Knee
This article needs additional citations for verification. (February 2022) |
| Knee | |
|---|---|
 Human knees | |
 Right knee (front-right view) | |
| Details | |
| System | Musculoskeletal system |
| Nerve | Femoral, obturator, sciatic |
| Identifiers | |
| Latin | articulatio genus |
| MeSH | D007717 |
| TA98 | A01.1.00.036 |
| TA2 | 161 |
| FMA | 24974 |
| Anatomical terminology | |
In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia (tibiofemoral joint), and one between the femur and patella (patellofemoral joint).[1] It is the largest joint in the human body.[2] The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.
It is often termed a compound joint having tibiofemoral and patellofemoral components.[3][4] (The fibular collateral ligament is often considered with tibiofemoral components.)[5]
Structure
[edit]The knee is a modified hinge joint, a type of synovial joint, which is composed of three functional compartments: the patellofemoral articulation, consisting of the patella, or "kneecap", and the patellar groove on the front of the femur through which it slides; and the medial and lateral tibiofemoral articulations linking the femur, or thigh bone, with the tibia, the main bone of the lower leg.[6] The joint is bathed in synovial fluid which is contained inside the synovial membrane called the joint capsule. The posterolateral corner of the knee is an area that has recently been the subject of renewed scrutiny and research.[7]
The knee is the largest joint and one of the most important joints in the body. It plays an essential role in movement related to carrying the body weight in horizontal (running and walking) and vertical (jumping) directions.[8]
At birth, the kneecap is just formed from cartilage, and this will ossify (change to bone) between the ages of three and five years. Because it is the largest sesamoid bone in the human body, the ossification process takes significantly longer.[9]
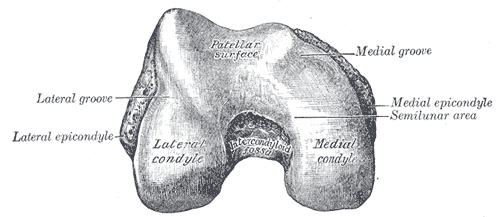
Articular bodies
[edit]The main articular bodies of the femur are its lateral and medial condyles. These diverge slightly distally and posteriorly, with the lateral condyle being wider in front than at the back while the medial condyle is of more constant width.[10]: 206 The radius of the condyles' curvature in the sagittal plane becomes smaller toward the back. This diminishing radius produces a series of involute midpoints (i.e. located on a spiral). The resulting series of transverse axes permit the sliding and rolling motion in the flexing knee while ensuring the collateral ligaments are sufficiently lax to permit the rotation associated with the curvature of the medial condyle about a vertical axis.[10]: 194–95
The pair of tibial condyles are separated by the intercondylar eminence[10]: 206 composed of a lateral and a medial tubercle.[10]: 202
The patella also serves an articular body, and its posterior surface is referred to as the trochlea of the knee.[11] It is inserted into the thin anterior wall of the joint capsule.[10]: 206 On its posterior surface is a lateral and a medial articular surface,[10]: 194 both of which communicate with the patellar surface which unites the two femoral condyles on the anterior side of the bone's distal end.[10]: 192
Articular capsule
[edit]The articular capsule has a synovial and a fibrous membrane separated by fatty deposits. Anteriorly, the synovial membrane is attached on the margin of the cartilage both on the femur and the tibia, but on the femur, it communicates with the suprapatellar bursa or recess and extends the joint space proximally.[10]: 210 The suprapatellar bursa is prevented from being pinched during extension by the articularis genus muscle.[12] Behind, the synovial membrane is attached to the margins of the two femoral condyles which produces two extensions (semimembranosus bursa under medial head of the gastrocnemius and popliteal bursa under lateral head of the gastrocnemius)[13] similar to the suprapatellar bursa. Between these two extensions, the synovial membrane passes in front of the two cruciate ligaments at the center of the joint, thus forming a pocket direct inward.[10]: 210
Synovium lining the capsule and its bursae. The synovium also lines infrapatellar fat pad, the fat pad that lies below the ligamentum patellae. Synovium projecting into the fat pad as two foldings.[13]
Nerves
[edit]From an anterior perspective, the superolateral quadrant of the knee is innervated by the nerves to the vastus lateralis and vastus intermedius, the sciatic nerve, and by the superior lateral genicular and common fibular nerves; in the inferolateral quadrant, the inferior lateral genicular nerve and recurrent fibular nerves predominate; the superomedial quadrant is innervated by the nerves to the vastus medialis and vastus intermedius, the obturator and sciatic nerves, and by the superior medial genicular nerve; and the inferomedial quadrant has innervation by the inferior medial genicular nerve and the infrapatellar branch of the saphenous nerve.[14][15]
