Cancer cell
Cancer cells are cells that divide continually, forming solid tumors or flooding the blood or lymph with abnormal cells.[1] Cell division is a normal process used by the body for growth and repair. A parent cell divides to form two daughter cells, and these daughter cells are used to build new tissue or to replace cells that have died because of aging or damage.[2] Healthy cells stop dividing when there is no longer a need for more daughter cells, but cancer cells continue to produce copies. They are also able to spread from one part of the body to another in a process known as metastasis.[3]
Classification
[edit]There are different categories of cancer cell, defined according to the cell type from which they originate.[4]
- Carcinoma, the majority of cancer cells are epithelial in origin, beginning in a tissue that lines the inner or outer surfaces of the body.[5]
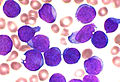
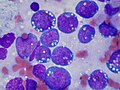
- Leukaemia, originate in the tissues responsible for producing new blood cells, most commonly in the bone marrow.[6][7]
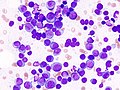
- Lymphoma and myeloma, derived from cells of the immune system.[8]
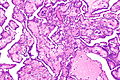
- Sarcoma, originating in connective tissue, including fat, muscle, and bone.[9]
- Central nervous system, derived from cells of the brain and spinal cord.[10]
- Mesothelioma, originating in the mesothelium; the lining of body cavities.[11]
-
Carcinoma
-
Leukaemia
-
Lymphoma
-
Myeloma
-
Sarcoma
-
Mesothelioma
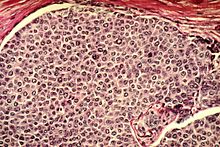
Histology
[edit]
Cancer cells have distinguishing histological features visible under the microscope.[12][13] The nucleus is often large and irregular, and the cytoplasm may also display abnormalities.[14]
Nucleus
[edit]The shape, size, protein composition, and texture of the nucleus are often altered in malignant cells. The nucleus may acquire grooves, folds or indentations, chromatin may aggregate or disperse, and the nucleolus can become enlarged. In normal cells, the nucleus is often round or solid in shape, but in cancer cells the outline is often irregular. Different combinations of abnormalities are characteristic of different cancer types, to the extent that nuclear appearance can be used as a marker in cancer diagnostics and staging.[15]
Causes
[edit]Cancer cells are created when the genes responsible for regulating cell division are damaged.[16] Carcinogenesis is caused by mutation and epimutation of the genetic material of normal cells, which upsets the normal balance between proliferation and cell death. This results in uncontrolled cell division in the body. The uncontrolled and often rapid proliferation of cells can lead to benign or malignant tumours (cancer). Benign tumors do not spread to other parts of the body or invade other tissues. Malignant tumors can invade other organs, spread to distant locations (metastasis) and become life-threatening.[17][18]
More than one mutation is necessary for carcinogenesis. In fact, a series of several mutations to certain classes of genes is usually required before a normal cell will transform into a cancer cell.[19]
Damage to DNA can be caused by exposure to radiation, chemicals, and other environmental sources, but mutations also accumulate naturally over time through uncorrected errors in DNA transcription, making age another risk factor.[20] Oncoviruses can cause certain types of cancer, and genetics are also known to play a role.[21]
Stem cell research suggests that excess SP2 protein may turn stem cells into cancer cells.[22] However, a lack of particular co-stimulated molecules that aid in the way antigens react with lymphocytes can impair the natural killer cells' function, ultimately leading to cancer.[23][24][25]
DNA repair and mutation
[edit]When a cell is deficient in the capacity to repair DNA damages, such damages tend to be retained within the cell at an increased level. These damages, upon replication of the cell’s DNA, may cause replication errors, including mutations that lead to cancer. Numerous inherited DNA repair disorders have been described that increase cancer risk (see Wikipedia article DNA repair-deficiency disorder). In addition, particular DNA repair enzymes have been found to be deficient in multiple cancers.[26][27] For example, deficient expression of the DNA repair enzyme O-6-methylguanine-DNA methyltransferase is observed in several kinds of cancer.
