Alzheimer's disease in the Hispanic/Latino population
Alzheimer's disease (AD) in the Hispanic/Latino population is becoming a topic of interest in AD research as Hispanics and Latinos are disproportionately affected by Alzheimer's Disease and underrepresented in clinical research.[1][2] AD is a neurodegenerative disease, characterized by the presence of amyloid-beta plaques and neurofibrillary tangles, that causes memory loss and cognitive decline in its patients.[3] However, pathology and symptoms have been shown to manifest differently in Hispanic/Latinos, as different neuroinflammatory markers are expressed and cognitive decline is more pronounced.[4][5] Additionally, there is a large genetic component of AD, with mutations in the amyloid precursor protein (APP), Apolipoprotein E APOE), presenilin 1 (PSEN1), bridging Integrator 1 (BIN1), SORL1, and Clusterin (CLU) genes increasing one's risk to develop the condition.[6][7][8] However, research has shown these high-risk genes have a different effect on Hispanics and Latinos then they do in other racial and ethnic groups.[9] Additionally, this population experiences higher rates of comorbidities, that increase their risk of developing AD.[9] Hispanics and Latinos also face socioeconomic and cultural factors, such as low income and a language barrier, that affect their ability to engage in clinical trials and receive proper care.[10][2]
Alzheimer's disease
[edit]
Alzheimer's disease is the most common form of dementia, accounting for 60% of all cases, and is the sixth leading cause of death in the elderly.[11][12] The disease typically presents itself with intracellular aggregation of hyper-phosphorylated tau, forming neurofibrillary tangles (NFTs), and the extracellular aggregation of amyloid beta (Aβ), forming neuritic plaques.[7] As of 2020, 5.4 million Americans have been diagnosed with Alzheimer's disease, and this number is projected to reach 15-22 million by 2050.[6][10] Hispanics and Latinos account for 55 million of the population and this population is projected to rise to 97 million, accounting for 25% of the U.S. population, in 2050.[10]
Hispanic/Latino population
[edit]Hispanics and Latinos make up 18% of the U.S. population, however, they are underrepresented in clinical research.[2][13] The National Institute of Health (NIH) reported that Hispanic and Latinos accounted for less than 8% of reported clinical trial participants.[10] One proposed reason for the lack of representation is that the Hispanic/Latino population includes many people from different countries, and with this diverse background come different characteristics and comorbidities associated with AD.[10] Hispanic and Latinos have a higher prevalence of AD compared to White non-Hispanics.[10][2] Studies estimate that 12% of older Hispanic and Latino adults were diagnosed with AD, the highest proportion compared to all other ethnic groups.[2] Hispanic and Latinos are the fastest-growing population in the U.S., and Hispanic/Latino seniors, those who are 65 and older, are expected to have the largest rise in AD and dementia cases compared to other populations, reaching 3.5 million by 2060.[10] In 2011 the National Alzheimer's Disease Project Act was signed into law.[2] The goal of this act was for The National Institute of Aging to accelerate research and clinical care of patients with AD; this act also has the benefit of seeking to improve the inclusion of underrepresented populations in AD research and clinical trials.[2] It is important to note that this neurodegenerative disease varies across all ethnic groups. Studies show that Latinos are up to one-and-a-half times more likely to develop Alzheimer's than non-Latino whites. [14]
Types
[edit]There exist two types of Alzheimer's disease: familial Alzheimer's disease, also called early-onset Alzheimer's disease (EOAD), and sporadic Alzheimer's disease, also called late-onset Alzheimer's disease (LOAD).[6][15] EOAD is the less common of the two, accounting for 5-10%, and patients with EOAD are typically diagnosed with familial AD before they turn 65 years old.[6][15] LOAD is more common and accounts for 90% of AD cases and its patients experience onset after they turn 65.[12][7] EOAD has been shown to have 2 types of inheritance patterns: mendelian (mEOAD) and non-mendelian (nmEOAD, sporadic) patterns.[6] The three main genes that implicated in familial AD are amyloid precursor protein (APP), Presenilin-1 (PSEN-1), presenilin-2 (PSEN-2).[6][15][7] Onset of sporadic AD has both genetic and environmental risk factors.[15] Some genes of interest in LOAD are the APOE gene, specifically the ApoE4 allele, bridging Integrator 1 (BIN1), SORL1, and clusterin (CLU).[6][7][16][17][8]
Pathology and symptoms
[edit]Amyloid beta plaques and neurofibrillary tangles
[edit]
Neuritic plaques and neurofibrillary Tangles (NFTs) are the main pathological component of AD.[7][18] Neuritic plaques are composed mainly of the peptide Aβ, but also include other components.[19] APP is processed through either of two pathways, the first is termed the amyloidogenic pathway and produces Aβ.[19] The second pathway is the non-amyloidogenic pathway and does not produce Aβ.[19] In the amyloidogenic pathway, APP (the parent protein) is trafficked to endosomes, cleaved by beta-secretase (BACE), after which it moves back to the cell surface to be cleaved by gamma secretase thus releasing the Aβ peptide.[7][8][18][19] This form of APP processing produces multiple Aβ peptides, of which Aβ40 and Aβ42 peptide are most abundantly produced.[7][20] APP can also be cleaved by alpha and gamma-secretase and undergo non-amyloidogenic processing.[18][20] NFTs form when the tau protein, which is involved in microtubule stability, is hyperphosphorylated, dissociates from microtubules and then aggregates with other p-tau monomers forming tau oligomers, fibrils and eventually NFTs.[7] These types of pathologies do not differ across ethnic groups.[7]
Chronic inflammation