The articular branches from the obturator and tibial nerves supply the posterior knee capsule, with additional supply from the common fibular nerve and sciatic nerve; the tibial nerve innervates the entire posterior capsule; the posterior division of the obturator nerve and the tibial nerve supply the superomedial aspect of the posterior capsule; the superolateral aspect of the posterior capsule is innervated by the tibial nerve, and by the common fibular and sciatic nerves.[15][16]
Bursae
[edit]Numerous bursae surround the knee joint. The largest communicative bursa is the suprapatellar bursa described above. Four considerably smaller bursae are located on the back of the knee. Two non-communicative bursae are located in front of the patella and below the patellar tendon, and others are sometimes present.[10]: 210
Cartilage
[edit]Cartilage is a thin, elastic tissue that protects the bone and makes certain that the joint surfaces can slide easily over each other. Cartilage ensures supple knee movement. There are two types of joint cartilage in the knees: fibrous cartilage (the meniscus) and hyaline cartilage. Fibrous cartilage has tensile strength and can resist pressure.[clarification needed] Hyaline cartilage covers the surface along which the joints move. Collagen fibres within the articular cartilage have been described by Benninghoff as arising from the subchondral bone in a radial manner, building so called Gothic arches. On the surface of the cartilage, these fibres appear in a tangential orientation and increase the abrasion resistance. There are no blood vessels inside of the hyaline cartilage, the alimentation is performed per diffusion. Synovial fluid and the subchondral bone marrow serve both as nutrition sources for the hyaline cartilage. Lack of at least one source induces a degeneration. Cartilage will wear over the years. Cartilage has a very limited capacity for self-restoration. The newly formed tissue will generally consist of a large part of fibrous cartilage of lesser quality than the original hyaline cartilage. As a result, new cracks and tears will form in the cartilage over time.[17]
Menisci
[edit]The articular disks of the knee-joint are called menisci because they only partly divide the joint space.[10]: 26 These two disks, the medial meniscus and the lateral meniscus, consist of connective tissue with extensive collagen fibers containing cartilage-like cells. Strong fibers run along the menisci from one attachment to the other, while weaker radial fibers are interlaced with the former. The menisci are flattened at the center of the knee joint, fused with the synovial membrane laterally, and can move over the tibial surface.[10]: 208 [18] The upper and lower surfaces of the menisci are free. Each meniscus have anterior and posterior horns that meet in the intercondylar area of the tibia.[13]
Medial meniscus is bigger, less curved, and thinner. Its posterior horn is thicker (14mm) than the anterior horn (6mm).[13]
The lateral meniscus is smaller, more curved (nearly circular), and has more uniform thickness than medial meniscus (10mm). The lateral meniscus is less attached to the joint capsule, because its posterolateral surface is grooved by the popliteus tendon, separating the meniscus from the capsule. The popliteus tendon is not attached to the lateral meniscus.[13]
Ligaments
[edit]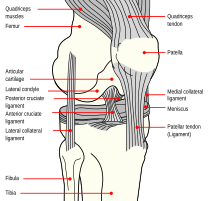
The ligaments surrounding the knee joint offer stability by limiting movements and, together with the menisci and several bursae, protect the articular capsule.[19]
Intracapsular
[edit]The knee is stabilized by a pair of cruciate ligaments. These ligaments are both extrasynovial, intracapsular ligaments.[20] The anterior cruciate ligament (ACL) stretches from the lateral condyle of femur to the anterior intercondylar area.[13] The ACL prevents the tibia from being pushed too far anterior relative to the femur.[13] It is often torn during twisting or bending of the knee.[21] The posterior cruciate ligament (PCL) stretches from medial condyle of femur to the posterior intercondylar area. This ligament prevents posterior displacement of the tibia relative to the femur.[13] Injury to this ligament is uncommon but can occur as a direct result of forced trauma to the ligament.[citation needed]
The transverse ligament stretches from the lateral meniscus to the medial meniscus. It passes in front of the menisci. It is divided into several strips in 10% of cases.[10]: 208 The two menisci are attached to each other anteriorly by the ligament.[22] The posterior (of Wrisberg) and anterior meniscofemoral ligaments (of Humphrey) stretch from the posterior horn of the lateral meniscus to the medial femoral condyle. They pass anterior and posterior to the posterior cruciate ligament respectively.[13][10]: 208 The meniscotibial ligaments (or "coronary") stretches from inferior edges of the menisci to the periphery of the tibial plateaus.
