Health effects of salt
The health effects of salt are the conditions associated with the consumption of either too much or too little salt. Salt is a mineral composed primarily of sodium chloride (NaCl) and is used in food for both preservation and flavor. Sodium ions are needed in small quantities by most living things, as are chlorine ions. Salt is involved in regulating the water content (fluid balance) of the body. Both sodium and chlorine ions are used for electrical signaling in the nervous system, among other biological roles.[1][2]
Salt is usually high in ultra-processed and hyperpalatable foods.[3] In 2020, the World Health Organization (WHO) recommended that adults consume no more than 5 grams (0.18 oz) (just under a teaspoon) of salt per day, an amount providing about 2 grams (0.071 oz) of sodium per day.[4][5] The WHO further recommends that salt intake be adjusted for those aged 2 to 15 years old based on their energy requirements relative to those of adults.[4] High sodium consumption (5 g or more of salt per day) and insufficient potassium intake (less than 3.5 grams (0.12 oz) per day) have been linked to high blood pressure and increased risk of heart disease, stroke, and kidney disease.[6][7]
As an essential nutrient, sodium is involved in numerous cellular and organ functions. Several national health organizations recommend limiting sodium consumption to 2.3 g per day. However, some studies have found that sodium intake that is below 3 g per day (equivalent to about 7.5 g of salt) may increase the risk for cardiovascular disease and early death.[6][8][9] The cardiovascular benefits of reducing salt consumption are similar to reductions in obesity, cholesterol, and tobacco use.[10]
Acute effects
[edit]Hypernatremia (high blood sodium level, above 145 mEq/L) causes thirst, and due to brain cell shrinkage may cause confusion, muscle twitching, or spasms. With severe elevation, seizures and comas may occur.[11][12] Death can be caused by ingestion of large amounts of salt at a time (about 1 g per kg of body weight).[13] Deaths have also been caused by the use of salt solutions as emetics, typically after suspected poisoning.[14]
Hyponatremia, or blood sodium levels below 135 mEq/L, causes brain cells to swell; the symptoms can be subtle and may include altered personality, lethargy, and confusion. In severe cases, when blood sodium falls below 115 mEq/L, stupor, muscle twitching or spasms, seizures, coma, and death can result.[15]
Long-term effects
[edit]Major health organizations and recent reviews state that high consumption of salt increases the risk of several diseases in children and adults.[16][17][18][19]
Excess sodium consumption increases blood pressure.[16][19] Some studies suggest a U-shaped association between salt intake and mortality, with increased mortality associated with both excessively low and excessively high salt intake.[8][9][20] Larger reductions in salt intake lead to larger decreases in blood pressure.[19]
Normotensive overweight/obese patients who were salt restricted for six weeks showed an endothelin 1 (ET-1) decrease of 14% associated with a 45% increase in flow-mediated dilation (FMD).[21] ET-1 has autocrine action on endothelial cells causing the release of nitric oxide.[21] Another study using middle-aged or older adults with moderately elevated blood pressure taking sodium chloride tablets or placebo tablets for a few weeks showed that sodium restriction increased nitric oxide and tetrahydrobiopterin (BH4) resulting in improved FMD without affecting blood pressure.[22] The suppression of endothelium production of nitric oxide is the result of oxidative stress on the vasculature.[23]
Health effects associated with excessive sodium consumption include:
- Stroke and cardiovascular disease.[24]
- High blood pressure: Evidence shows an association between salt intakes and blood pressure among different populations and age ranges in adults.[25] Reduced salt intake also results in a small but statistically significant reduction in blood pressure.[19][26]
- Left ventricular hypertrophy (cardiac enlargement): "Evidence suggests that high salt intake causes left ventricular hypertrophy. This is a strong risk factor for cardiovascular disease, independently of blood pressure effects."[25] "...there is accumulating evidence that high salt intake predicts left ventricular hypertrophy."[27]
- Edema (fluid retention): A decrease in salt intake has been suggested to treat edema.[12][28]
- Kidney disease: Excessive salt (sodium) intake, combined with an inadequate intake of water, can cause hypernatremia. It can exacerbate renal disease.[12] A US expert committee reported in 2013 the common recommendation by several authorities "to reduce daily sodium intake to less than 2,300 milligrams and further reduce intake to 1,500 mg among persons who are 51 years of age and older and those of any age who are African-American or have hypertension, diabetes, or chronic kidney disease", but concluded that there was no health-outcome-based rationale for reducing intake below 2,300 mg, and did not have a recommendation for an upper limit.[29]
A meta-analysis investigated the association between sodium intake and health outcomes, including all-cause mortality and cardiovascular disease (CVD) events.[9] Low sodium intake level was a mean of <115 mmol (2645 mg), usual sodium intake was 115-215 mmol (2645–4945 mg), and a high sodium intake was >215 mmol (4945 mg), concluding: "Both low sodium intakes and high sodium intakes are associated with increased mortality, consistent with a U-shaped association between sodium intake and health outcomes".