[edit]Neuroinflammation is another pathological component of AD pathology, and is associated with an increase in levels of inflammatory markers.[7][21] Researchers have also identified many genes linked to immune function that are risk factors for AD, such as TREM2.[21] TREM2 are highly expressed in microglia, the immune cell of the brain, tying the progression of AD with dysfunction in microglial activity.[22] Neuroinflammation, Aβ and tau pathologies interact in Alzheimer's disease, and their progress can be monitored with biomarkers.[21] For example, studies have found the neuroinflammatory marker YKL-40 in the cerebrospinal fluid (CSF) of AD patients.[17][4] This protein increases years before the onset of AD symptoms and correlates with other neurodegenerative biomarkers, which suggests a potential to predict disease progression.[4] While YKL-40 has not been shown to associate with the APOE -ε4 allele, there is research to link this biomarker to AD in the Hispanic population.[4]
Neurodegeneration
[edit]Along with the plaques and inflammation, patients with AD also suffer from neurodegeneration, characterized by loss of neurons and synapses (the communication tool for neurons).[18][7] As a result, the entire brain shrinks in volume (termed brain atrophy), the ventricles grow larger, and the hippocampus and cortex shrink in size.[7][18] As all these pathologies progress, patients begin to experience a decline in memory, cognitive abilities, and independence. The accumulation of neurofibrillary tangles and loss of synaptic fields correlate most closely with cognitive loss.[7]
Mild cognitive impairment
[edit]Mild cognitive impairment (MCI) precedes the overt diagnosis of AD.[3][23][24] To be diagnosed with MCI a patient must show memory impairment, a progressive decline in cognitive abilities without presenting symptoms of Parkinson's disease, cerebrovascular diseases, and behavioral or language disorders.[24] Studies show that older Hispanic/Latinos exhibit a higher prevalence of dementia than caucasians.[5][25] Demographic and linguistic factors can prevent a proper MCI diagnosis.[26][27] For instance, subjects for whom English might not be the primary language require use of a translator to perform the cognitive testing, which could affect testing results, but such experimental weaknesses are frequently not described.[26][27]

Brain imaging
[edit]Positron emission tomography (PET) is a brain imaging technique that uses a small amount of radioactive substance, called a tracer, to measure energy use or a specific molecule in different brain regions.[28] In AD research, tracers can be used to detect neuritic plaques (containing Aβ) and tau. Depending on the tracer used, the signal can be used to determine the presence of neuritic plaques and NFTs.[28]

Biomarkers
[edit]Establishing biomarkers for the early detection of AD is an ongoing are of research because pathological changes occur years before symptoms become apparent.[7][17] Common biomarkers for AD include amyloid beta and hyperphosphorylated tau, both of which can be found in brain tissue and cerebrospinal fluid (CSF).[7] Aβ provides a biomarker of neuritic plaques, which form when APP cleavage results in an increase in the Aβ42/Aβ40 ratio.[7] Hyperphosphorylated tau serves as a biomarker of neurofibrillary tangles (NFTs), with the presence of NFTs indicating a disruption in microtubule stability and neuronal injury.[7] Researchers have begun investigating other markers in the CSF, such as markers of neuronal injury, like Visinin-Like-Protein-1 (VILIP-1), YKL-40, and Neurogranin (NGRN).[17] Due to the low use of CSF sampling in most countries, efforts have been made to study biomarkers in blood.[17] Through work on blood biomarkers, researchers have been able to find proteins that are elevated in AD patients and have predictive potential.[17] The predictive potential of these plasma markers increases further when coupled with the presence of genetic risk factors, such as the APOE E4 allele.[17] Examples of plasma biomarkers include interleukin, TGF, and micro-RNA.[17]
Genetic risk factors being considered for integration with biomarkers includes ApoE, PSEN1, Bin1, CLU, and SORL1.[16][8][7][6]
APOE gene
[edit]
Apolipoprotein E (APOE) is a lipoprotein, composed of 299 amino acids, that is expressed throughout the body but particularly important in the brain where it is involved in cholesterol metabolism, specifically in the intracellular and extracellular transport, delivery, and distribution.[16] APOE associates with high-density lipoproteins (HDL).[12] The gene for APOE is located on chromosome 19 and exhibits polymorphisms in the population defined by three alleles of APOE: 𝜀2, 𝜀3, and 𝜀4.[16][19] These alleles differ by only two single nucleotide polymorphisms in exon 4, rs429358 and rs7412 (amino-acid position 112 and 158).[7][16] APOE𝜀3 is the more common of the three and is present in 50-90% of the general population.[16][19] APOE 𝜀4 is the most common risk factor for LOAD, increasing genetic risk up to 33-fold, depending on the population (see the table below).[20] Over 50% of LOAD patients have the 𝜀4 allele and that having even one copy of the 𝜀4 allele increases the risk of developing Alzheimer's by a factor of 4.[7][6][16][19] APOE 𝜀2 has been shown to have a neuroprotective effect with carriers of the allele showing a lower prevalence of AD.[16][19] The neuropathological effects of APOE ε4 are pleiotropic; APOE ε4 impairs uptake of cholesterol by neurons, promotes microglial dysfunction, promotes beta-amyloid aggregation and is increases cerebral angiopathy (CAA).[7][12][19] The increased incidence of AD associated with the APOE ε4 allele has been proposed to be directly linked to Aβ because it modulates Aβ aggregation and clearance, although increasing evidence points to a multitude of actions.[29]
| Population | APOE𝜀4 Association with AD |
|---|---|
| Caucasian | 12.5 |
| African Americans | 5.7 |
| Hispanic | 2.2 |
| Japanese | 33.1 |