Extracapsular
[edit]The patellar ligament connects the patella to the tuberosity of the tibia. It is also occasionally called the patellar tendon because there is no definite separation between the quadriceps tendon (which surrounds the patella) and the area connecting the patella to the tibia.[23] This very strong ligament helps give the patella its mechanical leverage[24] and also functions as a cap for the condyles of the femur. Laterally and medially to the patellar ligament, the lateral and medial retinacula connect fibers from the vasti lateralis and medialis muscles to the tibia. Some fibers from the iliotibial tract radiate into the lateral retinaculum and the medial retinaculum receives some transverse fibers arising on the medial femoral epicondyle.[10]: 206
The medial collateral ligament (MCL a.k.a. "tibial") stretches from the medial epicondyle of the femur to the medial tibial condyle. It is composed of three groups of fibers, one stretching between the two bones, and two fused with the medial meniscus. The MCL is partly covered by the pes anserinus and the tendon of the semimembranosus passes under it.[10]: 206 It protects the medial side of the knee from being bent open by a stress applied to the lateral side of the knee (a valgus force).[10]: 206
The lateral collateral ligament (LCL a.k.a. "fibular") stretches from the lateral epicondyle of the femur to the head of fibula. It is separate from both the joint capsule and the lateral meniscus.[10]: 206 It protects the lateral side from an inside bending force (a varus force). The anterolateral ligament (ALL) is situated in front of the LCL.[citation needed]
Lastly, there are two ligaments on the dorsal side of the knee. The oblique popliteal ligament is a radiation of the tendon of the semimembranosus on the medial side, from where it is direct laterally and proximally. The arcuate popliteal ligament originates on the apex of the head of the fibula to stretch proximally, crosses the tendon of the popliteus muscle, and passes into the capsule.[10]: 206
Muscles
[edit]The most muscles responsible for the movement of the knee joint belong to either the anterior, medial or posterior compartment of the thigh. The extensors generally belong to the anterior compartment and the flexors to the posterior. The two exceptions to this is gracilis, a flexor, which belongs to the medial compartment and sartorius, a flexor, in the anterior compartment. Additionally, some muscles in the lower leg provide weak knee flexion, namely the gastrocnemius, in addition to their primary function of moving the foot.
Extensors
[edit]Flexors
[edit]Posterior compartment
| Muscle | Origin | Insertion | Artery | Nerve | Action | Antagonist |
|---|---|---|---|---|---|---|
| Sartorius | Anterior superior iliac spine | Pes anserinus | superficial circumflex iliac artery, lateral femoral artery, deep femoral artery, descending geniculate artery, femoral artery | femoral nerve | hip joint: flexion, lateral rotation and abduction. Knee joint: flexion and medial rotation | Quadriceps muscle (partly) |
| Biceps femoris | Long head: tuberosity of the ischium, short head: linea aspera on the femur[25] | The head of the fibula[25] which articulates with the back of the lateral tibial condyle | Inferior gluteal artery, perforating arteries, popliteal artery | Long head: medial (tibial) part of sciatic nerve, short head: lateral (common fibular) part of sciatic nerve[25] | Flexion of knee, laterally rotates leg at knee (when knee is flexed), extends hip joint (long head only)[25] | Quadriceps muscle |
| Semitendinosus | Tuberosity of the ischium[25] | Pes anserinus | Inferior gluteal artery, perforating arteries | Sciatic[25] (tibial, L5, S1, S2) | Flexes knee, extends hip joint, medially rotates leg at knee[25] | Quadriceps muscle |
| Semimembranosus | Tuberosity of the ischium[25] | Medial surface of tibia[25] | Profunda femoris, gluteal artery | Sciatic nerve[25] | Flexes knee, extends hip joint, medially rotates leg at knee[25] | Quadriceps muscle |
| Gastrocnemius | Medial and lateral condyle of the femur | Calcaneus | Sural arteries | Tibial nerve from the sciatic, specifically, nerve roots S1, S2 | Minor flexion of knee and plantarflexion | Tibialis anterior muscle |
| Plantaris | Lateral supracondylar ridge of femur above lateral head of gastrocnemius | Tendo calcaneus (medial side, deep to gastrocnemius tendon) | Sural arteries | Tibial nerve | Flexes knee and plantar flexes foot | Tibialis anterior muscle |
| Popliteus | Middle facet of the lateral surface of the lateral femoral condyle | Posterior tibia under the tibial condyles | Popliteal artery | Tibial nerve | Medial rotation and flexion of knee |
Medial compartment:
| Muscle | Origin | Insertion | Artery | Nerve | Action | Antagonist |
|---|---|---|---|---|---|---|
| Gracilis | Inferior pubic ramus[26] | Pes anserinus | Obturator artery | Anterior branch of obturator nerve[26] | Flexion and medial rotation of knee;[26] adduction of hip, flexion of hip, |
Blood supply
[edit]
The femoral artery and the popliteal artery help form the arterial network or plexus, surrounding the knee joint. There are six main branches: two superior genicular arteries, two inferior genicular arteries, the descending genicular artery and the recurrent branch of anterior tibial artery.[27]
The medial genicular arteries penetrate the knee joint.