Salt-preserved foods
[edit]Possible effects of microplastic contamination
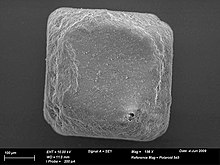
[edit]Microplastic contamination in sea salt has been confirmed in all areas of the world, ranging from zero to 1,674 particles per kilogram.[35] The most common particles are polypropylene, followed by polyethylene and nylon.[36] Microplastic particles per kg sea salt tend to be higher when sourced from Asian countries.[35] Salt sourced from India ranged from 115 to 560 particles/kg.[37] Sea salt sourced from China reported more than 400/kg.[38] Microplastics also accrue in shellfish grown or harvested in regions with microplastic contamination of seawater, and are a significant contributor to human exposure.[39] The extent to which humans are exposed to microplastics in foods and beverages can be assessed via measuring microplastics content in feces, but the health effects, if any, are poorly understood.[40]
Dietary recommendations
[edit]Recommended intakes of salt are usually expressed in terms of sodium intake as an Adequate Intake (AI) and a Tolerable upper intake level (Upper Limit or UL). Salt (as sodium chloride) contains 39.3 percent of sodium by weight.
| Country | Description | Sodium intake mg per day |
Salt intake mg per day |
Authority | Remarks |
|---|---|---|---|---|---|
| United Kingdom | The Reference Nutrient Intake (RNI) defined for a typical adult | RNI: 1600 | RNI: 4000 | Scientific Advisory Committee on Nutrition (SACN) (2003)[41] | However, average adult intake is two and a half times the RNI. SACN states, "The target salt intakes set for adults and children do not represent ideal or optimum consumption levels, but achievable population goals." The Food Safety Authority of Ireland endorses the UK targets.[27] |
| Canada | An Adequate Intake (AI) and Upper Limit (UL) recommended for persons aged 4 years or more. | AI: 1200–1500 UL: 1900–2300 |
AI: 3000–3750 UL: 5500–5750 |
Health Canada (2017)[7] | "Canadians are consuming too much sodium without understanding the risks to their health. Canadians should lower their sodium intakes, as part of maintaining a healthy lifestyle, to reduce the risk of high blood pressure, stroke and heart and kidney disease." (2017)[7] |
| Australia and New Zealand | An Adequate Intake (AI) and an Upper Level of intake (UL) defined for adults | AI: 460–920 UL: 2300 |
AI: 1150–2300 UL: 5750 |
NHMRC (2006)[42] | Not able to define a recommended dietary intake (RDI) |
| United States | An Adequate Intake (AI) and Upper Limit (UL) defined for adults. A different UL defined for the special group comprising people over 51 years of age, African Americans and people with hypertension, diabetes, or chronic kidney disease (regardless of age).[6] | UL: 2300 UL for special group: 1500 |
UL: 5750 UL for special group: 3750 |
Department of Agriculture and Department of Health and Human Services (2010)[43][44] | The Food and Drug Administration itself does not make a recommendation, but refers readers to the dietary guidelines given by this authority.[45] |
| Sweden | An Adequate Intake (AI) and Upper Level of intake (UL) defined for adults | AI: 2000
UL: 2400 |
AI: 5000
UL: 6000 |
Swedish Food Agency (2023)[46] | An excessive intake of sodium increases the blood pressure, which in turn can lead to increased risk of cardiovascular diseases and kidney failure. It is estimated that one forth of the adults in Sweden have high blood pressure, and almost half of all over 65 years of age. The Swedish recommendations are based on the Nordic Nutritional Recommendations (2012).[47] |
| Nordic countries | An Adequate Intake (AI) and Chronic disease risk reduction (CDRR) | UL: 1500
CDRR: 2300 |
UL: 2500
CDRR: 5750 |
The Nordic Nutritional Recommendations (NNR) (2023)[48] | Adverse effects of high intake are high blood pressure and increased mortality.[49][48] |