While extensive research has been done on the APOE4 gene, more information is available for caucasians than for other ethnic and racial groups.[2] The research focusing on the Hispanic and Latino population, suggests that race is a key variable in assessing the risk of carrying the APOE ε4 allele in developing AD.[6][10][16] Genetic studies of Hispanic and Latino populations, show a lower risk of developing AD for individuals with the APOE ε4 than observed in Caucasians.[10] For instance, the prevalence of AD seen in Caribbean Hispanics, compared to White Non-Hispanics, appears to be independent of APOE genotype.[10] Our understanding of ApoE ε4 continues to evolve, though, as Hispanic and Latino representation in research increases leading to larger sample sizes and improved population stratification .[10][2][13]
PSEN1 gene
[edit]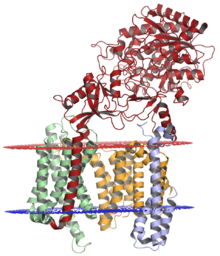

Presenilin 1 (PSEN1) is the catalytic subunit of the transmembrane protein complex gamma-secretase.[30][12] This protein cleaves amyloid precursor protein (APP), after beta-secretase cleavage, to produce Amyloid beta.[12][30] The gene for PSEN1 is located on chromosome 14, q24.2, and consists of 12 exons that encode a 467-amino-acid protein that is predicted to traverse the membrane 9 times.[12] Over 200 pathogenic mutations of this protein exist, many of which account for 18% to 50% of autosomal dominant EOAD cases.[16][12][31] PSEN1 mutations increase the risk of developing AD by increasing the production of amyloid beta-42, compared to amyloid beta-40.[12] Unlike APOE4, PSEN1 mutations tend to have a clear pathological effect in Hispanics and Latinos and tend to express region-specific mutations.[10] Puerto Ricans have a G206A mutation that causes familial AD, Cuban families diagnosed with EAOD commonly exhibit a L174M, mutation, Mexican families exhibit L171P and A431E mutations, and Colombian families exhibit an E280A mutation (particularly in the municipality of Yarumal).[10][32]
BIN1 gene
[edit]Bridging Integrator 1 (BIN1) is a widely expressed Bin-Amphiphysin-Rvs (BAR) adaptor protein that is located on chromosome 2, q14.3, and contains 20 exons.[20] BIN1 mainly regulates clathrin-mediated endocytosis. Due to a large number of exons, this gene is subject to alternative splicing, with the major forms varying in the splicing of exons 6a, 10, 12, and 13.[20] Genetic studies indicate that dysfunction in BIN1 is the second most important risk factor for AD.[7][20] The mechanism through which BIN1 contributes to AD, though, is unclear. Studies suggest a range of possible reasons that BIN1 is associated with AD including interactions of BIN1 with the microtubule-associated proteins (i.e. CLIP170), endosomal trafficking of APP and APOE by BIN1, and BIN1 mediated regulation of inflammation through the expression of indoleamine 2,3-dioxygenase (IDO1).[20] The interaction of BIN1 and tau might also be important because elevated levels of BIN1 are associated with increased AD risk through tau load; this result is suggested because of studies of the functional rs59335482 variant.[20] Additionally, endocytic trafficking of APP by BIN1 could be important because trafficking determines if APP will undergo the non-amyloidogenic or the amyloidogenic pathway.[20] For example, if APP is transported to the endosome, it will likely be cleaved by beta-secretase and undergo amyloidogenic processing, but if it accumulates on the cell surface it will be likely cleaved by alpha-secretase and undergo non-amyloidogenic processing.[20] Lastly, BIN1 facilitates the kynurenine pathway of tryptophan metabolism by regulating the expression of the rate-limiting enzyme indoleamine 2,3-dioxygenase (IDO1).[20] For the IDO1 mechanism, increased BIN1 expression could increase levels of a toxic tryptophan derivative IDO1.[20] These metabolites have been suggested to be involved in AD pathology and cognitive decline, as they co-localize with the plaques and NFTs in patient brains.[20]
Genome-wide association studies (GWAS) in the Hispanic/Latino population indicate that polymorphisms in the BIN1, ABAC7 and CD2AP genes are more significant in Caribbean Hispanics.[8] For instance, one BIN1 mutation that has been explored in this Caribbean Hispanics is rs13426725.[20] Other variants that increase the risk of AD include rs6733839.[20]
SORL1 gene
[edit]
Sortilin-related receptor 1 (SORL1) is a 250-kDa membrane protein with seven distinct domains that make it a member of two receptor families: the low-density lipoprotein receptor (LDLR) family of ApoE receptors and the vacuolar protein sorting 10 (VPS10) domain receptor family.[29][8] In humans, the SORL1 gene is located on chromosome 11, specifically q232-q24.2.[29] As a protein SORL1 is highly expressed in the brain.[29] SORL1 is an intracellular protein that is expressed in early endosomes and the trans-Golgi network.[29] SORL1 plays an important role in the intracellular trafficking of APP.[29][8] The protein can bind to APP expressed in endosomes and allow APP to be transported back to the cell surface, which prevents amyloidogenic processing and the production of cytotoxic Aβ40 and Aβ42.[29][33] Moreover, SORL1 has been shown to facilitate cholesterol transport through its tendency to bind to APOE-lipoprotein complexes.[29] Strong disease-linked polymorphisms in SORL1 combine with its role in APP trafficking render SORL1 a biomarker of strong interest for LOAD.[29][33] Decreased levels of SORL1 transcript and protein have been observed in the brains of AD patients.[29][33]
Analysis of SORL1 polymorphisms in the Hispanic/Latino population using GWAS and whole-genome sequencing (WGS) have shown that several SORL1 mutations are seen in Caribbean Hispanics.[8][33] Two rare polymorphisms in SORL1 associated with AD were observed in this population, rs117260922-E270K and rs143571823-T947M, as well as a common variant (rs2298813-A528T) .[8][33] These polymorphisms are not specific to Hispanics/Latinos as they are also observed in non-Hispanic white individuals.[8]
ATP binding cassette transporters
[edit]