Although a DNA repair deficiency can predispose a cell lineage to develop cancer, increased (rather than decreased) expression of a repair capability may also emerge in the progression of cancer cell lineages, and this capability may be clinically important as reviewed by Lingg et al.[28] For instance, the DNA repair gene DMC1 encodes a protein that is normally expressed only in cells undergoing meiosis where it helps maintain an undamaged germ-line. However, DMC1 is also expressed in various cancer cell lines including cervical, breast, and lymphoma cancer cell lines.[28] Expression of meiotic DNA repair genes such as DMC1 may promote tumor cell growth by dealing with endogenous DNA damage within the tumor, and may also diminish the effectiveness of anticancer therapy, such as radiation therapy.[28]
Pathology
[edit]Cells playing roles in the immune system, such as T-cells, are thought to use a dual receptor system when they determine whether or not to kill sick or damaged human cells. If a cell is under stress, turning into tumors, or infected, molecules including MIC-A and MIC-B are produced so that they can attach to the surface of the cell.[23] These work to help macrophages detect and kill cancer cells.[29]
Discovery
[edit]Early evidence of human cancer can be interpreted from Egyptian papers (1538 BCE) and mummified remains.[30] In 2016, a 1.7 million-year-old osteosarcoma was reported by Edward John Odes (a doctoral student in Anatomical Sciences from Witwatersrand Medical School, South Africa) and colleagues, representing the oldest documented malignant hominin cancer.[31]
The understanding of cancer was significantly advanced during the Renaissance period and in the Age of Discovery. Sir Rudolf Virchow, a German biologist and politician, studied microscopic pathology, and linked his observations to illness. He is described as “the founder of cellular pathology”.[32][33] In 1845, Virchow and John Hughes Bennett independently observed an abnormal increase in white blood cells in patients. Virchow correctly identified the condition as a blood disease, and named it leukämie in 1847 (later anglicised to leukemia).[34][35][36] In 1857, he was the first to describe a type of tumour called chordoma that originated from the clivus (at the base of the skull).[37][38]
Telomerase
[edit]Cancer cells have unique features that make them “immortal” according to some researchers.[39] The enzyme telomerase is used to extend the cancer cell's life span.[40] While the telomeres of most cells shorten after each division, eventually causing the cell to die, telomerase extends the cell's telomeres. This is a major reason that cancer cells can accumulate over time, creating tumors.[39]
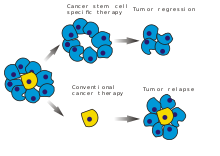
Treatment
[edit]In February 2019, medical scientists announced that iridium attached to albumin, creating a photosensitized molecule, can penetrate cancer cells and, after being irradiated with light (a process called photodynamic therapy), destroy the cancer cells.[41][42]
See also
[edit]References
[edit]- ^ Chakradhar, Shraddha (2019-01-15). "Arrested cells may awaken yet". Nature Medicine. doi:10.1038/d41591-019-00004-x.
- ^ Ong, Joseph Y.; Torres, Jorge Z. (July 2019). "Dissecting the mechanisms of cell division". Journal of Biological Chemistry. 294 (30): 11382–11390. doi:10.1074/jbc.AW119.008149. PMC 6663871.
- ^ "National Cancer Institute: is this cancer?". 2007-09-17. Retrieved 1 August 2016.
- ^ "Histological types of cancer - CRS - Cancer Research Society". www.crs-src.ca. Archived from the original on 2017-08-27. Retrieved 2016-08-02.
- ^ "Cancer Classification | SEER Training". training.seer.cancer.gov. Retrieved 2025-02-24.
- ^ Chennamadhavuni, Adithya; Lyengar, Varun; Mukkamalla, Shiva Kumar R.; Shimanovsky, Alex (2025), "Leukemia", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32809325, retrieved 2025-02-24
- ^ "Leukemia - Symptoms and causes". Mayo Clinic. Retrieved 2025-02-24.
- ^ Díaz-Tejedor, Andrea; Lorenzo-Mohamed, Mauro; Puig, Noemí; García-Sanz, Ramón; Mateos, María-Victoria; Garayoa, Mercedes; Paíno, Teresa (2021-03-17). "Immune System Alterations in Multiple Myeloma: Molecular Mechanisms and Therapeutic Strategies to Reverse Immunosuppression". Cancers. 13 (6): 1353. doi:10.3390/cancers13061353. ISSN 2072-6694. PMC 8002455. PMID 33802806.
- ^ Popovich, John R.; Kashyap, Sarang; Gasalberti, David P.; Cassaro, Sebastiano (2025), "Sarcoma", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30137818, retrieved 2025-02-24
- ^ "Central Nervous System: brain and spinal cord". qbi.uq.edu.au. 2017-11-10. Retrieved 2025-02-24.