As of 2009 the average sodium consumption in 33 countries was in the range of 2,700 to 4,900 mg/day. This ranged across many cultures, and together with animal studies, this suggests that sodium intake is tightly controlled by feedback loops in the body. This makes recommendations to reduce sodium consumption below 2,700 mg/day potentially futile.[50] Upon review, an expert committee that was commissioned by the Institute of Medicine and the Centers for Disease Control and Prevention reported that there was no health outcome-based rationale for reducing daily sodium intake levels below 2,300 milligrams, as had been recommended by previous dietary guidelines; the report did not have a recommendation for an upper limit of daily sodium intake.[29][51]
The United States Centers for Disease Control and Prevention (CDC) states that excess sodium can increase blood pressure and the risk for heart disease and stroke in some individuals.[52] Therefore, health authorities recommend limitations on dietary sodium.[53][54][55][56] The United States Department of Health and Human Services recommends that individuals consume no more than 1500–2300 mg of sodium (3750–5750 mg of salt) per day.[52][43]
Although sea salt is sometimes promoted as being healthier than table salt, both forms have the same sodium content.[57]
Labeling
[edit]UK: The Food Standards Agency defines the level of salt in foods as follows: "High is more than 1.5 g salt per 100 g (or 0.6 g sodium). Low is 0.3 g salt or less per 100 g (or 0.1 g sodium). If the amount of salt per 100 g is in between these figures, then that is a medium level of salt." In the UK, foods produced by some supermarkets and manufacturers have 'traffic light' colors on the front of the packet: red (high), amber (medium), or green (low).[58]
USA: The FDA Food Labeling Guide stipulates whether a food can be labeled as "free" "low," or "reduced/less" in respect of sodium. When other health claims are made about a food (e.g., low in fat, calories, etc.), a disclosure statement is required if the food exceeds 480 mg of sodium per 'serving'.[59]
Campaigns
[edit]Australia
[edit]In Australia, the "Drop the Salt! Campaign" aimed to reduce the consumption of salt by Australians to 6g per day over the course of five years ending in 2012.[60]
South Africa
[edit]In 2016, South Africa was the first country to legislate the maximum amount of salt in processed food.[61] The legislation was aimed at addressing the fact that 60% of salt in the diet was contributed to by processed foods, with 65% of all ethnic groups consuming sodium in excess of 6g/day, and 40% of young adults in excess of 9g/day.[62]
United Kingdom
[edit]Consensus Action on Salt and Health (CASH)[63] established in the United Kingdom in 1996, actively campaigns to raise awareness of the negative health effect of high intake of salt. The 2008 focus includes raising awareness of high levels of salt hidden in sweet foods that are marketed towards children.[64] In 2004, Britain's Food Standards Agency started a public health campaign called "Salt – Watch it", which recommends no more than 6 g of salt per day; it features a character called Sid the Slug and was criticised by the Salt Manufacturers Association (SMA).[65] The Advertising Standards Authority did not uphold the SMA complaint in its adjudication.[66] In March 2007, the FSA launched the third phase of their campaign with the slogan "Salt. Is your food full of it?" fronted by comedian Jenny Eclair.[67]
United States
[edit]Federal programs
[edit]Since 2010, as part of the Sodium Reduction in Communities Program (SRCP), the United States Centers for Disease Control and Prevention funded local communities across the United States to implement a variety of policy, systems, and environmental change strategies focused on increasing access to lower sodium in foods in a variety of settings such as hospitals, congregate meal sites, and university settings.[68]
Voluntary initiatives
[edit]In January 2010, New York City launched the National Salt Reduction Initiative (NSRI).[69] It was the only coordinated, voluntary effort to reduce sodium in the United States, an effort supported by the Institute of Medicine as an interim goal in advance of federal action on sodium reduction.