Adenosine triphosphate (ATP)-binding cassette transporters are a large family of ABC transporters that regulates the efflux of cholesterol in neuronal cells.[7] Two members of the ATP binding cassette transporter family have been implicated in LOAD: ABC Subfamily A Member 1 (ABCA1) and ABC Subfamily A member 7 (ABCA7).[8][6][20] ABCA1 is a 220-240 kDa protein whose gene is located in chromosome 9q31.1[34] Its putative role in AD is tied to its role in stabilizing ApoE lipidation and degrading amyloid beta expressed in the brain.[8][7] ABCA7 exhibits strong genetic linkage to AD; it is involved in lipid and cholesterol processing, as well as immune system function.[35][20] ABCA7 exhibits tighter association with amyloid deposition than ABCA1.[35] The research on ABCA7 mutations in the Hispanic/Latino population is a bit controversial. Some studies propose that mutations in ABCA7 are more common in Caucasian patients, whereas Hispanics/Latinos are more likely to express a BIN1 mutation.[8] But researchers have still found polymorphisms specific to this population, one example being a 44-base pair frameshift deletion in ABCA7 increases AD risk in African Americans and Caribbean Hispanics.[6]
Clusterin
[edit]Clusterin (CLU), also known as apolipoprotein J, is an 82 kDa glycoprotein protein that is located on chromosome 8.[7][36][17] It has multiple physiological functions, some examples being lipid transport, immune modulation, and cell death.[17][36] CLU is known to have the ability to clear Aβ peptides and prevent their aggregation, which suggests that CLU has a neuroprotective effect.[17][36][7] While one might expect AD to be associated with lower levels of a neuroprotective protein, biomarker studies indicate that CLU is upregulated in the plasma, CSF, hippocampus, and cortex of AD patients.[17][36][7] One theory explaining this apparent contradiction is CLU is actually reduced early in life, increasing risk of developing AD.[17] In this scenario, CLU might increase in subjects with AD as a compensatory response to the disease; further research is clearly necessary to clairy this area.[17] However, genetic studies show that CLU is the third most significant risk factor for LOAD, which has propelled extensive genetic research related to CLU and AD.[36] Two CLU variants of interest, that are associated with reduced AD frequency, are rs11136000 and rs9331896.[17] However, little is known about the relationship between CLU and AD risk in the Hispanic/Latino community.[37]
Comorbidities
[edit]Studies have shown that metabolic disorders, such as diabetes, cardiovascular disease, hypertension, obesity, and depression can increase one's risk of developing AD as well as increase the rate at which it progresses.[9][10][38] In the United States, 33% of the total population suffers from a metabolic disorder (i.e. diabetes and hypertension).[10] Hispanic and Latino adults are at an increased risk of developing these conditions compared to Caucasians.[2] As of 2017, it has been reported that 35% of all Latinos suffer from an AD comorbidity, with 17% suffering from diabetes and 25.4% suffering from hypertension.[10] The high prevalence of cardiovascular and metabolic conditions is thought to contribute to the higher risk of Alzheimer's Disease seen in Hispanics and Latinos.[10][2][13][38]
Hypertension
[edit]
Hypertension is a condition characterized by persistently high blood pressure.[39][40] Two measurements are taken to quantify blood pressure: systolic and diastolic blood pressure.[40] A patient is diagnosed as hypertensive when their systolic blood pressure is greater than 140 mmHg or diastolic blood pressure is greater than 90 mmHg. Not many people with hypertension are aware that they have the condition.[40][39] In 2010, 31.1% of adults worldwide had hypertension, but only 45.6% of them were aware they had the condition.[40] Hypertension is more apparent in the Hispanic/Latino population, as in 2008 the incidence rate of hypertension for Hispanic adults aged 45–84 was 65.7%, compared to 56.8% for non-Hispanic whites of the same age.[2][41] Hispanic/Latinos are more likely to be unaware of their condition, compared to non-Hispanics, and be less likely to seek treatment, which increases the risk of developing cardiovascular disease and AD.[41][40] Hypertension can be reduced by lifestyle changes (e.g., weight loss and exercise) and pharmacological intervention.[38][39] Multiple studies suggest that use of antihypertensive drugs might reduce the risk of dementia and AD.[38][19]
Diabetes
[edit]Type-II diabetes is a metabolic condition characterized by high blood sugar and defective insulin secretion by pancreatic β-cells.[42][43] A patient is diagnosed with diabetes when their fasting blood glucose levels are above 7.0 mmol/L (126 mg/dL) or above 11.1 mmol/L (200 mg/dl) two hours after an oral dose of glucose.[43] As with hypertension, diabetes is more common in the Hispanic/Latino population than in the Caucasian population.[44] In the U.S., Hispanic/Latinos are reported to have a diabetes prevalence of 22.6%, compared to 11.3% in non-Hispanic whites.[44] This increased risk is associated with genetic factors, environmental factors (i.e. diet), and socioeconomic status.[41][45] Recently AD has also been characterized as a metabolic disease of glucose regulation, as patients experience alterations in brain insulin responsiveness that leads to oxidative stress and inflammation.[44] Changes in cerebral glucose signaling associated with AD have been proposed to as type three diabetes, although this has not been adopted as an official designation.[44][46] Older diabetic Mexican Americans are twice as likely to develop dementia than those without diabetes.[44] Additionally, the longer a patient is diabetic, the faster the rate of cognitive decline within the same and racial and age group.[44]
Lifestyle
[edit]Alzheimer's can change your life rapidly and it involves stripping away a lot of an individual's abilities. The neurons that are damaged first are those involving memory, language, and thinking. Indvidual's living with this disease may develop changes in mood, personality or behavior and eventually neuronal damage extends to parts of the brain that enable basic bodily functions. [47] Many of the comorbidities for AD can be reduced through lifestyle changes.[40][42] Hypertension can be treated by reducing sodium intake, increasing potassium intake, reducing alcohol consumption, and engaging in at least 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity per week.[40] Similarly, diabetes can also be treated by increasing physical activity and changing diet.[42] The same lifestyle changes are recommended for AD patients.[7]