Function
[edit]The knee permits flexion and extension about a virtual transverse axis, as well as a slight medial and lateral rotation about the axis of the lower leg in the flexed position. The knee joint is called "mobile" because the femur and lateral meniscus move[28]: 399 over the tibia during rotation, while the femur rolls and glides over both menisci during extension-flexion.[10]: 212–213
The center of the transverse axis of the extension/flexion movements is located where both collateral ligaments and both cruciate ligaments intersect. This center moves upward and backward during flexion, while the distance between the center and the articular surfaces of the femur changes dynamically with the decreasing curvature of the femoral condyles. The total range of motion is dependent on several parameters such as soft-tissue restraints, active insufficiency, and hamstring tightness.[28]: 398
| Extension 5–10° | Flexion 120–150° |
|---|---|
| Quadriceps (with some assistance from the Tensor fasciae latae) |
(In order of importance) Semimembranosus Semitendinosus Biceps femoris Gracilis Sartorius Popliteus Gastrocnemius |
| Internal rotation* 10° | External rotation* 30–40° |
| (In order of importance) Semimembranosus Semitendinosus Gracilis Sartorius Popliteus |
Biceps femoris |
| *(knee flexed 90°) | |
Extended position
[edit]With the knee extended, both the lateral and medial collateral ligaments, as well as the anterior part of the anterior cruciate ligament, are taut. During extension, the femoral condyles glide and roll into a position which causes the complete unfolding of the tibial collateral ligament. During the last 10° of extension, an obligatory terminal rotation is triggered in which the knee is rotated medially 5°. The final rotation is produced by a lateral rotation of the tibia in the non-weight-bearing leg, and by a medial rotation of the femur in the weight-bearing leg. This terminal rotation is made possible by the shape of the medial femoral condyle, assisted by contraction of the popliteus muscle and the iliotibial tract and is caused by the stretching of the anterior cruciate ligament. Both cruciate ligaments are slightly unwound and both lateral ligaments become taut.[10]: 212
Flexed position
[edit]In the flexed position, the collateral ligaments are relaxed while the cruciate ligaments are taut. Rotation is controlled by the twisted cruciate ligaments; the two ligaments get twisted around each other during medial rotation of the tibia—which reduces the amount of rotation possible—while they become unwound during lateral rotation of the tibia. Because of the oblique position of the cruciate ligaments, at least a part of one of them is always tense and these ligaments control the joint as the collateral ligaments are relaxed. Furthermore, the dorsal fibers of the tibial collateral ligament become tensed during extreme medial rotation and the ligament also reduces the lateral rotation to 45–60°.[10]: 212
Clinical significance
[edit]
Knee pain is caused by trauma, misalignment, degeneration, and conditions producing arthritis.[29] The most common knee disorder is generally known as patellofemoral syndrome.[29] The majority of minor cases of knee pain can be treated at home with rest and ice, but more serious injuries do require surgical care.[29]
One form of patellofemoral syndrome involves a tissue-related problem that creates pressure and irritation in the knee between the patella and the trochlea (patellar compression syndrome), which causes pain. The second major class of knee disorder involves a tear, slippage, or dislocation that impairs the structural ability of the knee to balance the leg (patellofemoral instability syndrome). Patellofemoral instability syndrome may cause either pain, a sense of poor balance, or both.[29]
Prepatellar bursitis also known as housemaid's knee is painful inflammation of the prepatellar bursa (a frontal knee bursa) often brought about by occupational activity such as roofing.
Age also contributes to disorders of the knee. Particularly in older people, knee pain frequently arises due to osteoarthritis. In addition, weakening of tissues around the knee may contribute to the problem.[30] Patellofemoral instability may relate to hip abnormalities or to tightness of surrounding ligaments.[29]
Cartilage lesions can be caused by:
- Accidents (fractures)
- Injuries
- The removal of a meniscus
- Anterior cruciate ligament injury
- Posterior cruciate ligament injury
- Posterolateral corner injury
- Medial knee injuries
- Considerable strain on the knee.
Any kind of work during which the knees undergo heavy stress may also be detrimental to cartilage. This is especially the case in professions in which people frequently have to walk, lift, or squat. Other causes of pain may be excessive on, and wear off, the knees, in combination with such things as muscle weakness and overweight.
Common complaints:
- A painful, blocked, locked or swollen knee.
- Sufferers sometimes feel as if their knees are about to give way, or may feel uncertain about their movement.