As of 2013, over 90 state and local health authorities and health organizations had signed on as partners of the NSRI. Together, the NSRI partnership encouraged food manufacturers and chain restaurants to voluntarily commit to NSRI sodium reduction targets for 2012 and 2014. The NSRI aimed to reduce sodium in the food supply by 25 percent in five years and reduce population sodium intake by 20 percent in the same time, thereby reducing risk for heart attacks and strokes.[69]
Taxation
[edit]In the United States, taxation of sodium has been proposed as a method of decreasing sodium intake and thereby improving health in countries where typical salt consumption is high.[70] Taking an alternative view, the Salt Institute, a salt industry body based in North America, is active in promoting the use of salt,[71] and questioning or opposing the recommended restrictions on salt intake.[72]
Sweden
[edit]In 1989 the Swedish Food Agency launched the symbol Nyckelhålet[73] (The Green Keyhole). The symbol is a public health campaign that aims to help consumers to find healthier food alternatives, and the requirements for using the symbol differs between food categories. Apart from salt, the requirements include fat content, fat quality, fibre content and sugar. It is voluntary for food manufacturers to apply for the symbol on food items that fulfill the requirements, and the application is usually reviewed by the municipal environment and health protection board. Since June 2009, the symbol is also used in Norway and Denmark.
Dietary reduction
[edit]A low sodium diet reduces the intake of sodium by the careful selection of food. The use of a salt substitute can provide a taste offsetting the perceived blandness of low-salt food; potassium chloride is widely used for this purpose. The World Health Organization (WHO) recommends daily potassium intake of not less than 3,510 mg.[18] Government interventions such as food product reformulation and food procurement policy have the potential to reduce the population salt intake.[74]
Studies found that excessively low sodium intake, below about three grams (3,000 mg) of salt per day, is associated with increased mortality and higher risk for cardiovascular disease.[8][9]
A 2020 Cochrane systematic review[75] concludes that for white people with hypertension, reducing salt intake results in a decrease of about 4 mmHg (about 3.5%) of their blood pressure; for people with normal blood pressure, the decrease was negligible. Weak evidence indicated that these effects might be a little greater in black and Asian people. This review also indicates potential negative side effects on hormones and lipid levels, so that decreasing salt intake is not necessarily recommended for people with normal blood pressure.
In people with chronic kidney disease, including those on dialysis, there is high-certainty evidence that dietary salt restriction may help to lower systolic and diastolic blood pressure, as well as albuminuria.[76] The risk of hypotensive symptoms, such as dizziness, may also increase in some people, with moderate certainty.[76] It is unclear whether this affects the dosage required for anti-hypertensive medications. The effect of salt restriction on extracellular fluid, oedema, and total body weight reduction is also uncertain.[76]
References
[edit]- ^ Caldwell JH, Schaller KL, Lasher RS, Peles E, Levinson SR (May 2000). "Sodium channel Na(v)1.6 is localized at nodes of ranvier, dendrites, and synapses". Proceedings of the National Academy of Sciences of the United States of America. 97 (10): 5616–5620. Bibcode:2000PNAS...97.5616C. doi:10.1073/pnas.090034797. PMC 25877. PMID 10779552.
- ^ Jentsch, Thomas J.; Stein, Valentin; Weinreich, Frank; Zdebik, Anselm A. (2002-04-01). "Molecular Structure and Physiological Function of Chloride Channels". Physiological Reviews. 82 (2): 503–568. doi:10.1152/physrev.00029.2001. ISSN 0031-9333. PMID 11917096.
- ^ Monteiro, Carlos A.; Cannon, Geoffrey; Levy, Renata B; Moubarac, Jean-Claude; Louzada, Maria L. C.; Rauber, Fernanda; Khandpur, Neha; Cediel, Gustavo; Neri, Daniela; Martinez-Steele, Euridice; Baraldi, Larissa G.; Jaime, Patricia C. (2019). "Ultra-processed foods: what they are and how to identify them". Public Health Nutrition. 22 (5): 936–941. doi:10.1017/S1368980018003762. ISSN 1368-9800. PMC 10260459. PMID 30744710.
- ^ a b "Salt reduction: fact sheet". World Health Organization. 29 April 2020. Retrieved 20 November 2020.