Hispanics and Latinos in clinical research
[edit]
The terms Latino and Hispanic are used interchangeably in formal and informal settings.[48] The term "Hispanic" specifically denotes those who can trace their ancestry to a Spanish-speaking country, such as Spain and most of Latin America, the exceptions being Brazil, Guyana, Suriname, and French Guiana.[10] The term "Latino" denotes those who can trace their ancestry to Latin America and the Caribbean.[10] The diversity among Hispanic and Latino groups has led to proposals that the Latino/Hispanic population in the U.S. should not be treated as a homogenous group, and also to define subgroups based on their country of origin.[2] The Latino/Hispanic community has recently been open to wanting to learn more about Alzheimer's Disease but because of they limited resources they aren't able to participate in clinical research.[49]
Socioeconomic status
[edit]The socioeconomic status of the Hispanic/Latino population is thought to contribute to their low participation in clinical trials.[13][2][10] In the U.S., the income and socioeconomic status of Hispanics and Latinos are lower when compared to White Non-Hispanics.[10] In 2015, a study reported that 25% of the Hispanic/Latino population lives in poverty and their median family income was $17,800 lower than their white counterparts.[10] The Hispanic/Latino community have grown the understand the affect Alzheimer has had on their community. A need for care was found to have been associated with education level and be a leading contributor to disability among older people. This shows significant implications for the economy and overall burden caregivers have to take on.[50]
Studies from 2017 showed that the difference in income is present across many income brackets, with only 38.6% of Latinos reporting a household income between $50,000 and $149,999, in comparison to 45.6% of Non-Hispanic whites.[10] A similar trend was seen with levels of higher education and medical literacy attained by Hispanics and Latinos.[10][2] As of 2013, it was reported that 22% of Latino adults (25 years and over) had earned an associate degree or higher, compared to the 46% seen in White Non-Hispanics.[10] This trend is also seen with advanced degrees, as Latinos only account for 7% of Master's degrees and 1% Doctorate degrees awarded in the U.S.[10] The lower measures of socioeconomic achievement and education level have been proposed to be associated with high mortality and dementia rates.[2][10][13] In contrast, high educational levels are correlated with lower rates of dementia.[7]
Hispanic and Latinos that are 65 years and older make up one of the largest groups of uninsured individuals in the U.S.[2] This makes it difficult for these seniors to obtain the clinical care necessary for management of AD.[7][6][2] The cost of care for insured patients 65 years and older was estimated to be $25,213 per person, compared to the estimated $7750 for senior patients without AD.[51] Increasing efforts are being made to include minorities in clinical research, for instance by providing travel support for participants.[13][10]
| Payment Source | Cost in Billions ($) |
|---|---|
| Medicare | $155 |
| Medicaid | $51 |
| Out of Pocket | $66 |
| Other | $33 |
| TOTAL | $305 |
Language barrier
[edit]Putative language barriers can also interfere with healthcare for the Hispanic and Latino community. Clinical trials can require participants to be fluent in English, which can potentially exclude older Hispanic and Latino subjects, who might not be fluent in English.[10][2] Only 40% of the older generation, Latinos over the age of 69, are fluent.[10] Proficiency in English is less of an issue for younger Latinos, with 90% of the population between the ages of 5 and 17 speaking the language fluently.[10] Weak communication between physician and patient can also impair medical care.[2][10] For instance, this issue occurs with clinical notes, which are typically translated from the English version of the same document for Spanish-speaking individuals.[2] The medical community is attempting to address this issue by recruiting staff and physicians able to communicate with participants in their native language, as well as providing training on cultural sensitivity.[10][13]
See also
[edit]References
[edit]- ^ Marquez, David X.; Perez, Adriana; Johnson, Julene K.; Jaldin, Michelle; Pinto, Juan; Keiser, Sahru; Tran, Thi; Martinez, Paula; Guerrero, Javier; Portacolone, Elena (26 July 2022). "Increasing engagement of Hispanics/Latinos in clinical trials on Alzheimer's disease and related dementias". Alzheimer's & Dementia: Translational Research & Clinical Interventions. 8 (1): e12331. doi:10.1002/trc2.12331. ISSN 2352-8737. PMC 9322823. PMID 35910673.
- ^ a b c d e f g h i j k l m n o p q r s t u Massett, Holly A.; Mitchell, Alexandra K.; Alley, Leah; Simoneau, Elizabeth; Burke, Panne; Han, Sae H.; Gallop-Goodman, Gerda; McGowan, Melissa (2021-06-29). Gleason, Carey (ed.). "Facilitators, Challenges, and Messaging Strategies for Hispanic/Latino Populations Participating in Alzheimer's Disease and Related Dementias Clinical Research: A Literature Review". Journal of Alzheimer's Disease. 82 (1): 107–127. doi:10.3233/JAD-201463. PMID 33998537. S2CID 234745473.
- ^ a b Goedert, Michel; Spillantini, Maria Grazia (2006-11-03). "A Century of Alzheimer's Disease". Science. 314 (5800): 777–781. Bibcode:2006Sci...314..777G. doi:10.1126/science.1132814. ISSN 0036-8075. PMID 17082447. S2CID 13906986.
- ^ a b c d Baldacci, Filippo; Lista, Simone; Palermo, Giovanni; Giorgi, Filippo Sean; Vergallo, Andrea; Hampel, Harald (2019-07-03). "The neuroinflammatory biomarker YKL-40 for neurodegenerative diseases: advances in development". Expert Review of Proteomics. 16 (7): 593–600. doi:10.1080/14789450.2019.1628643. ISSN 1478-9450. PMID 31195846. S2CID 189813489.