Overall fitness and knee injury
[edit]Physical fitness is related integrally to the development of knee problems. The same activity such as climbing stairs may cause pain from patellofemoral compression for someone who is physically unfit, but not for someone else (or even for that person at a different time). Obesity is another major contributor to knee pain. For instance, a 30-year-old woman who weighed 120 pounds (54 kg) at age 18 years, before her three pregnancies, and now weighs 285 pounds (129 kg), had added 660 pounds (300 kg) of force across her patellofemoral joint with each step.[31]
Common injuries due to physical activity
[edit]
In sports that place great pressure on the knees, especially with twisting forces, it is common to tear one or more ligaments or cartilages. Some of the most common knee injuries are those to the medial side: medial knee injuries.[32]
Anterior cruciate ligament injury
[edit]The anterior cruciate ligament is the most commonly injured ligament of the knee. The injury is common during sports. Twisting of the knee is a common cause of over-stretching or tearing the ACL. When the ACL is injured a popping sound may be heard, and the leg may suddenly give out. Besides swelling and pain, walking may be painful and the knee will feel unstable. Minor tears of the anterior cruciate ligament may heal over time, but a torn ACL requires surgery. After surgery, recovery is prolonged and low impact exercises are recommended to strengthen the joint.[33]
Torn meniscus injury
[edit]The menisci act as shock absorbers and separate the two ends of bone in the knee joint. There are two menisci in the knee, the medial (inner) and the lateral (outer). When there is torn cartilage, it means that the meniscus has been injured. Meniscus tears occur during sports often when the knee is twisted. Menisci injury may be innocuous and one may be able to walk after a tear, but soon swelling and pain set in. Sometimes the knee will lock while bending. Pain often occurs when one squats. Small meniscus tears are treated conservatively but most large tears require surgery.[34]
Fractures
[edit]
Knee fractures are rare but do occur, especially as a result of a road accident. Knee fractures include a patella fracture, and a type of avulsion fracture called a Segond fracture. There is usually immediate pain and swelling, and a difficulty or inability to stand on the leg. The muscles go into spasm and even the slightest movements are painful. X-rays can easily confirm the injury and surgery will depend on the degree of displacement and type of fracture.
Ruptured tendon
[edit]Tendons usually attach muscle to bone. In the knee the quadriceps and patellar tendon can sometimes tear. The injuries to these tendons occur when there is forceful contraction of the knee. If the tendon is completely torn, bending or extending the leg is impossible. A completely torn tendon requires surgery but a partially torn tendon can be treated with leg immobilization followed by physical therapy.
Overuse
[edit]Overuse injuries of the knee include tendonitis, bursitis, muscle strains, and iliotibial band syndrome. These injuries often develop slowly over weeks or months. Activities that induce pain usually delay healing. Rest, ice and compression do help in most cases. Once the swelling has diminished, heat packs can increase blood supply and promote healing. Most overuse injuries subside with time but can flare up if the activities are quickly resumed.[35] Individuals may reduce the chances of overuse injuries by warming up prior to exercise, by limiting high impact activities and keep their weight under control.[citation needed]
Varus or valgus deformity
[edit]
There are two disorders relating to an abnormal angle in the coronal plane at the level of the knee:
- Genu valgum is a valgus deformity in which the tibia is turned outward in relation to the femur, resulting in a knock-kneed appearance.
- Genu varum is a varus deformity in which the tibia is turned inward in relation to the femur, resulting in a bowlegged deformity.
The degree of varus or valgus deformity can be quantified by the hip-knee-ankle angle,[36] which is an angle between the femoral mechanical axis and the center of the ankle joint.[37] It is normally between 1.0° and 1.5° of varus in adults.[38] Normal ranges are different in children.[39]
-
Hip-knee-ankle angle by age, with 95% prediction interval.[39]
Chronic pain from osteoarthritis
[edit]Knee osteoarthritis is a major cause of pain and disability worldwide, with prevalence estimated at about 4% of the population, particularly among the elderly.[40] Radiofrequency ablation of certain knee nerves is an outpatient procedure to reduce chronic arthritic pain.[14][15][40] Using radiofrequency energy delivered via small electrodes positioned at target genicular nerves, the treatment achieves partial sensory denervation of the joint capsule.[40] Despite the extensive innervation of the knee, specifically targeting the superior lateral, superior medial, and inferior medial genicular nerves has proved to be an effective ablation method for reducing chronic knee pain.[40] In clinical research, such treatment has been shown to produce about 50% less knee pain for up to two years after the procedure.[40]
Surgical interventions
[edit]Before the advent of arthroscopy and arthroscopic surgery, patients having surgery for a torn ACL required at least nine months of rehabilitation, having initially spent several weeks in a full-length plaster cast. With current techniques, such patients may be walking without crutches in two weeks, and playing some sports in a few months.