- ^ Hiriart, Emilye; Deepe, Raymond; Wessels, Andy (2019-04-08). "Mesothelium and Malignant Mesothelioma". Journal of Developmental Biology. 7 (2): 7. doi:10.3390/jdb7020007. ISSN 2221-3759. PMC 6630312. PMID 30965570.
- ^ Baba, Alecsandru Ioan; Câtoi, Cornel (2007), "TUMOR CELL MORPHOLOGY", Comparative Oncology, The Publishing House of the Romanian Academy, retrieved 2025-02-24
- ^ Kumar, Rajesh; Srivastava, Rajeev; Srivastava, Subodh (2015-08-23). "Detection and Classification of Cancer from Microscopic Biopsy Images Using Clinically Significant and Biologically Interpretable Features". Journal of Medical Engineering. 2015: 1–14. doi:10.1155/2015/457906. ISSN 2314-5129.
- ^ Baba AT, Câtoi C (2007). "Comparative Oncology". Tumor Cell Morphology. The Publishing House of the Romanian Academy.
- ^ Zink D, Fischer AH, Nickerson JA (September 2004). "Nuclear structure in cancer cells". Nature Reviews. Cancer. 4 (9): 677–687. doi:10.1038/nrc1430. PMID 15343274. S2CID 29052588.
- ^ "Cell Division, Cancer | Learn Science at Scitable". www.nature.com. Retrieved 2025-02-24.
- ^ Martin, Tracey A.; Ye, Lin; Sanders, Andrew J.; Lane, Jane; Jiang, Wen G. (2013), "Cancer Invasion and Metastasis: Molecular and Cellular Perspective", Madame Curie Bioscience Database [Internet], Landes Bioscience, retrieved 2025-02-24
- ^ "Metastatic Cancer: When Cancer Spreads - NCI". www.cancer.gov. 2015-05-12. Retrieved 2025-02-24.
- ^ Fearon ER, Vogelstein B (June 1990). "A genetic model for colorectal tumorigenesis". Cell. 61 (5): 759–767. doi:10.1016/0092-8674(90)90186-I. PMID 2188735. S2CID 22975880.
- ^ Ribeiro, Jessica Honorato; Altinisik, Nazlican; Rajan, Nicholas; Verslegers, Mieke; Baatout, Sarah; Gopalakrishnan, Jay; Quintens, Roel (2023-10-10). "DNA damage and repair: underlying mechanisms leading to microcephaly". Frontiers in Cell and Developmental Biology. 11. doi:10.3389/fcell.2023.1268565. hdl:1854/LU-01HCQGJ4BBKZRSHZ3JRPFBQPDG. ISSN 2296-634X.
- ^ "About Cancer". Cancer Research UK. 2017-08-30. Retrieved 2025-02-24.
- ^ "Too much SP2 protein turns stem cells into 'evil twin' cancer cells". ScienceDaily. Retrieved 2025-02-24.
- ^ a b "The Innate Immune System: NK Cells". Community College of Baltimore County. Archived from the original on 2010-07-27. Retrieved 2010-12-01.
- ^ Coënon, Loïs; Geindreau, Mannon; Ghiringhelli, François; Villalba, Martin; Bruchard, Mélanie (2024-08-23). "Natural Killer cells at the frontline in the fight against cancer". Cell Death & Disease. 15 (8): 614. doi:10.1038/s41419-024-06976-0. ISSN 2041-4889. PMC 11343846. PMID 39179536.
- ^ Abel, Alex M.; Yang, Chao; Thakar, Monica S.; Malarkannan, Subramaniam (2018-08-13). "Natural Killer Cells: Development, Maturation, and Clinical Utilization". Frontiers in Immunology. 9. doi:10.3389/fimmu.2018.01869. ISSN 1664-3224. PMC 6099181. PMID 30150991.
- ^ Alhmoud, Jehad F.; Woolley, John F.; Al Moustafa, Ala-Eddin; Malki, Mohammed Imad (2020-04-23). "DNA Damage/Repair Management in Cancers". Cancers. 12 (4): 1050. doi:10.3390/cancers12041050. ISSN 2072-6694. PMC 7226105. PMID 32340362.
- ^ Torgovnick, Alessandro; Schumacher, Björn (2015-04-23). "DNA repair mechanisms in cancer development and therapy". Frontiers in Genetics. 6. doi:10.3389/fgene.2015.00157. ISSN 1664-8021. PMC 4407582.