- ^ a b González, Hector M.; Tarraf, Wassim; Fornage, Myriam; González, Kevin A.; Chai, Albert; Youngblood, Marston; Abreu, Maria de los Angeles; Zeng, Donglin; Thomas, Sonia; Talavera, Gregory A.; Gallo, Linda C.; Kaplan, Robert; Daviglus, Martha L.; Schneiderman, Neil (2019-12-01). "A research framework for cognitive aging and Alzheimer's disease among diverse US Latinos: Design and implementation of the Hispanic Community Health Study/Study of Latinos—Investigation of Neurocognitive Aging (SOL-INCA)". Alzheimer's & Dementia. 15 (12): 1624–1632. doi:10.1016/j.jalz.2019.08.192. ISSN 1552-5260. PMC 6925624. PMID 31759880.
- ^ a b c d e f g h i j k l m Reitz, Christiane; Rogaeva, Ekaterina; Beecham, Gary W. (2020-10-06). "Late-onset vs nonmendelian early-onset Alzheimer disease". Neurology: Genetics. 6 (5): e512. doi:10.1212/NXG.0000000000000512. ISSN 2376-7839. PMC 7673282. PMID 33225065.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae Breijyeh, Zeinab; Karaman, Rafik (2020-12-08). "Comprehensive Review on Alzheimer's Disease: Causes and Treatment". Molecules. 25 (24): 5789. doi:10.3390/molecules25245789. ISSN 1420-3049. PMC 7764106. PMID 33302541.
- ^ a b c d e f g h i j k l m Tosto, Giuseppe; Reitz, Christiane (2016-12-01). "Genomics of Alzheimer's disease: Value of high-throughput genomic technologies to dissect its etiology". Molecular and Cellular Probes. Genetics of multifactorial diseases. 30 (6): 397–403. doi:10.1016/j.mcp.2016.09.001. ISSN 0890-8508. PMID 27618776.
- ^ a b c d Liu, Chia-Chen; Kanekiyo, Takahisa; Xu, Huaxi; Bu, Guojun (February 2013). "Apolipoprotein E and Alzheimer disease: risk, mechanisms, and therapy". Nature Reviews. Neurology. 9 (2): 106–118. doi:10.1038/nrneurol.2012.263. ISSN 1759-4758. PMC 3726719. PMID 23296339.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag Vega, Irving E.; Cabrera, Laura Y.; Wygant, Cassandra M.; Velez-Ortiz, Daniel; Counts, Scott E. (2017-06-23). Abisambra, Jose (ed.). "Alzheimer's Disease in the Latino Community: Intersection of Genetics and Social Determinants of Health". Journal of Alzheimer's Disease. 58 (4): 979–992. doi:10.3233/JAD-161261. PMC 5874398. PMID 28527211.
- ^ Nazha, Bassel; Mishra, Manoj; Pentz, Rebecca; Owonikoko, Taofeek K. (2019-05-01). "Enrollment of Racial Minorities in Clinical Trials: Old Problem Assumes New Urgency in the Age of Immunotherapy". American Society of Clinical Oncology Educational Book. 39 (39): 3–10. doi:10.1200/EDBK_100021. ISSN 1548-8748. PMID 31099618. S2CID 157059400.
- ^ a b c d e f g h i Bekris, Lynn M.; Yu, Chang-En; Bird, Thomas D.; Tsuang, Debby W. (24 February 2011). "Genetics of Alzheimer Disease". Journal of Geriatric Psychiatry and Neurology. 23 (4): 213–227. doi:10.1177/0891988710383571. ISSN 0891-9887. PMC 3044597. PMID 21045163.
- ^ a b c d e f g Konkel, Lindsey (1 December 2015). "Racial and Ethnic Disparities in Research Studies: The Challenge of Creating More Diverse Cohorts". Environmental Health Perspectives. 123 (12): A297–A302. doi:10.1289/ehp.123-A297. ISSN 0091-6765. PMC 4670264. PMID 26625444.
- ^ Manuel, G., & Patel, A. (2020). Alzheimer's Disease and Related Dementias in Hispanic and Latin Populations: A Review.* Journal of Alzheimer's Disease*, 76(4), 1219-1232. https://doi.org/10.3233/JAD-200514
- ^ a b c d Piaceri, Irene; Nacmias, Benedetta; Sorbi, Sandro (2013-01-01). "Genetics of familial and sporadic Alzheimer's disease". Frontiers in Bioscience. 5 (1): 167–177. doi:10.2741/E605. ISSN 1945-0494. PMID 23276979.
- ^ a b c d e f g h i j Sun, Qiying; Xie, Nina; Tang, Beisha; Li, Rena; Shen, Yong (2017). "Alzheimer's Disease: From Genetic Variants to the Distinct Pathological Mechanisms". Frontiers in Molecular Neuroscience. 10: 319. doi:10.3389/fnmol.2017.00319. ISSN 1662-5099. PMC 5635057. PMID 29056900.
- ^ a b c d e f g h i j k l m n o p Huynh, Rose Ann; Mohan, Chandra (2017). "Alzheimer's Disease: Biomarkers in the Genome, Blood, and Cerebrospinal Fluid". Frontiers in Neurology. 8: 102. doi:10.3389/fneur.2017.00102. ISSN 1664-2295. PMC 5357660. PMID 28373857.
- ^ a b c d e "What Happens to the Brain in Alzheimer's Disease?". National Institute on Aging. Retrieved 2022-12-05.
- ^ a b c d e f g h i j Scheltens, Philip; De Strooper, Bart; Kivipelto, Miia; Holstege, Henne; Chételat, Gael; Teunissen, Charlotte E.; Cummings, Jeffrey; van der Flier, Wiesje M. (2021-04-24). "Alzheimer's disease". Lancet. 397 (10284): 1577–1590. doi:10.1016/S0140-6736(20)32205-4. ISSN 1474-547X. PMC 8354300. PMID 33667416.