In addition to developing new surgical procedures, ongoing research is looking into underlying problems which may increase the likelihood of an athlete suffering a severe knee injury. These findings may lead to effective preventive measures, especially in female athletes, who have been shown to be especially vulnerable to ACL tears from relatively minor trauma.
Articular cartilage repair treatment:
- Arthroscopic debridement of the knee (arthroscopic lavage)
- Mosaïc-plasty
- Microfracture (Ice-picking)
- Autologous chondrocyte implantation
- Osteochondral Autograft and Allografts
- PLC Reconstruction
Imaging
[edit]MRI
[edit]Both anterior cruciate ligament (ACL) and posterior cruciate ligaments (PCL) are hypointense on both T1 and T2 weighted images of MRI. However, some high signal striations are often seen at the distal part of the ACL, making ACL higher intensity than PCL on MRI scans.[20]
-
Knee MRI (PD TSE FS sagittal)
-
Knee MRI (T1 TSE sagittal)
-
Knee MRI (sagittal TSE FS)
-
Knee MRI (sagittal T1 TSE)
-
Knee MRI (coronal T2 TSE FS)
-
Knee MRI (traverse PD TSE FS)
-
Knee MRI osteoarthritis (sagittal TSE FS)
-
Knee MRI osteoarthritis (sagittal T1 TSE)
-
Knee MRI osteoarthritis (coronal T2 TSE FS)
-
Knee MRI osteoarthritis (traverse PD TSE FS)
-
Real-time MRI- Knee
-
Knee MR
X-ray
[edit]-
Knee X-ray
-
Knee X-ray (weight bearing)
-
Knee X-ray (weight bearing, flexion)
Illustrations
[edit]-
Cruciate ligaments
-
Left knee-joint from behind, showing interior ligaments.
-
Capsule of right knee-joint (distended). Lateral aspect.
-
Anterior and lateral view of knee.
-
Anterior view of knee.
Other animals
[edit]In humans, the term "knee" refers to the joints between the femur, tibia, and patella, in the leg.
In quadrupeds such as dogs, horses, and mice, the homologous joints between the femur, tibia, and patella, in the hind leg, are known as the stifle joint. Also in quadrupeds, particularly horses, ungulates, and elephants, the layman's term "knee" also commonly refers to the forward-facing joint in the foreleg, the carpus, which is homologous to the human wrist.
In birds, the "knee" is the joint between the femur and tibiotarsus, and also the patella (when present). The layman's term "knee" may also refer to the (lower and often more visible due to not being covered by feathers) joint between the tibiotarsus and tarsometatarsus, which is homologous to the human ankle.
In insects and other animals, the term knee widely refers to any hinge joint.
See also
[edit]- Arthrofibrosis
- Articular cartilage repair
- Chondromalacia patellae
- Fibular collateral ligament
- Geniculum
- Genuflection
- Knee arthritis
- Knee cartilage replacement therapy
- Knee examination
- Kneecapping
- Kneeling
- Knésetja
- Medial collateral ligament
- Partial knee replacement unicompartmental knee arthroplasty
- Posterolateral corner injuries
- Reflex hammer
References
[edit]- ^ Chhajer, Bimal (2006). "Anatomy of Knee". Knee Pain. Fusion Books. pp. 10–11. ISBN 978-81-8419-181-3.
- ^ Kulowski, Jacob (July 1932). "Flexion contracture of the knee". The Journal of Bone and Joint Surgery. 14 (3): 618–663. Archived from the original on 2016-08-03. Retrieved 2015-05-08. Republished as: Kulowski, J (2007). "Flexion contracture of the knee: The mechanics of the muscular contracture and the turnbuckle cast method of treatment; with a review of fifty-five cases. 1932". Clinical Orthopaedics and Related Research. 464: 4–10. doi:10.1097/BLO.0b013e31815760ca. PMID 17975372. S2CID 9932906.
- ^ Rytter, Søren; Egund, Niels; Jensen, Lilli; Bonde, Jens (2009). "Occupational kneeling and radiographic tibiofemoral and patellofemoral osteoarthritis". Journal of Occupational Medicine and Toxicology. 4: 19. doi:10.1186/1745-6673-4-19. PMC 2726153. PMID 19594940.
- ^ Gill TJ, Van de Velde SK, Wing DW, Oh LS, Hosseini A, Li G (2009). "Tibiofemoral and Patellofemoral Kinematics After Reconstruction of an Isolated Posterior Cruciate Ligament Injury: In Vivo Analysis During Lunge". The American Journal of Sports Medicine. 37 (12): 2377–2385. doi:10.1177/0363546509341829. PMC 3832057. PMID 19726621.