- ^ "Sodium: How to tame your salt habit". Mayo Clinic. 29 June 2019. Retrieved 20 November 2020.
- ^ a b c "Too much and too little salt is associated with increased heart risks". CardioSmart, American College of Cardiology. 24 July 2016. Retrieved 20 November 2020.
- ^ a b c "Sodium in Canada". Government of Canada. 1 March 2017. Retrieved 20 November 2020.
- ^ a b c Mente A, O'Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, et al. (July 2016). "Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies". Lancet. 388 (10043): 465–475. doi:10.1016/S0140-6736(16)30467-6. hdl:10379/16625. PMID 27216139. S2CID 44581906.
- ^ a b c d Graudal N, Jürgens G, Baslund B, Alderman MH (September 2014). "Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis". American Journal of Hypertension. 27 (9): 1129–1137. doi:10.1093/ajh/hpu028. PMID 24651634.
- ^ Delahaye F (2013). "Should we eat less salt?". Archives of Cardiovascular Diseases. 106 (5): 324–332. doi:10.1016/j.acvd.2013.01.003. PMID 23769406.
- ^ Lewis JL (March 2013). "Hypernatremia". Merck Manual of Diagnosis and Therapy. Medical Library Association. Retrieved 25 December 2015.
- ^ a b c "Better Health Channel: Salt". Department of Health & Human Services, State Government of Victoria, Australia. May 2014.
- ^ "Safety data for sodium chloride". The Physical and Theoretical Chemistry Laboratory of Oxford University. 18 November 2005. Archived from the original on 2 December 2011. Retrieved 7 July 2011.
- ^ Türk EE, Schulz F, Koops E, Gehl A, Tsokos M (January 2005). "Fatal hypernatremia after using salt as an emetic--report of three autopsy cases". Legal Medicine. 7 (1): 47–50. doi:10.1016/j.legalmed.2004.06.005. PMID 15556015. Archived from the original on 2 February 2017.
- ^ Lewis III JL (May 2009). "Hyponatremia". Merck Manual of Diagnosis and Therapy. Archived from the original on 2011-01-11. Retrieved 2016-06-08.
- ^ a b "Sodium, potassium and health". Salt. US Centers for Disease Control and Prevention. 23 August 2022. Retrieved 10 May 2023.
- ^ "EFSA provides advice on adverse effects of sodium". European Food Safety Authority. 22 June 2005. Retrieved 10 May 2023.
- ^ a b "WHO issues new guidance on dietary salt and potassium". World Health Organization. 31 January 2013. Archived from the original on February 3, 2013.
- ^ a b c d He FJ, Li J, Macgregor GA (April 2013). "Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials". BMJ. 346 (apr03 3): f1325. doi:10.1136/bmj.f1325. PMID 23558162.
- ^ Asayama K, Stolarz-Skrzypek K, Persu A, Staessen JA (September 2014). "Systematic review of health outcomes in relation to salt intake highlights the widening divide between guidelines and the evidence" (PDF). American Journal of Hypertension. 27 (9): 1138–1142. doi:10.1093/ajh/hpu126. PMID 25122867.
- ^ a b Dickinson KM, Clifton PM, Keogh JB (2014). "A reduction of 3 g/day from a usual 9 g/day salt diet improves endothelial function and decreases endothelin-1 in a randomised cross_over study in normotensive overweight and obese subjects". Atherosclerosis. 233 (1): 32–38. doi:10.1016/j.atherosclerosis.2013.11.078. PMID 24529119.
- ^ Jablonski KL, Racine ML, Seals DR (2013). "Dietary sodium restriction reverses vascular endothelial dysfunction in middle-aged/older adults with moderately elevated systolic blood pressure". Journal of the American College of Cardiology. 61 (3): 335–343. doi:10.1016/j.jacc.2012.09.010. PMC 3549053. PMID 23141486.
- ^ Greaney JL, DuPont JJ, Farquhar WS (2012). "Dietary sodium loading impairs microvascular function independent of blood pressure in humans: role of oxidative stress". The Journal of Physiology. 590 (21): 5519–5528. doi:10.1113/jphysiol.2012.236992. PMC 3515835. PMID 22907057.
- ^ Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP (November 2009). "Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies". BMJ. 339: b4567. doi:10.1136/bmj.b4567. PMC 2782060. PMID 19934192.