- ^ a b c d e f g h i j k l m n o p q Tan, Meng-Shan; Yu, Jin-Tai; Tan, Lan (2013-10-01). "Bridging integrator 1 (BIN1): form, function, and Alzheimer's disease". Trends in Molecular Medicine. 19 (10): 594–603. doi:10.1016/j.molmed.2013.06.004. ISSN 1471-4914. PMID 23871436.
- ^ a b c Leng, Fangda; Edison, Paul (March 2021). "Neuroinflammation and microglial activation in Alzheimer disease: where do we go from here?". Nature Reviews Neurology. 17 (3): 157–172. doi:10.1038/s41582-020-00435-y. ISSN 1759-4766. PMID 33318676. S2CID 229163795.
- ^ Rohn, Troy T. (2013-03-06). "The Triggering Receptor Expressed on Myeloid Cells 2: "TREM-ming" the Inflammatory Component Associated with Alzheimer's Disease". Oxidative Medicine and Cellular Longevity. 2013: e860959. doi:10.1155/2013/860959. ISSN 1942-0900. PMC 3606781. PMID 23533697.
- ^ Li, Lanlan; Yu, Xianfeng; Sheng, Can; Jiang, Xueyan; Zhang, Qi; Han, Ying; Jiang, Jiehui (2022-09-15). "A review of brain imaging biomarker genomics in Alzheimer's disease: implementation and perspectives". Translational Neurodegeneration. 11 (1): 42. doi:10.1186/s40035-022-00315-z. ISSN 2047-9158. PMC 9476275. PMID 36109823.
- ^ a b Langa, Kenneth M.; Levine, Deborah A. (2014-12-17). "The diagnosis and management of mild cognitive impairment: a clinical review". JAMA. 312 (23): 2551–2561. doi:10.1001/jama.2014.13806. ISSN 1538-3598. PMC 4269302. PMID 25514304.
- ^ Arévalo, Sandra P.; Kress, Jennifer; Rodriguez, Francisca S. (April 2020). "Validity of Cognitive Assessment Tools for Older Adult Hispanics: A Systematic Review". Journal of the American Geriatrics Society. 68 (4): 882–888. doi:10.1111/jgs.16300. ISSN 1532-5415. PMID 31886524. S2CID 209511214.
- ^ a b Briceño, Emily M.; Mehdipanah, Roshanak; Gonzales, Xavier Fonz; Langa, Kenneth M.; Levine, Deborah A.; Garcia, Nelda M.; Longoria, Ruth; Giordani, Bruno J.; Heeringa, Steven G.; Morgenstern, Lewis B. (13 April 2020). "Neuropsychological assessment of mild cognitive impairment in Latinx adults: A scoping review". Neuropsychology. 34 (5): 493–510. doi:10.1037/neu0000628. ISSN 1931-1559. PMC 8209654. PMID 32281811.
- ^ a b Briceño, E; Mehdipanah, R; Gonzales, X; Langa, K; Levine, D; Garcia, N; Longoria, R; Giordani, B; Heeringa, S; Morgenstern, L (2019-08-30). "Culture and Diagnosis of MCI in Hispanics: A Literature Review". Archives of Clinical Neuropsychology. 34 (7): 1239. doi:10.1093/arclin/acz029.06. ISSN 1873-5843.
- ^ a b "How Biomarkers Help Diagnose Dementia". National Institute on Aging. Retrieved 2022-12-05.
- ^ a b c d e f g h i j Yin, Rui-Hua; Yu, Jin-Tai; Tan, Lan (2015-06-01). "The Role of SORL1 in Alzheimer's Disease". Molecular Neurobiology. 51 (3): 909–918. doi:10.1007/s12035-014-8742-5. ISSN 1559-1182. PMID 24833601. S2CID 16362596.
- ^ a b KHANAHMADI, Mohammad; FARHUD, Dariush D.; MALMIR, Maryam (July 2015). "Genetic of Alzheimer's Disease: A Narrative Review Article". Iranian Journal of Public Health. 44 (7): 892–901. ISSN 2251-6085. PMC 4645760. PMID 26576367.
- ^ Jiang, Haowei; Jayadev, Suman; Lardelli, Michael; Newman, Morgan (2018-01-01). "A Review of the Familial Alzheimer's Disease Locus PRESENILIN 2 and Its Relationship to PRESENILIN 1". Journal of Alzheimer's Disease. 66 (4): 1323–1339. doi:10.3233/JAD-180656. ISSN 1387-2877. PMID 30412492. S2CID 53247231.
- ^ Tejada-Vera B. (2013). Mortality from Alzheimer's Disease in the United States: Data for 2000 and 2010. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- ^ a b c d e Vardarajan, Badri N.; Zhang, Yalun; Lee, Joseph H.; Cheng, Rong; Bohm, Christopher; Ghani, Mahdi; Reitz, Christiane; Reyes-Dumeyer, Dolly; Shen, Yufeng; Rogaeva, Ekaterina; St George-Hyslop, Peter; Mayeux, Richard (7 November 2014). "Coding mutations in SORL 1 and Alzheimer disease: SORL1 Variants and AD". Annals of Neurology. 77 (2): 215–227. doi:10.1002/ana.24305. PMC 4367199. PMID 25382023.
- ^ Stieger, Bruno (2007-01-01), Enna, S. J.; Bylund, David B. (eds.), "ABC1, ATP Binding Cassette Permease 1", xPharm: The Comprehensive Pharmacology Reference, New York: Elsevier, pp. 1–3, ISBN 978-0-08-055232-3, retrieved 2022-12-03
- ^ a b Dib, Shiraz; Pahnke, Jens; Gosselet, Fabien (27 April 2021). "Role of ABCA7 in Human Health and in Alzheimer's Disease". International Journal of Molecular Sciences. 22 (9): 4603. doi:10.3390/ijms22094603. ISSN 1422-0067. PMC 8124837. PMID 33925691.
