes
[edit]During the second pandemic, the scientific community varied in its beliefs about the causes of cholera. In France, doctors believed cholera was associated with the poverty of certain communities or poor environment. Russians believed the disease was contagious, although doctors did not understand how it spread. The United States believed that cholera was brought by recent immigrants, specifically the Irish, and epidemiologists understand they were carrying disease from British ports. Lastly, the British thought the disease might rise from divine intervention.[24]
Legacy
[edit]
Norwegian poet Henrik Wergeland wrote a stage play inspired by the pandemic, which had reached Norway. In The Indian Cholera (Den indiske Cholera, 1835), he set his play in Colonial India, lambasting the poor response to the pandemic by authorities.[25][26][27]
In response to the second cholera pandemic, the Ottoman Empire and Egypt reformed their quarantine systems, following the western Mediterranean model. In 1831, the Egyptian Quarantine Board was established. It constructed Egypt’s first modern lazaretto in Alexandria in 1833. In 1831, the Ottoman government set up the first permanent quarantine complex in Istanbul. In 1838, the Ottoman government established the Supreme Council of Health, which oversaw 59 quarantines. While largely useless against cholera, these quarantines shored up the two countries' epidemiological defenses against bubonic plague.[28]
As a result of the epidemic, the medical community developed a major advance, the intravenous saline drip. It was developed from the work of Dr. Thomas Latta of Leith, near Edinburgh. Latta established from blood studies that a saline drip greatly improved the condition of patients and saved many lives by preventing dehydration. Latta died in 1833 of tuberculosis.[29]
See also
[edit]Notes
[edit]- ^ It first appeared in Quebec with the arrival on 28 April 1832 of the ship Constantia, which had come from Ireland.
References
[edit]- ^ a b "Cholera's seven pandemics". Canadian Broadcasting Corporation. December 2, 2008. Retrieved 2008-12-11.
- ^ Al‐Adham, Ibrahim S.I.; Jaber, Nisrein; Ali Agha, Ahmed S.A.; Al-Remawi, Mayyas; Al-Akayleh, Faisal; Al-Muhtaseb, Najah; Collier, Philip J. (March 2024). "Sporadic regional re-emergent cholera: a 19th century problem in the 21st century". Journal of Applied Microbiology. 135 (3). doi:10.1093/jambio/lxae055.
The third cholera pandemic (1852–1860) originating in India, is known for its widespread geographical reach and high mortality rate—being the deadliest of 19th-century epidemics.
- ^ Meehan, C. D.; Markel, H. (2009). "Cholera, Historical". In Schaechter, Moselio (ed.). Encyclopedia of Microbiology (Third ed.). Academic Press. pp. 24–29. doi:10.1016/B978-012373944-5.00301-1. ISBN 9780123739445.
- ^ Johnston, William (May 2019). "Cholera and the Environment in Nineteenth-Century Japan". Cross-Currents: East Asian History and Culture Review. 8 (1). University of Hawai'i Press. doi:10.1353/ach.2019.0005 – via Project Muse.
More than any other acute infectious disease, cholera was a defining element of the nineteenth century. This was as true for those living on the Japanese archipelago as for other people across the globe.
- ^ Cholera's seven pandemics, cbc.ca, December 2, 2008.
- ^ "Cholera – Cholera through history". Encyclopedia Britannica. Retrieved 2020-12-10.
- ^ a b c "Asiatic Cholera Pandemic of 1826-37". UCLA Fielding School of Public Health. August 6, 2001. Archived from the original on February 23, 2024.
- ^ Pollitzer, R. (1954). "Cholera studies. 1. History of the disease". Bulletin of the World Health Organization. 10 (3): 436. PMC 2542143. PMID 13160764.
Haeser remarked in this connexion that the infection which had been introduced during the first pandemic into the Dutch East Indies (now Indonesia) and the Philippines, persisted there until 1830, and also claimed that in 1832 cholera reached the Swan River region of Australia, but showed no tendency to spread there.
- ^ Pollitzer, R. (1954). "Cholera studies. 1. History of the disease". Bulletin of the World Health Organization. 10 (3): 432. PMC 2542143. PMID 13160764.
While information for 1828 is indefinite, it is known that in 1829 cholera was rampant in Afghanistan, penetrated into Persia, and was also present in the region of Bukhara and Chiva.
- ^ Charlotte E. Henze (15 December 2010). Disease, Health Care and Government in Late Imperial Russia: Life and Death on the Volga, 1823-1914. Taylor & Francis. p. 13. ISBN 978-0-203-83397-1.