- ^ a b "Salt and Health" (PDF). Scientific Advisory Committee on Nutrition (SACN). p. 3. Archived from the original (PDF) on 11 February 2014.
- ^ Hooper L, Bartlett C, Davey SG, Ebrahim S (26 January 2004). "Advice to reduce dietary salt for prevention of cardiovascular disease" (PDF). The Cochrane Database of Systematic Reviews. 2009 (1): CD003656. doi:10.1002/14651858.CD003656.pub2. PMID 14974027.
- ^ a b "Salt and Health: Review of the Scientific Evidence and Recommendations for Public Policy in Ireland" (PDF). Food Safety Authority of Ireland. p. 12. Archived from the original (PDF) on 2021-04-13. Retrieved 2021-01-16.
- ^ "Fluid retention". Australia: Better Health Channel. Australia, Victoria. Archived from the original on 24 March 2015.
- ^ a b Strom BL, Yaktine AL, Oria M, et al. (Committee on the Consequences of Sodium Reduction in Populations) (2013). Sodium Intake in Populations: Assessment of Evidence (PDF). Washington, DC: National Academies Press; Food and Nutrition Board; Board on Population Health and Public Health Practice; Institute of Medicine. doi:10.17226/18311. ISBN 978-0-309-28295-6. PMID 24851297. Archived from the original (PDF) on 2 February 2017.
- ^ "Diet, Nutrition, Physical Activity and Cancer: A Global Perspective". wcrf.org. Retrieved 14 February 2023.
- ^ "Preservation and processing of foods and cancer risk". wcrf.org. Retrieved 14 February 2023.
- ^ "Stomach Cancer Risk Factors". cancer.org. Retrieved 14 February 2023.
- ^ He, Feng J.; Li, Jiafu; Macgregor, Graham A. (2013-04-03). "Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials". BMJ (Clinical Research Ed.). 346: f1325. doi:10.1136/bmj.f1325. ISSN 1756-1833. PMID 23558162.
- ^ Wang, Yi-Jie; Yeh, Tzu-Lin; Shih, Ming-Chieh; Tu, Yu-Kang; Chien, Kuo-Liong (2020-09-25). "Dietary Sodium Intake and Risk of Cardiovascular Disease: A Systematic Review and Dose-Response Meta-Analysis". Nutrients. 12 (10): 2934. doi:10.3390/nu12102934. ISSN 2072-6643. PMC 7601012. PMID 32992705.
- ^ a b Kim JS, Lee HJ, Kim SK, Kim HJ (November 2018). "Global Pattern of Microplastics (MPs) in Commercial Food-Grade Salts: Sea Salt as an Indicator of Seawater MP Pollution". Environmental Science & Technology. 52 (21): 12819–12828. Bibcode:2018EnST...5212819K. doi:10.1021/acs.est.8b04180. PMID 30285421. S2CID 206582726.
- ^ Selvam S, Manisha A, Venkatramanan S, Chung SY, Paramasivam CR, Singaraja C (January 2020). "Microplastic presence in commercial marine sea salts: A baseline study along Tuticorin Coastal salt pan stations, Gulf of Mannar, South India". Marine Pollution Bulletin. 150: 110675. Bibcode:2020MarPB.15010675S. doi:10.1016/j.marpolbul.2019.110675. PMID 31669711. S2CID 204966981.
- ^ Vidyasakar A, Krishnakumar S, Kumar KS, Neelavannan K, Anbalagan S, Kasilingam K, et al. (October 2021). "Microplastic contamination in edible sea salt from the largest salt-producing states of India". Marine Pollution Bulletin. 171: 112728. Bibcode:2021MarPB.17112728V. doi:10.1016/j.marpolbul.2021.112728. PMID 34303058.
- ^ Feng D, Yuan H, Tang J, Cai X, Yang B (December 2021). "Preliminary investigation of microplastics in the production process of sea salt sourced from the Bohai Sea, China, using an optimised and consistent approach". Food Additives & Contaminants. Part A, Chemistry, Analysis, Control, Exposure & Risk Assessment. 38 (12): 2151–2164. doi:10.1080/19440049.2021.1956691. PMID 34372756. S2CID 236967839.