- ^ a b c d e Foster, Evangeline M.; Dangla-Valls, Adrià; Lovestone, Simon; Ribe, Elena M.; Buckley, Noel J. (2019). "Clusterin in Alzheimer's Disease: Mechanisms, Genetics, and Lessons From Other Pathologies". Frontiers in Neuroscience. 13: 164. doi:10.3389/fnins.2019.00164. ISSN 1662-453X. PMC 6403191. PMID 30872998.
- ^ Du, Wenjin; Tan, Jiping; Xu, Wei; Chen, Jinwen; Wang, Luning (2016-11-01). "Association between clusterin gene polymorphism rs11136000 and late‑onset Alzheimer's disease susceptibility: A review and meta‑analysis of case‑control studies". Experimental and Therapeutic Medicine. 12 (5): 2915–2927. doi:10.3892/etm.2016.3734. ISSN 1792-0981. PMC 5103725. PMID 27882096.
- ^ a b c d Santiago, Jose A.; Potashkin, Judith A. (2021-02-12). "The Impact of Disease Comorbidities in Alzheimer's Disease". Frontiers in Aging Neuroscience. 13: 631770. doi:10.3389/fnagi.2021.631770. ISSN 1663-4365. PMC 7906983. PMID 33643025.
- ^ a b c Oparil, Suzanne; Acelajado, Maria Czarina; Bakris, George L.; Berlowitz, Dan R.; Cífková, Renata; Dominiczak, Anna F.; Grassi, Guido; Jordan, Jens; Poulter, Neil R.; Rodgers, Anthony; Whelton, Paul K. (2018-03-22). "Hypertension". Nature Reviews. Disease Primers. 4: 18014. doi:10.1038/nrdp.2018.14. ISSN 2056-676X. PMC 6477925. PMID 29565029.
- ^ a b c d e f g Mills, Katherine T; Stefanescu, Andrei; He, Jiang (April 2020). "The global epidemiology of hypertension". Nature Reviews. Nephrology. 16 (4): 223–237. doi:10.1038/s41581-019-0244-2. ISSN 1759-5061. PMC 7998524. PMID 32024986.
- ^ a b c Guzman, Nicolas J. (2012-06-01). "Epidemiology and Management of Hypertension in the Hispanic Population". American Journal of Cardiovascular Drugs. 12 (3): 165–178. doi:10.2165/11631520-000000000-00000. ISSN 1179-187X. PMC 3624012. PMID 22583147.
- ^ a b c Galicia-Garcia, Unai; Benito-Vicente, Asier; Jebari, Shifa; Larrea-Sebal, Asier; Siddiqi, Haziq; Uribe, Kepa B.; Ostolaza, Helena; Martín, César (30 August 2020). "Pathophysiology of Type 2 Diabetes Mellitus". International Journal of Molecular Sciences. 21 (17): 6275. doi:10.3390/ijms21176275. ISSN 1422-0067. PMC 7503727. PMID 32872570.
- ^ a b Olokoba, Abdulfatai B.; Obateru, Olusegun A.; Olokoba, Lateefat B. (July 2012). "Type 2 Diabetes Mellitus: A Review of Current Trends". Oman Medical Journal. 27 (4): 269–273. doi:10.5001/omj.2012.68. ISSN 1999-768X. PMC 3464757. PMID 23071876.
- ^ a b c d e f Avilés-Santa, M. Larissa; Colón-Ramos, Uriyoán; Lindberg, Nangel M.; Mattei, Josiemer; Pasquel, Francisco J.; Pérez, Cynthia M. (2017). "From Sea to Shining Sea and the Great Plains to Patagonia: A Review on Current Knowledge of Diabetes Mellitus in Hispanics/Latinos in the US and Latin America". Frontiers in Endocrinology. 8: 298. doi:10.3389/fendo.2017.00298. ISSN 1664-2392. PMC 5687125. PMID 29176960.
- ^ Umpierrez, Guillermo E; Gonzalez, Amparo; Umpierrez, Denise; Pimentel, Diana (2007-10-01). "Diabetes Mellitus in the Hispanic/Latino Population: An Increasing Health Care Challenge in the United States". The American Journal of the Medical Sciences. 334 (4): 274–282. doi:10.1097/MAJ.0b013e3180a6efe3. ISSN 0002-9629. PMID 18030184.
- ^ Nguyen, Thuy Trang; Ta, Qui Thanh Hoai; Nguyen, Thi Kim Oanh; Nguyen, Thi Thuy Dung; Van Giau, Vo (2020-04-30). "Type 3 Diabetes and Its Role Implications in Alzheimer's Disease". International Journal of Molecular Sciences. 21 (9): 3165. doi:10.3390/ijms21093165. ISSN 1422-0067. PMC 7246646. PMID 32365816.
- ^ Lopez, O. L., Kuller, L. H., & Barnes, L. L. (2022). Alzheimer's Disease in the Hispanic Population: Epidemiology, Risk Factors, and Research Directions. *Neurodegenerative Diseases*, 22(5) 591-602. https://doi.org/10.1159/000522235
- ^ Greenwood, Shannon (2020-08-11). "About One-in-Four U.S. Hispanics Have Heard of Latinx, but Just 3% Use It". Pew Research Center's Hispanic Trends Project. Retrieved 2022-11-15.
- ^ "Marquez-2022
- ^ Gonzalez, H. M., Tarraf, W., Whitfield, K. E., & Vega, W. A. (2022). The Epidemiology of Alzheimer's Disease and Related Dementias in the Hispanic/Latino Population> Implications for Healthy Policy and Practice. * Journal of Alzheimer's Disease*, 87(3), 947-957. https://doi.org/10/3233/JAD-221118
- ^ a b Winston Wong, PharmD (2020-08-17). "Economic Burden of Alzheimer Disease and Managed Care Considerations". Supplements and Featured Publications. Addressing Unmet Needs in Alzheimer Disease: Implications of Delayed Diagnosis and Examining New and Emerging Therapies. 26 (8).