- ^ Scott, Jacob; Lee, Ho; Barsoum, Wael; Van Den Bogert, Antonie J. (2007). "The effect of tibiofemoral loading on proximal tibiofibular joint motion". Journal of Anatomy. 211 (5): 647–653. doi:10.1111/j.1469-7580.2007.00803.x. PMC 2375777. PMID 17764523.
- ^ Burgener, Francis A.; Meyers, Steven P.; Tan, Raymond K.; Zaunbauer, Wolfgang (2002). Differential Diagnosis in Magnetic Resonance Imaging. Stuttgart: Thieme. ISBN 978-1588900852. OCLC 48983197., p. 390
- ^ Chahla, Jorge; Moatshe, Gilbert; Dean, Chase S.; LaPrade, Robert F. (2016). "Posterolateral Corner of the Knee: Current Concepts". The Archives of Bone and Joint Surgery. 4 (2): 97–103. PMC 4852053. PMID 27200384.
- ^ "Knee Joint". The Lecturio Medical Concept Library. Retrieved 2021-06-22.
- ^ "Do babies have kneecaps?". HowStuffWorks.com. 2009-02-19. Archived from the original on 2013-03-15.
- ^ a b c d e f g h i j k l m n o p q r s t u v w Platzer, Werner (2004). Color Atlas of Human Anatomy, Vol. 1: Locomotor System (5th ed.). Thieme. pp. 26, 192–252. ISBN 978-1588901590. OCLC 727951508.
- ^ Netter, Frank H. (2013). The Netter collection of medical illustrations. Volume 6, Musculoskeletal system. Part II, Spine and lower limb: a compilation of paintings. Iannotti, Joseph P., Parker, Richard D. (Orthopedist), Machado, Carlos A. G. (2nd ed.). Philadelphia, PA: Elsevier Saunders. ISBN 978-1416063827. OCLC 821699791.
- ^ Reider, B; Marshall, J. L.; Koslin, B; Ring, B; Girgis, F. G. (1981). "The anterior aspect of the knee joint". The Journal of Bone and Joint Surgery. American Volume. 63 (3): 351–356. doi:10.2106/00004623-198163030-00004. PMID 7204430.[permanent dead link]
- ^ a b c d e f g h i Ryan, Stephanie (2011). "Chapter 8". Anatomy for diagnostic imaging (Third ed.). Elsevier Ltd. pp. 289, 292. ISBN 978-0702029714. OCLC 729966424.
- ^ a b Tran J, Peng PW, Lam K, Baig E, Agur AM, Gofeld M (May 2018). "Anatomical Study of the Innervation of Anterior Knee Joint Capsule: Implication for Image-Guided Intervention". Regional Anesthesia and Pain Medicine. 43 (4): 407–414. doi:10.1097/AAP.0000000000000778. PMID 29557887. ProQuest 2720408173.
- ^ a b c Fonkoué L, Behets C, Kouassi JK, et al. (December 2019). "Distribution of sensory nerves supplying the knee joint capsule and implications for genicular blockade and radiofrequency ablation: an anatomical study". Surgical and Radiologic Anatomy. 41 (12): 1461–1471. doi:10.1007/s00276-019-02291-y. PMID 31338537.
- ^ Tran J, Peng PW, Gofeld M, Chan V, Agur AM (February 2019). "Anatomical study of the innervation of posterior knee joint capsule: implication for image-guided intervention". Regional Anesthesia and Pain Medicine. 44 (2): 234–238. doi:10.1136/rapm-2018-000015. PMID 30700618. ProQuest 2553100556.
- ^ "Cartilage". Encyclopaedia Britannica. Retrieved 2021-06-23.
- ^ Gibbon, Anthony. "Knee Anatomy". North Yorkshire Orthopaedic Specialists. Archived from the original on 23 April 2013. Retrieved 6 February 2013.
- ^ Goldman, Lee; Schafer, Andrew I. (2012), Goldman's Cecil Medicine, Elsevier, pp. vii, doi:10.1016/b978-1-4377-1604-7.00513-3
- ^ a b Kam CK, Chee DW, Peh WC (April 2010). "Magnetic resonance imaging of cruciate ligament injuries of the knee". Canadian Association of Radiologists Journal. 61 (2): 80–89. doi:10.1016/j.carj.2009.11.003. PMID 20110155. S2CID 40819119.
- ^ "ACL injury - Symptoms and causes". Mayo Clinic. Retrieved 2022-12-30.