- ^ J. N. Hays (2005). Epidemics and Pandemics: Their Impacts on Human History. Santa Barbara, California: ABC-CLIO. ISBN 978-1-85109-658-9. OCLC 606929770.
- ^ "Asiatic Cholera Pandemic of 1826-37". Dept. of Epidemiology University of California, Los Angeles.
- ^ Raymond Durand (1980). Robert Bielecki (ed.). Depesze z powstańczej Warszawy 1830–1831: raporty konsula francuskiego w Królestwie Polskim [Memoranda from Warsaw during the Uprising 1830–1831: reports of the French consul to the Kingdom of Poland]. Warsaw: Czytelnik. ISBN 978-83-07-00254-5. OCLC 7732541.
- ^ Tomasz Strzeżek (1998). Kornelia Kompanowska (ed.). Warszawa 1831 [Warsaw 1831]. Historyczne Bitwy. Warsaw: Dom Wydawniczy Bellona. pp. 11–12. ISBN 978-83-11-08793-4.
- ^ Bosin, Yury V. (2009). "Russia, cholera riots of 1830–1831". In Ness, Immanuel (ed.). The International Encyclopedia of Revolution and Protest (PDF). Blackwell Publishing. pp. 2877–2878.
- ^ Kraikovski, Alexei (2013). "The St. Petersburg Cholera Riot of 1831: Water Pollution and Social Tension". Arcadia: Explorations in Environmental History. 9. Rachel Carson Center for Environment and Society. doi:10.5282/rcc/5299. ISSN 2199-3408.
- ^ "No. 18807". The London Gazette. 27 May 1831. p. 1027.
- ^ "No. 18863". The London Gazette. 21 October 1831. p. 2160.
- ^ "No. 18863". The London Gazette. 21 October 1831. p. 2159.
- ^ Buckley, Jorunn Jacobsen (2010). The great stem of souls: reconstructing Mandaean history. Piscataway, N.J: Gorgias Press. ISBN 978-1-59333-621-9.
- ^ "Cholera in Sunderland". UK Parliament. Archived from the original on 2013-07-06.
- ^ Rosenberg, Charles E. (1987). The Cholera Years: The United States in 1832, 1849, and 1866. University of Chicago Press. ISBN 0-226-72677-0.
- ^ The Ghosts of Duffy's Cut. Praeger Publishers. 2006. ISBN 0-275-98727-2.
In the summer of 1832, Irish immigrant Philip Duffy contracted 57 of his newly arrived countrymen to lay a stretch of railroad some 30 miles west of Philadelphia. Within two months, all were dead, struck down in the global cholera pandemic that hit Philadelphia the same time they did.
- ^ Hayes, J.N. (2005). Epidemics and Pandemics: Their Impacts on Human History. Santa Barbara, CA: ABC-CLIO. pp. 214–219.
- ^ Kumar Rai, Saurav (July 3, 2020). "Pandemics Through Indian Literary Lens". Peepul Tree Stories. Retrieved September 17, 2024.
- ^ Schiedermair, Joachim (December 2012). "The Masses and the Elite: the Conception of Social Inequality in 1840s Scandinavian Literature". Romantik: Journal for the Study of Romanticisms. 1 (1): 125. doi:10.7146/rom.v1i1.15853.
- ^ Zwart, Hub (2020). "Emerging viral threats and the simultaneity of the non-simultaneous: zooming out in times of Corona". Medicine, Health Care and Philosophy. 23 (4): 589–602. doi:10.1007/s11019-020-09970-3. PMC 7394271. PMID 32737743.
- ^ Hamed-Troyansky, Vladimir (2021). "Ottoman and Egyptian Quarantines and European Debates on Plague in the 1830s–1840s". Past and Present (253): 235–270. doi:10.1093/pastj/gtaa017.
- ^ Janakan, Gnananandan; Ellis, Harold (May 2013). "Dr Thomas Aitchison Latta (cl796-1833): pioneer of intravenous fluid replacement in the treatment of cholera". Journal of Medical Biography. 21 (2): 70–74. doi:10.1258/jmb.2012.012004. ISSN 0967-7720. PMID 24585745. S2CID 32188771.
Further reading
[edit]- ""Cholera Epidemics in the 19th Century" in Contagion: Historical Views of Diseases and Epidemics". CURIOSity Digital Collections. Harvard Library. Retrieved September 17, 2024.
- Pelling, Margaret (April 26, 2022). "Epidemics in Nineteenth-Century British Towns: How Important was Cholera?". Journal of Victorian Culture. 27 (2): 346–355. doi:10.1093/jvcult/vcac019.