- ^ Van Cauwenberghe L, Janssen CR (October 2014). "Microplastics in bivalves cultured for human consumption". Environmental Pollution. 193: 65–70. doi:10.1016/j.envpol.2014.06.010. PMID 25005888. S2CID 6939614.
- ^ Cho YM, Choi KH (March 2021). "The current status of studies of human exposure assessment of microplastics and their health effects: a rapid systematic review". Environmental Analysis, Health and Toxicology. 36 (1): e2021004–e2021000. doi:10.5620/eaht.2021004. PMC 8207003. PMID 33730791.
- ^ "Salt and Health". Scientific Advisory Committee on Nutrition (SACN). Government of the United Kingdom.
- ^ "Reference Nutrient Values, Sodium". National Health and Medical Research Council (NHMRC). Australian Government. Archived from the original on 29 September 2009.
- ^ a b "Dietary Guidelines for Americans 2010" (PDF). US Department of Agriculture and US Department of Health and Human Services. Archived from the original (PDF) on 5 October 2018. Retrieved 14 February 2015.
- ^ Zied E (31 January 2011). "New U.S. Dietary Guidelines Focus on Salt Reduction". U.S. News & World Report.
- ^ Greeley. "A Pinch of Controversy Shakes Up Dietary Salt". U.S. Food and Drug Administration. Archived from the original on 2009-05-12.
- ^ "Salt - råd". www.livsmedelsverket.se (in Swedish). Retrieved 2023-09-25.
- ^ Nordic Council Of Ministers, Nordic Council of Ministers (2014-03-11). "Nordic Nutrition Recommendations 2012" (PDF). www.norden.org. 5 (11): 1–3. doi:10.6027/Nord2014-002. Retrieved 2023-09-25.
- ^ a b "NORDIC NUTRITION RECOMMENDATIONS 2023 / INTEGRATING ENVIRONMENTAL ASPECTS". pub.norden.org. Retrieved 2023-09-25.
- ^ "NORDIC NUTRITION RECOMMENDATIONS 2023 / INTEGRATING ENVIRONMENTAL ASPECTS". pub.norden.org. Retrieved 2023-09-25.
- ^ McCarron DA, Geerling JC, Kazaks AG, Stern JS (November 2009). "Can dietary sodium intake be modified by public policy?". Clinical Journal of the American Society of Nephrology. 4 (11): 1878–1882. doi:10.2215/CJN.04660709. PMID 19833911.
- ^ Kolata G (14 May 2013). "No Benefit Seen in Sharp Limits on Salt in Diet". New York Times. Retrieved 3 June 2013.
- ^ a b "Salt". US Centers for Disease Control, Department of Health and Human Services, Atlanta, GA. 1 June 2016. Retrieved 9 June 2016.
- ^ "American Heart Association 2010 Dietary Guidelines" (PDF). 2010 Dietary Guidelines. American Heart Association. 23 January 2009. Archived from the original (PDF) on 24 January 2011. Retrieved 16 May 2010.
- ^ "Nutrient Reference Values for Australia and New Zealand – Sodium". Nutrient Reference Values for Australia and New Zealand. Australian Government National Health and Medical Research Council/ New Zealand Ministry of Health. Archived from the original on 29 September 2009. Retrieved 16 May 2010.
- ^ "Sodium Chloride". Eat Well, Be Well. UK Government Food Standards Agency. Retrieved 16 May 2010.
- ^ "Health Canada, Healthy Living, Sodium". Healthy Living. Health Canada. 2008. Archived from the original on 4 March 2010. Retrieved 16 May 2010.
- ^ Zeratsky K (27 August 2009). "Is sea salt better for your health than table salt?". Mayo Foundation for Medical Education and Research. Retrieved 22 April 2011.
- ^ "Understanding labels". Salt.gov.uk. 6 November 2009. Archived from the original on 31 March 2007. Retrieved 7 July 2011.
- ^ "A Food Labeling Guide—Appendix A". U.S. Food and Drug Administration. Archived from the original on 2006-03-21.
- ^ "Drop the Salt! Campaign". Australian Division on World Action on Salt & Health. Retrieved 7 March 2013.