- ^ Diab, Mohammad (1999). Lexicon of Orthopaedic Etymology. Taylor & Francis. ISBN 978-9057025976. OCLC 43779363., p. 200
- ^ "Definition of patellar tendon". MedicineNet.com. Archived from the original on 2013-11-05. Retrieved 2008-12-11.
- ^ Moore, Keith L.; Dalley, Arthur F.; Agur, Anne M. R. (2006). Clinically Oriented Anatomy. Lippincott Williams & Wilkins. p. 594. ISBN 978-0781736398. OCLC 57202439., p. 194
- ^ a b c d e f g h i j k Gosling 2008, p. 273
- ^ a b c Gosling et al. 2008, p. 266
- ^ Shim, S. S.; Leung, G. (July 1986). "Blood supply of the knee joint. A microangiographic study in children and adults". Clinical Orthopaedics and Related Research (208): 119–125. ISSN 0009-921X. PMID 3522019.
- ^ a b c Thieme Atlas of Anatomy: General Anatomy and Musculoskeletal System. New York: Thieme. 2006. ISBN 978-1588904195. OCLC 474717189.
- ^ a b c d e Afra R, Schepsis A (May 28, 2008). "Addressing patellofemoral pathology: Biomechanics and classification". The Journal of Musculoskeletal Medicine. Archived from the original on May 18, 2015.
- ^ Pill SG, Khoury LD, Chin GC, et al. (October 29, 2008). "MRI for evaluating knee pain in older patients: How useful is it?". The Journal of Musculoskeletal Medicine. 25 (11). Archived from the original on May 18, 2015.
- ^ Andrish JT (May 8, 2009). "Sports injuries in weekend warriors: 20 Clinical pearls". The Journal of Musculoskeletal Medicine. 26 (5). Archived from the original on May 18, 2015.
- ^ Campbell, Willis C.; Canale, S. T.; Beaty, James H. (2008). Campbell's Operative Orthopedics (11th ed.). Philadelphia: Mosby/Elsevier.
- ^ Knee pain and injuries Archived 2009-12-11 at the Wayback Machine About sports online portal. 2010-01-26
- ^ Tandeter HB, Shvartzman P, Stevens MA (1 December 1999). "Acute knee injuries: use of decision rules for selective radiograph ordering". Am Fam Physician. 60 (9): 2599–2608. PMID 10605994.
- ^ "Knee injuries and disorders". MedLine Plus. 28 June 2016. Archived from the original on 2016-07-04.
- ^ W-Dahl, Annette; Toksvig-Larsen, Sören; Roos, Ewa M (2009). "Association between knee alignment and knee pain in patients surgically treated for medial knee osteoarthritis by high tibial osteotomy. A one year follow-up study". BMC Musculoskeletal Disorders. 10 (1): 154. doi:10.1186/1471-2474-10-154. ISSN 1471-2474. PMC 2796991. PMID 19995425.
- ^ Cherian, Jeffrey J.; Kapadia, Bhaveen H.; Banerjee, Samik; Jauregui, Julio J.; Issa, Kimona; Mont, Michael A. (2014). "Mechanical, Anatomical, and Kinematic Axis in TKA: Concepts and Practical Applications". Current Reviews in Musculoskeletal Medicine. 7 (2): 89–95. doi:10.1007/s12178-014-9218-y. ISSN 1935-973X. PMC 4092202. PMID 24671469.
- ^ Sheehy L, Felson D, Zhang Y, Niu J, Lam YM, Segal N, et al. (2011). "Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study". Osteoarthritis and Cartilage. 19 (1): 58–64. doi:10.1016/j.joca.2010.09.011. ISSN 1063-4584. PMC 3038654. PMID 20950695.
- ^ a b Sabharwal, Sanjeev; Zhao, Caixia (2009). "The Hip-Knee-Ankle Angle in Children: Reference Values Based on a Full-Length Standing Radiograph". The Journal of Bone and Joint Surgery, American Volume. 91 (10): 2461–2468. doi:10.2106/JBJS.I.00015. ISSN 0021-9355. PMID 19797583.
- ^ a b c d e Conger A, Gililland J, Anderson L, et al. (July 2021). "Genicular Nerve Radiofrequency Ablation for the Treatment of Painful Knee Osteoarthritis: Current Evidence and Future Directions". Pain Medicine. 22 (Suppl 1): S20 – S23. doi:10.1093/pm/pnab129. PMID 34308957.
External links
[edit] Media related to Knee at Wikimedia Commons
Media related to Knee at Wikimedia Commons




![Hip-knee-ankle angle by age, with 95% prediction interval.[39]](http://upload.wikimedia.org/wikipedia/commons/thumb/0/07/Hip-knee-ankle_angle_by_age.png/192px-Hip-knee-ankle_angle_by_age.png)