- ^ a b c Lingg, L.; Rottenberg, S.; Francica, P. (2022). "Meiotic Genes and DNA Double Strand Break Repair in Cancer". Frontiers in Genetics. 13: 831620. doi:10.3389/fgene.2022.831620. PMC 8895043. PMID 35251135.
- ^ Pan, Xing-Qing (2012-11-13). "The mechanism of the anticancer function of M1 macrophages and their use in the clinic". Chinese Journal of Cancer. doi:10.5732/cjc.012.10046 (inactive 24 February 2025).
{{cite journal}}: CS1 maint: DOI inactive as of February 2025 (link) - ^ David AR, Zimmerman MR (October 2010). "Cancer: an old disease, a new disease or something in between?". Nature Reviews. Cancer. 10 (10): 728–733. doi:10.1038/nrc2914. PMID 20814420. S2CID 10492262.
- ^ Odes EJ, Randolph-Quinney PS, Steyn M, Throckmorton Z, Smilg JS, Zipfel B, et al. (2016). "Earliest hominin cancer: 1.7-million-year-old osteosarcoma from Swartkrans Cave, South Africa". South African Journal of Science. 112 (7/8): 5. doi:10.17159/sajs.2016/20150471. ISSN 1996-7489.
- ^ "History of cancer" (PDF). University of Bergen. 23 March 1999. Archived from the original (PDF) on 2012-03-14. Retrieved 2010-11-30.
- ^ "International Online Medical Council (IOMC)". International Online Medical Council. Retrieved 2025-02-24.
- ^ Degos L (2001). "John Hughes Bennett, Rudolph Virchow... and Alfred Donné: the first description of leukemia". The Hematology Journal. 2 (1): 1. doi:10.1038/sj/thj/6200090. PMID 11920227.
- ^ Kampen KR (January 2012). "The discovery and early understanding of leukemia". Leukemia Research. 36 (1): 6–13. doi:10.1016/j.leukres.2011.09.028. PMID 22033191.
- ^ Mukherjee S (16 November 2010). The Emperor of All Maladies: A Biography of Cancer. Simon and Schuster. ISBN 978-1-4391-0795-9. Retrieved 6 September 2011.
- ^ Hirsch EF, Ingals M (May 1923). "Sacrococcygeal chordoma". JAMA: The Journal of the American Medical Association. 80 (19): 1369. doi:10.1001/jama.1923.02640460019007.
- ^ Lopes A, Rossi BM, Silveira CR, Alves AC (1996). "Chordoma: retrospective analysis of 24 cases". Sao Paulo Medical Journal = Revista Paulista de Medicina. 114 (6): 1312–1316. doi:10.1590/S1516-31801996000600006. PMID 9269106.
- ^ a b Duesberg, Peter; McCormack, Amanda (March 1, 2013). "Immortality of cancers: A consequence of inherent karyotypic variations and selections for autonomy". Cell Cycle. 12 (5): 783–802. doi:10.4161/cc.23720. ISSN 1538-4101. PMC 3610726. PMID 23388461.
- ^ Shay, Jerry W. (2016-06-01). "Role of Telomeres and Telomerase in Aging and Cancer". Cancer Discovery. 6 (6): 584–593. doi:10.1158/2159-8290.CD-16-0062. ISSN 2159-8274. PMC 4893918. PMID 27029895.
- ^ University of Warwick (3 February 2019). "Simply shining light on dinosaur metal compound kills cancer cells". EurekAlert!. Retrieved 3 February 2019.
- ^ Zhang P, Huang H, Banerjee S, Clarkson GJ, Ge C, Imberti C, Sadler PJ (February 2019). "Nucleus-Targeted Organoiridium-Albumin Conjugate for Photodynamic Cancer Therapy". Angewandte Chemie. 58 (8): 2350–2354. doi:10.1002/anie.201813002. PMC 6468315. PMID 30552796.
Further reading
[edit]- Schwarzer, K.; Foerster, M.; Steiner, T.; Hermann, I. M.; Straube, E. (2010). "BCG strain S4-Jena: An early BCG strain is capable to reduce the proliferation of bladder cancer cells by induction of apoptosis". Cancer Cell International. 10: 21. doi:10.1186/1475-2867-10-21. PMC 2908063. PMID 20587032.
External links
[edit]- The History of Cancer Archived 2015-12-12 at the Wayback Machine. Cancer.org. Retrieved on 2010-12-01