- ^ Charlton K, Ware LJ, Baumgartner J, Cockeran M, Schutte AE, Naidoo N, Kowal P (March 2018). "How will South Africa's mandatory salt reduction policy affect its salt iodisation programme? A cross-sectional analysis from the WHO-SAGE Wave 2 Salt & Tobacco study". BMJ Open. 8 (3): e020404. doi:10.1136/bmjopen-2017-020404. PMC 5884349. PMID 29602855.
- ^ Webster J, Crickmore C, Charlton K, Steyn K, Wentzel-Viljoen E, Naidoo P (December 2016). "South Africa's salt reduction strategy: Are we on track, and what lies ahead?". South African Medical Journal = Suid-Afrikaanse Tydskrif vir Geneeskunde. 107 (1): 20–21. doi:10.7196/SAMJ.2017.v107i1.12120 (inactive 2024-11-10). hdl:10019.1/104738. PMID 28112084.
{{cite journal}}: CS1 maint: DOI inactive as of November 2024 (link) - ^ "CASH: Consensus Action on Salt and Health". Wolfson Institute of Population Health. Queen Mary University of London. Retrieved 7 March 2013.
- ^ Rebecca S (28 January 2008). "Child health fears over high salt levels in sweet foods". The Guardian. London. Retrieved 23 May 2010.
- ^ "New salt campaign under attack". Salt Manufacturers Association press release. Archived from the original on 2010-03-25.
- ^ Advertising Standards Authority "Broadcast Advertising Adjudications" (PDF). 20 April 2005. Archived from the original (PDF) on 2009-03-26.
- ^ "Salt TV ads". Salt.gov.uk. 6 November 2009. Archived from the original on 24 January 2009. Retrieved 7 July 2011.
- ^ "Sodium Reduction in Communities Program". United States Centers for Disease Control and Prevention. 13 October 2020. Retrieved 28 June 2021.
- ^ a b "Sodium initiatives". National Salt Reduction Initiative, City of New York. 2016.
- ^ Wilson N (October 2004). "Salt tax could reduce population's salt intake". BMJ. 329 (7471): 918. doi:10.1136/bmj.329.7471.918-c. PMC 523164. PMID 15485985.
- ^ "About the Salt Institute". Salt Institute. 2009. Retrieved 5 December 2010.
- ^ "Food salt & health". Salt Institute. 2009. Retrieved 5 December 2010.
- ^ "Nyckelhålet". www.livsmedelsverket.se (in Swedish). Retrieved 2024-06-05.
- ^ McLaren L, Sumar N, Barberio AM, Trieu K, Lorenzetti DL, Tarasuk V, et al. (September 2016). "Population-level interventions in government jurisdictions for dietary sodium reduction". The Cochrane Database of Systematic Reviews. 9 (9): CD010166. doi:10.1002/14651858.CD010166.pub2. PMC 6457806. PMID 27633834.
- ^ Graudal NA, Hubeck-Graudal T, Jurgens G (December 2020). "Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride". The Cochrane Database of Systematic Reviews. 12 (12): CD004022. doi:10.1002/14651858.CD004022.pub5. PMC 8094404. PMID 33314019.
- ^ a b c McMahon EJ, Campbell KL, Bauer JD, Mudge DW, Kelly JT, et al. (Cochrane Kidney and Transplant Group) (June 2021). "Altered dietary salt intake for people with chronic kidney disease". The Cochrane Database of Systematic Reviews. 2021 (6): CD010070. doi:10.1002/14651858.CD010070.pub3. PMC 8222708. PMID 34164803.
Further reading
[edit]- Organization, World Health (2012). Guideline: sodium intake for adults and children. World Health Organization. ISBN 978-92-4-150483-6. Retrieved 10 May 2023.
- Neravetla SR, Neravetla SR (2012). Salt Kills. Springfield, OH: Health Now Books, LLC. ISBN 978-1938009006.
- Committee on Strategies to Reduce Sodium Intake (2010). Henry JE, Taylor CL (eds.). Strategies to Reduce Sodium Intake in the United States. Washington, DC: The National Academies Press. doi:10.17226/12818. ISBN 978-0-309-14805-4. PMID 21210559.
- Panel on Dietary Reference Intakes for Electrolytes and Water (2005). Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC: The National Academies Press. doi:10.17226/10925. ISBN 978-0-309-09158-9.
